Abstract
The proliferation of anti-vaccination arguments is a threat to the success of many immunization programmes. Effective rebuttal of contrarian arguments requires an approach that goes beyond addressing flaws in the arguments, by also considering the attitude roots—that is, the underlying psychological attributes driving a person’s belief—of opposition to vaccines. Here, through a pre-registered systematic literature review of 152 scientific articles and thematic analysis of anti-vaccination arguments, we developed a hierarchical taxonomy that relates common arguments and themes to 11 attitude roots that explain why an individual might express opposition to vaccination. We further validated our taxonomy on coronavirus disease 2019 anti-vaccination misinformation, through a combination of human coding and machine learning using natural language processing algorithms. Overall, the taxonomy serves as a theoretical framework to link expressed opposition of vaccines to their underlying psychological processes. This enables future work to develop targeted rebuttals and other interventions that address the underlying motives of anti-vaccination arguments.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
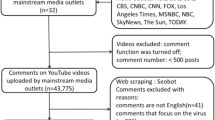
Data availability
All datasets used in this article are publicly available at https://osf.io/e4yp6/. The dataset used in Study 1 is accessible at https://osf.io/xu2cz (retrieved from Scopus, Web of Science, PubMed, PsycInfo, PsyArXiv, ArXiv and MedrXiv). The dataset used in Study 2 is accessible at https://osf.io/d839n (retrieved from https://covid19misinfo.org portal)
Code availability
All source code used in this article is publicly available at https://osf.io/e4yp6/.
References
Greenwood, B. The contribution of vaccination to global health: past, present and future. Philos. Trans. R. Soc. B 369, 20130433 (2014).
Ten Threats to Global Health in 2019 (World Health Organization, 2019).
MacDonald, N. E. et al. Vaccine hesitancy: definition, scope and determinants. Vaccine 33, 4161–4164 (2015).
Ball, P. & Maxmen, A. The epic battle against coronavirus misinformation and conspiracy theories. Nature 581, 371–375 (2020).
Karlsson, L. C. et al. Fearing the disease or the vaccine: the case of COVID-19. Pers. Individ. Dif. 172, 110590 (2021).
Gagneur, A. et al. A postpartum vaccination promotion intervention using motivational interviewing techniques improves short-term vaccine coverage: PromoVac study. BMC Public Health 18, 1–8 (2018).
Reiter, P. L., Gilkey, M. B. & Brewer, N. T. HPV vaccination among adolescent males: results from the national immunization survey-teen. Vaccine 31, 2816–2821 (2013).
Wiley, K. E. & Leask, J. Respiratory vaccine uptake during pregnancy. Lancet Respir. Med. 1, 9–11 (2013).
Brewer, N. T., Chapman, G. B., Rothman, A. J., Leask, J. & Kempe, A. Increasing vaccination: putting psychological science into action. Psychol. Sci. Public Interest 18, 149–207 (2017).
Immunization Agenda 2030: A Global Strategy to Leave No One Behind (World Health Organization, 2020).
European Immunization Agenda 2030: Draft for the Seventy-First Regional Committee for Europe (World Health Organization, 2021).
Center for Countering Digital Hate. Pandemic profiteers: the business of anti-vaxx https://www.counterhate.com/pandemicprofiteers (2021).
Smith, N. & Graham, T. Mapping the anti-vaccination movement on Facebook. Inf. Commun. Soc. 22, 1310–1327 (2019).
Peretti-Watel, P. et al. ‘I think I made the right decision… I hope I’m not wrong’. Vaccine hesitancy, commitment and trust among parents of young children. Sociol. Health Illn. 41, 1192–1206 (2019).
Hornsey, M. J. & Fielding, K. S. Attitude roots and jiu jitsu persuasion: understanding and overcoming the motivated rejection of science. Am. Psychol. 72, 459 (2017).
Ajzen, I. & Fishbein, M. The influence of attitudes on behavior. In The Handbook of Attitudes (eds Albarracín, D., Johnson, M. & Zanna, P.) 173–221 (Lawrence Erlbaum Associates Publishers, 2005).
Glasman, L. R. & Albarracín, D. Forming attitudes that predict future behavior: a meta-analysis of the attitude-behavior relation. Psychol. Bull. 132, 778 (2006).
Festinger, L. A Theory of Cognitive Dissonance vol. 2 (Stanford Univ. Press, 1957).
Bleser, W. K., Elewonibi, B. R., Miranda, P. Y. & BeLue, R. Complementary and alternative medicine and influenza vaccine uptake in us children. Pediatrics 138, e20154664 (2016).
Moran, M. B., Lucas, M., Everhart, K., Morgan, A. & Prickett, E. What makes anti-vaccine websites persuasive? A content analysis of techniques used by anti-vaccine websites to engender anti-vaccine sentiment. J. Commun. Healthc. 9, 151–163 (2016).
Browne, M. Epistemic divides and ontological confusions: the psychology of vaccine scepticism. Hum. Vaccin. Immunother. 14, 2540–2542 (2018).
Lewandowsky, S., Woike, J. K. & Oberauer, K. Genesis or evolution of gender differences? Worldview-based dilemmas in the processing of scientific information. J. Cogn. 3, 9 (2020).
Kata, A. A postmodern Pandora’s box: anti-vaccination misinformation on the internet. Vaccine 28, 1709–1716 (2010).
Hughes, B. et al. Development of a codebook of online anti-vaccination rhetoric to manage COVID-19 vaccine misinformation. Int. J. Environ. Res. Public Health 18, 7556 (2021).
Wawrzuta, D., Jaworski, M., Gotlib, J. & Panczyk, M. What arguments against COVID-19 vaccines run on facebook in poland: content analysis of comments. Vaccines 9, 481 (2021).
Fournet, N. et al. Under-vaccinated groups in Europe and their beliefs, attitudes and reasons for non-vaccination: two systematic reviews. BMC Public Health 18, 1–17 (2018).
Coan, T. G., Boussalis, C., Cook, J. & Nanko, M. O. Computer-assisted classification of contrarian claims about climate change. Sci. Rep. 11, 22320 (2021).
Lewandowsky, S. & Cook, J. The Conspiracy Theory Handbook (John Cook, Center for Climate Change Communication, George Mason Univ., 2020).
Walton, D. N. What is reasoning? What is an argument? J. Philos. 87, 399–419 (1990).
Van Eemeren, F. H. & Grootendorst, R. Speech Acts in Argumentative Discussions: A Theoretical Model for the Analysis of Discussions Directed towards Solving Conflicts of Opinion vol. 1 (Walter de Gruyter, 2010).
Pinto, R. C. The relation of argument to inference. In Argument, Inference and Dialectic (ed Pinto, R. C.) 32–45 (Springer, 2001).
Hitchcock, D. Informal logic and the concept of argument. In Philosophy of Logic (ed. Jacquette, D.) 101–129 (Elsevier, 2007).
Braun, V. & Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 3, 77–101 (2006).
Hornsey, M. J. Why facts are not enough: understanding and managing the motivated rejection of science. Curr. Dir. Psychol. Sci. 29, 583–591 (2020).
Aaronovitch, D. Voodoo Histories: How Conspiracy Theory Has Shaped Modern History (Random House, 2010).
Goreis, A. & Voracek, M. A systematic review and meta-analysis of psychological research on conspiracy beliefs: field characteristics, measurement instruments, and associations with personality traits. Front. Psychol. 10, 205 (2019).
Goldberg, Z. J. & Richey, S. Anti-vaccination beliefs and unrelated conspiracy theories. World Aff. 183, 105–124 (2020).
Hornsey, M. J., Harris, E. A. & Fielding, K. S. The psychological roots of anti-vaccination attitudes: a 24-nation investigation. Health Psychol. 37, 307 (2018).
Jolley, D. & Douglas, K. M. The effects of anti-vaccine conspiracy theories on vaccination intentions. PLoS ONE 9, e89177 (2014).
Lewandowsky, S., Gignac, G. E. & Oberauer, K. The role of conspiracist ideation and worldviews in predicting rejection of science. PLoS ONE 8, e75637 (2013).
Shapiro, G. K., Holding, A., Perez, S., Amsel, R. & Rosberger, Z. Validation of the vaccine conspiracy beliefs scale. Papillomavirus Res. 2, 167–172 (2016).
Soveri, A., Karlsson, L. C., Antfolk, J., Lindfelt, M. & Lewandowsky, S. Unwillingness to engage in behaviors that protect against COVID-19: the role of conspiracy beliefs, trust, and endorsement of complementary and alternative medicine. BMC Public Health 21, 1–12 (2021).
Lewandowsky, S. et al. When science becomes embroiled in conflict: recognizing the public’s need for debate while combating conspiracies and misinformation. Ann. Am. Acad. Polit. Soc. Sci. 700, 26–40 (2022).
Hornsey, M. J., Lobera, J. & Díaz-Catalán, C. Vaccine hesitancy is strongly associated with distrust of conventional medicine, and only weakly associated with trust in alternative medicine. Soc. Sci. Med. 255, 113019 (2020).
Lee, C., Whetten, K., Omer, S., Pan, W. & Salmon, D. Hurdles to herd immunity: distrust of government and vaccine refusal in the US, 2002–2003. Vaccine 34, 3972–3978 (2016).
Salmon, D. A. et al. Factors associated with refusal of childhood vaccines among parents of school-aged children: a case–control study. Arch. Pediatr. Adolesc. Med. 159, 470–476 (2005).
Tram, K. H. et al. Deliberation, dissent, and distrust: understanding distinct drivers of coronavirus disease 2019 vaccine hesitancy in the United States. Clin. Infect. Dis. 74, 1429–1441 (2022).
Pennycook, G., Cheyne, J. A., Seli, P., Koehler, D. J. & Fugelsang, J. A. Analytic cognitive style predicts religious and paranormal belief. Cognition 123, 335–346 (2012).
Svedholm, A. M. & Lindeman, M. The separate roles of the reflective mind and involuntary inhibitory control in gatekeeping paranormal beliefs and the underlying intuitive confusions. Br. J. Psychol. 104, 303–319 (2013).
Fasce, A. & Picó, A. Science as a vaccine: the relation between scientific literacy and unwarranted beliefs. Sci. Educ. 28, 109–125 (2019).
Hart, J. & Graether, M. Something’s going on here: psychological predictors of belief in conspiracy theories. J. Individ. Dif. 39, 229–237 (2018).
Torres, M. N., Barberia, I. & Rodríguez-Ferreiro, J. Causal illusion as a cognitive basis of pseudoscientific beliefs. Br. J. Psychol. 111, 840–852 (2020).
Pierre, J. M. Mistrust and misinformation: a two-component, socio-epistemic model of belief in conspiracy theories. J. Soc. Polit. Psychol. 8, 617–641 (2020).
van Prooijen, J.-W. An existential threat model of conspiracy theories. Eur. Psychol. 25, 16–25 (2019).
Browne, M., Thomson, P., Rockloff, M. J. & Pennycook, G. Going against the herd: psychological and cultural factors underlying the ‘vaccination confidence gap’. PLoS ONE 10, e0132562 (2015).
Kennedy, J. Populist politics and vaccine hesitancy in western europe: an analysis of national-level data. Eur. J. Public Health 29, 512–516 (2019).
Lewandowsky, S. & Oberauer, K. Worldview-motivated rejection of science and the norms of science. Cognition 215, 104820 (2021).
Whitehead, A. L. & Perry, S. L. How culture wars delay herd immunity: Christian nationalism and anti-vaccine attitudes. Socius 6, 2378023120977727 (2020).
Motta, M. Republicans, not Democrats, are more likely to endorse anti-vaccine misinformation. Am. Polit. Res. 49, 428–438 (2021).
Rekker, R. The nature and origins of political polarization over science. Public Underst. Sci. 30, 352–368 (2021).
Grabenstein, J. D. What the world’s religions teach, applied to vaccines and immune globulins. Vaccine 31, 2011–2023 (2013).
Eriksson, K. & Vartanova, I. Vaccine confidence is higher in more religious countries. Hum. Vaccin. Immunother. 18, 1–3 (2022).
Barskey, A. E. et al. Mumps outbreak in Orthodox Jewish communities in the united states. N. Engl. J. Med. 367, 1704–1713 (2012).
Bodson, J., Wilson, A., Warner, E. L. & Kepka, D. Religion and HPV vaccine-related awareness, knowledge, and receipt among insured women aged 18-26 in utah. PLoS ONE 12, e0183725 (2017).
Hanratty, B. et al. UK measles outbreak in non-immune anthroposophic communities: the implications for the elimination of measles from Europe. Epidemiol. Infect. 125, 377–383 (2000).
Amin, A. B. et al. Association of moral values with vaccine hesitancy. Nat. Hum. Behav. 1, 873–880 (2017).
Rossen, I., Hurlstone, M. J., Dunlop, P. D. & Lawrence, C. Accepters, fence sitters, or rejecters: moral profiles of vaccination attitudes. Soc. Sci. Med. 224, 23–27 (2019).
Daniel Freeman, D. et al. Injection fears and COVID-19 vaccine hesitancy. Psychol. Med. 53, 1185–1195 (2021).
Ajzen, I. The theory of planned behavior. Organ. Behav. Hum. Decis. Process. 50, 179–211 (1991).
Green, J., Edgerton, J., Naftel, D., Shoub, K. & Cranmer, S. J. Elusive consensus: polarization in elite communication on the COVID-19 pandemic. Sci. Adv. 6, eabc2717 (2020).
Betsch, C. et al. Beyond confidence: development of a measure assessing the 5C psychological antecedents of vaccination. PLoS ONE 13, e0208601 (2018).
Caserotti, M. et al. Associations of COVID-19 risk perception with vaccine hesitancy over time for Italian residents. Soc. Sci. Med. 272, 113688 (2021).
González-Block, M. Á. et al. Influenza vaccination hesitancy in five countries of South America. Confidence, complacency and convenience as determinants of immunization rates. PLoS ONE 15, e0243833 (2020).
Kwok, K. O. et al. Influenza vaccine uptake, COVID-19 vaccination intention and vaccine hesitancy among nurses: a survey. Int. J. Nurs. Stud. 114, 103854 (2021).
Attwell, K., Smith, D. T. & Ward, P. R. ‘If your child’s vaccinated, why do you care about mine?’ Rhetoric, responsibility, power and vaccine rejection. J. Sociol. 57, 268–285 (2021).
Quadri-Sheriff, M. et al. The role of herd immunity in parents’ decision to vaccinate children: a systematic review. Pediatrics 130, 522–530 (2012).
Betsch, C., Böhm, R. & Korn, L. Inviting free-riders or appealing to prosocial behavior? Game-theoretical reflections on communicating herd immunity in vaccine advocacy. Health Psychol. 32, 978 (2013).
Hershey, J. C., Asch, D. A., Thumasathit, T., Meszaros, J. & Waters, V. V. The roles of altruism, free riding, and bandwagoning in vaccination decisions. Organ. Behav. Hum. Decis. Process. 59, 177–187 (1994).
Ibuka, Y., Li, M., Vietri, J., Chapman, G. B. & Galvani, A. P. Free-riding behavior in vaccination decisions: an experimental study. PLoS ONE 9, e87164 (2014).
Gidengil, C., Chen, C., Parker, A. M., Nowak, S. & Matthews, L. Beliefs around childhood vaccines in the United States: a systematic review. Vaccine 37, 6793–6802 (2019).
Meszaros, J. R. et al. Cognitive processes and the decisions of some parents to forego pertussis vaccination for their children. J. Clin. Epidemiol. 49, 697–703 (1996).
Benin, A. L., Wisler-Scher, D. J., Colson, E., Shapiro, E. D. & Holmboe, E. S. Qualitative analysis of mothers’ decision-making about vaccines for infants: the importance of trust. Pediatrics 117, 1532–1541 (2006).
Hatoková, M., Masaryk, R. & Túnyiová, M. How Slovak mothers view child vaccination: focus group analysis. Ceskoslovenska Psychol. 62 (2018).
Bryden, G. M., Browne, M., Rockloff, M. & Unsworth, C. The privilege paradox: geographic areas with highest socio-economic advantage have the lowest rates of vaccination. Vaccine 37, 4525–4532 (2019).
Pereira, J. A. et al. Contagious comments: what was the online buzz about the 2011 Quebec measles outbreak? PLoS ONE 8, e64072 (2013).
Boghossian, P. Fear of Knowledge: Against Relativism and Constructivism (Clarendon Press, 2007).
Kusch, M. Relativism in the Philosophy of Science (Cambridge Univ. Press, 2021).
Reich, J. A. Neoliberal mothering and vaccine refusal: imagined gated communities and the privilege of choice. Gend. Soc. 28, 679–704 (2014).
Schindler, J., Schindler, S. & Pfattheicher, S. The role of intuition in vaccination attitudes. J. Health Psychol. 26, 2950–2957 (2021).
Ten Kate, J., De Koster, W. & Van der Waal, J. "Following your gut” or “questioning the scientific evidence”: understanding vaccine skepticism among more-educated dutch parents. J. Health Soc. Behav. 62, 85–99 (2021).
Tomljenovic, H., Bubic, A. & Erceg, N. It just doesn’t feel right—the relevance of emotions and intuition for parental vaccine conspiracy beliefs and vaccination uptake. Psychol. Health 35, 538–554 (2020).
Finkelstein, S. R. et al. Psychological reactance impacts ratings of pediatrician vaccine-related communication quality, perceived vaccine safety, and vaccination priority among us parents. Hum. Vaccin. Immunother. 16, 1024–1029 (2020).
Soveri, A. et al. Trait reactance and trust in doctors as predictors of vaccination behavior, vaccine attitudes, and use of complementary and alternative medicine in parents of young children. PLoS ONE 15, e0236527 (2020).
Sprengholz, P., Felgendreff, L., Böhm, R. & Betsch, C. Vaccination policy reactance: predictors, consequences, and countermeasures. J. Health Psychol. 27, 1394–1407 (2022).
Akande, A., Ahmad, M. & Majid, U. A qualitative meta-synthesis on how autonomy promotes vaccine rejection or delay among health care providers. Health Promot. Int. 37, daab099 (2022).
Crescitelli, M. D. et al. A meta-synthesis study of the key elements involved in childhood vaccine hesitancy. Public Health 180, 38–45 (2020).
Garcia, D., Goel, M., Agrawal, A. K. & Kumaraguru, P. Collective aspects of privacy in the twitter social network. EPJ Data Sci. 7, 1–13 (2018).
Li, Y., Hills, T. & Hertwig, R. A brief history of risk. Cognition 203, 104344 (2020).
Reimers, N. & Gurevych, I. Sentence-BERT: Sentence Embeddings using Siamese BERT-Networks. In Proc. 2019 Conference on Empirical Methods in Natural Language Processing and the 9th International Joint Conference on Natural Language Processing (EMNLP-IJCNLP) (eds Huang, R. & Padó, S.) 3982–3992 (Association for Computational Linguistics, 2019).
McInnes, L., Healy, J. & Melville, J. UMAP: Uniform Manifold Approximation and Projection for dimension reduction. Preprint at arXiv https://doi.org/10.48550/arXiv.1802.03426 (2018).
Nowell, L. S., Norris, J. M., White, D. E. & Moules, N. J. Thematic analysis: striving to meet the trustworthiness criteria. Int. J. Qual. Methods 16, 1609406917733847 (2017).
Tunstall, L. et al. Efficient few-shot learning without prompts. Preprint at arXiv https://doi.org/10.48550/arXiv.2209.11055 (2022).
Liu, Y. et al. Roberta: a robustly optimized BERT pretraining approach. Preprint at arXiv https://doi.org/10.48550/arXiv.1907.11692 (2019).
Wolf, T. et al. Transformers: State-of-the-Art Natural Language Processing. In Proc. 2020 Conference on Empirical Methods in Natural Language Processing: System Demonstrations (eds Liu, Q. & Schlangen, D.) 38–45 (Association for Computational Linguistics, 2020).
Pedregosa, F. et al. Scikit-learn: machine learning in Python. J. Mach. Learn. Res. 12, 2825–2830 (2011).
Gururangan, S. et al. Don't Stop Pretraining: Adapt Language Models to Domains and Tasks. In Proc. 58th Annual Meeting of the Association for Computational Linguistics (eds Jurafsky, D. et al.) 8342–8360 (Association for Computational Linguistics, 2020).
Vaswani, A. et al. Attention is all you need. Preprint at arXiv https://arxiv.org/abs/1706.03762 (2017).
Davies, P., Chapman, S. & Leask, J. Antivaccination activists on the World Wide Web. Arch. Dis. Child. 87, 22–25 (2002).
Friedlander, E. Opposition to immunization: a pattern of deception. Sci. Rev. Altern. Med. 5, 18–23 (2001).
Nasir, L. Reconnoitering the antivaccination web sites: news from the front. J. Fam. Pract. 49, 731–731 (2000).
Wolfe, R. M. Vaccine safety activists on the internet. Expert Review in Vaccines 1, 249–252 (2002).
Zimmerman, R. K. et al. Vaccine criticism on the World Wide Web. J. Med. Internet Res. 7, e369 (2005).
Bean, S. J. Emerging and continuing trends in vaccine opposition website content. Vaccine 29, 1874–1880 (2011).
Ward, J. K., Peretti-Watel, P., Larson, H. J., Raude, J. & Verger, P. Vaccine-criticism on the internet: new insights based on French-speaking websites. Vaccine 33, 1063–1070 (2015).
Jamison, A. et al. Adapting and extending a typology to identify vaccine misinformation on twitter. Am. J. Public Health 110, S331–S339 (2020).
Klimiuk, K., Czoska, A., Biernacka, K. & Balwicki, Ł. Vaccine misinformation on social media—topic-based content and sentiment analysis of Polish vaccine-deniers’ comments on Facebook. Hum. Vaccin. Immunother. 17, 2026–2035 (2021).
Broniatowski, D. A. et al. Facebook pages, the “Disneyland” measles outbreak, and promotion of vaccine refusal as a civil right, 2009–2019. Am. J. Public Health 110, S312–S318 (2020).
Kohler, S. & Koinig, I. The effect of science-related populism on vaccination attitudes and decisions. J. Behav. Med. 46, 1–10 (2022).
Griffith, J., Marani, H. & Monkman, H. et al. COVID-19 vaccine hesitancy in Canada: content analysis of tweets using the theoretical domains framework. J. Med. Internet Res. 23, e26874 (2021).
Nyhan, B., Reifler, J., Richey, S. & Freed, G. L. Effective messages in vaccine promotion: a randomized trial. Pediatrics 133, e835–e842 (2014).
Nyhan, B. & Reifler, J. Does correcting myths about the flu vaccine work? An experimental evaluation of the effects of corrective information. Vaccine 33, 459–464 (2015).
Miller, B. When is consensus knowledge based? Distinguishing shared knowledge from mere agreement. Synthese 190, 1293–1316 (2013).
Lemaitre, T. et al. Impact of a vaccination promotion intervention using motivational interview techniques on long-term vaccine coverage: the PromoVac strategy. Hum. Vaccin. Immunother. 15, 732–739 (2019).
Woolley, A. W., Aggarwal, I. & Malone, T. W. Collective intelligence and group performance. Curr. Dir. Psychol. Sci. 24, 420–424 (2015).
Holford, D. L., Fasce, A., Costello, T. & Lewandowsky, S. Psychological profiles of anti-vaccination argument endorsement. Sci. Rep. In press (2023).
Henrich, J., Heine, S. J. & Norenzayan, A. Most people are not weird. Nature 466, 29–29 (2010).
Rosenberg, B. D. & Siegel, J. T. A 50-year review of psychological reactance theory: do not read this article. Motiv. Sci. 4, 281 (2018).
Kahan, D. M. in Emerging Trends in the Social and Behavioral Sciences: An Interdisciplinary, Searchable, and Linkable Resource (eds Scott, R. & Kosslyn, S.) 1–16 (Wiley Online Library, 2015).
Holford, D. L., Schmid, P., Fasce, A. & Lewandowsky, S. The empathetic refutational interview to tackle vaccine misconceptions and improve vaccine acceptance. Preprint at OSF https://doi.org/10.31219/osf.io/8ndz2 (2023).
Page, M. J. et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int. J. Surg. 88, 105906 (2021).
Gusenbauer, M. & Haddaway, N. R. Which academic search systems are suitable for systematic reviews or meta-analyses? Evaluating retrieval qualities of Google Scholar, PubMed, and 26 other resources. Res. Synth. Methods 11, 181–217 (2020).
Hayes, A. F. & Krippendorff, K. Answering the call for a standard reliability measure for coding data. Commun. Methods Meas. 1, 77–89 (2007).
Kiger, M. E. & Varpio, L. Thematic analysis of qualitative data: Amee guide no. 131. Medical Teacher 42, 846–854 (2020).
Verelst, F., Kessels, R., Willem, L. & Beutels, P. No such thing as a free-rider? understanding drivers of childhood and adult vaccination through a multicountry discrete choice experiment. Vaccines 9, 264 (2021).
Wasserblat, M. Sentence transformer fine-tuning (setfit): Outperforms gpt-3 on few-shot text-classification while being 1600 times smaller. https://towardsdatascience.com/sentence-transformer-fine-tuning-setfit-outperforms-gpt-3-on-few-shot-text-classification-while-d9a3788f0b4e (2021)
Alex, N. et al. RAFT: A real-world few-shot text classification benchmark. https://arxiv.org/abs/2109.14076 (2021)
Gidengil, C., Chen, C., Parker, A. M., Nowak, S. & Matthews, L. Beliefs around childhood vaccines in the united states: A systematic review. Vaccine 37, 6793–6802 (2019).
Van den Hoven, M. Why one should do one’s bit: Thinking about free riding in the context of public health ethics. Public Health Ethics 5, 154–160 (2012).
Rozbroj, T., Lyons, A. & Lucke, J. Vaccine-hesitant and vaccine-refusing parents’ reflections on the way parenthood changed their attitudes to vaccination. J. Commun. Healthc. 45, 63–72 (2020).
Coan, T. G., Boussalis, C., Cook, J. & Nanko, M. O. Computer-assisted classification of contrarian claims about climate change. Sci. Rep. 11, 22320 (2021).
Smith, N. & Graham, T. Mapping the anti-vaccination movement on facebook. Information, Commun. Sci. 22, 1310–1327 (2019).
Argyris, Y. A. et al. Using machine learning to compare provaccine and antivaccine discourse among the public on social media: algorithm development study. JMIR public health and surveillance 7, e23105 (2021).
Arnold, K. The epidemic–terrorism nexus and how to safeguard africa against bioterrorism: Lessons from the global polio eradication initiative? South African Journal of International Affairs 28, 145–165 (2021).
Asveld, L. Mass-vaccination programmes and the value of respect for autonomy. Bioethics 22, 245–257 (2008).
Attwell, K., Smith, D. T. & Ward, P. R. ‘the unhealthy other’: How vaccine rejecting parents construct the vaccinating mainstream. Vaccine 36, 1621–1626 (2018).
Auwen, A., Emmons, M. & Dehority, W. Portrayal of immunization in american cinema: 1925 to 2016. Clinical pediatrics 59, 360–368 (2020).
Baines, A., Ittefaq, M. & Abwao, M. # scamdemic,# plandemic, or# scaredemic: what parler social media platform tells us about covid-19 vaccine. Vaccines 9, 421 (2021).
Baker, J. P. The pertussis vaccine controversy in great britain, 1974–1986. Vaccine 21, 4003–4010 (2003).
Basch, C. H., Meleo-Erwin, Z., Fera, J., Jaime, C. & Basch, C. E. A global pandemic in the time of viral memes: Covid-19 vaccine misinformation and disinformation on tiktok. Hum. Vaccin. Immunother. 17, 2373–2377 (2021).
Bean, S. J. & Catania, J. A. Immunology beliefs as a factor in vaccine opposition among complementary and alternative medical providers. SAGE Open Medicine 6, 2050312118807625 (2018).
Berezin, M. & Eads, A. Risk is for the rich? childhood vaccination resistance and a culture of health. Soc. Sci. Med. 165, 233–245 (2016).
Bonnevie, E. et al. Content themes and influential voices within vaccine opposition on twitter, 2019. Am J Public Health. 110, S326–S330 (2020).
Bonnevie, E., Gallegos-Jeffrey, A., Goldbarg, J., Byrd, B. & Smyser, J. Quantifying the rise of vaccine opposition on twitter during the covid-19 pandemic. J. Health Commun. 14, 12–19 (2021).
Bradshaw, A. S. et al. Propagandizing anti-vaccination: Analysis of vaccines revealed documentary series. Vaccine 38, 2058–2069 (2020).
Bradshaw, A. S., Shelton, S. S., Wollney, E., Treise, D. & Auguste, K. Pro-vaxxers get out: Anti-vaccination advocates influence undecided first-time, pregnant, and new mothers on facebook. Health Commun. 36, 693–702 (2021).
Brandmayr, F. Public epistemologies and intellectual interventions in contemporary italy. Int. J. Polit. Cult. Soc. 34, 47–68 (2021).
Bricker, B. & Justice, J. The postmodern medical paradigm: a case study of anti-mmr vaccine arguments. Western Journal of Communication 83, 172–189 (2019).
Buller, D. B. et al. Insights on hpv vaccination in the united states from mothers’ comments on facebook posts in a randomized trial. Hum. Vaccin. Immunother. 15, 1479–1487 (2019).
Buts, J. Memes of gandhi and mercury in anti-vaccination discourse. Media and Communication. 8, 353–363 (2020).
Byström, E., Lindstrand, A., Likhite, N., Butler, R. & Emmelin, M. Parental attitudes and decision-making regarding mmr vaccination in an anthroposophic community in sweden–a qualitative study. Vaccine 32, 6752–6757 (2014).
Cameron, D. imagine the perfect vaccine: Homeopathic vaccine alternatives and vaccine discourse in english canada. Canadian Bulletin of Medical History 38, 32–62 (2021).
Carrion, M. L. you need to do your research: Vaccines, contestable science, and maternal epistemology. Public Underst. Sci. 27, 310–324 (2018).
Caulfield, T., Marcon, A. R. & Murdoch, B. Injecting doubt: responding to the naturopathic anti-vaccination rhetoric. Journal of Law and the Biosciences 4, 229–249 (2017).
Cloes, R., Ahmad, A. & Reintjes, R. Risk communication during the 2009 influenza a (h1n1) pandemic: stakeholder experiences from eight european countries. Disaster Med. Public Health Prep. 9, 127–133 (2015).
Cmeciu, C. & Coman, I. Governmental and public thematic patterns on vaccination during a measles outbreak: the romanian perspective. Glob. Health Promot. 28, 23–31 (2021).
Conis, E. A mother’s responsibility: women, medicine, and the rise of contemporary vaccine skepticism in the united states. Bulletin of the History of Medicine 87, 407–435 (2013).
Conis, E. Vaccines, pesticides, and narratives of exposure and evidence. Canadian Bulletin of Medical History 34, 297–326 (2017).
Covolo, L., Ceretti, E., Passeri, C., Boletti, M. & Gelatti, U. What arguments on vaccinations run through youtube videos in italy? a content analysis. Hum. Vaccin. Immunother. 13, 1693–1699 (2017).
Criss, S. et al. Advocacy, hesitancy, and equity: exploring us race-related discussions of the covid-19 vaccine on twitter. Int. J. Environ. Res. Public Health 18, 5693 (2021).
Davis, M. ‘globalist war against humanity shifts into high gear’: Online anti-vaccination websites and ‘anti-public’discourse. Public Understanding of Science 28, 357–371 (2019).
DeDominicis, K. et al. Shouting at each other into the void: A linguistic network analysis of vaccine hesitance and support in online discourse regarding california law sb277. Soc. Sci. Med. 266, 113216 (2020).
Deml, M. J. et al. we treat humans, not herds!: A qualitative study of complementary and alternative medicine (cam) providers’ individualized approaches to vaccination in switzerland. Soc. Sci. Med. 240, 112556 (2019).
Kinder, F. D. Parental refusal of human papillomavirus vaccine: multisite study. J. Pediatr. Health Care 32, 150–156 (2018).
Duchsherer, A., Jason, M., Platt, C. A. & Majdik, Z. P. Immunized against science: Narrative community building among vaccine refusing/hesitant parents. Public Underst. Sci. 29, 419–435 (2020).
Ekram, S., Debiec, K. E., Pumper, M. A. & Moreno, M. A. Content and commentary: Hpv vaccine and youtube. Journal of pediatric and adolescent gynecology 32, 153–157 (2019).
Elbarazi, I. et al. Exploring vaccine hesitancy among healthcare providers in the united arab emirates: a qualitative study. Hum. Vaccin. Immunother. 17, 2018–2025 (2021).
Evans, M. R., Prout, H., Prior, L., Tapper-Jones, L. M. & Butler, C. C. A qualitative study of lay beliefs about influenza immunisation in older people. British Journal of General Practice 57, 352–358 (2007).
Fadda, M., Allam, A. & Schulz, P. J. Arguments and sources on italian online forums on childhood vaccinations: Results of a content analysis. Vaccine 33, 7152–7159 (2015).
Fichman, M. & Keelan, J. E. Resister’s logic: the anti-vaccination arguments of alfred russel wallace and their role in the debates over compulsory vaccination in england, 1870–1907. Stud. Hist. Philos. Biol. Biomed. Sci. 38, 585–607 (2007).
Gallagher, J. & Lawrence, H. Y. et al. Rhetorical appeals and tactics in new york times comments about vaccines: Qualitative analysis. Journal of medical internet research 22, e19504 (2020).
Gargiulo, F., Cafiero, F., Guille-Escuret, P., Seror, V. & Ward, J. K. Asymmetric participation of defenders and critics of vaccines to debates on french-speaking twitter. Sci. Rep. 10, 1–12 (2020).
Glanz, J. M. et al. A mixed methods study of parental vaccine decision making and parent–provider trust. Academic pediatrics 13, 481–488 (2013).
Gorman, D., Bielecki, K., Willocks, L. & Pollock, K. A qualitative study of vaccination behaviour amongst female polish migrants in edinburgh, scotland. Vaccine 37, 2741–2747 (2019).
Grandahl, M. et al. Not the right time: why parents refuse to let their daughters have the human papillomavirus vaccination. Acta Paediatrica 103, 436–441 (2014).
Grant, L. et al. Vaccination persuasion online: a qualitative study of two provaccine and two vaccine-skeptical websites. J. Med. Internet Res. 17, e133 (2015).
Guidry, J. P., Carlyle, K., Messner, M. & Jin, Y. On pins and needles: how vaccines are portrayed on pinterest. Vaccine 33, 5051–5056 (2015).
Guillari, A. et al. Influenza vaccination and healthcare workers: barriers and predisposing factors. a literature review. Acta Bio Medica: Atenei Parmensis 92 (2021).
Gullion, J. S., Henry, L. & Gullion, G. Deciding to opt out of childhood vaccination mandates. Public health nursing 25, 401–408 (2008).
Harvey, A. M., Thompson, S., Lac, A. & Coolidge, F. L. Fear and derision: a quantitative content analysis of provaccine and antivaccine internet memes. Health Educ. Behav. 46, 1012–1023 (2019).
Hasnan, S. & Tan, N. C. Multi-domain narrative review of vaccine hesitancy in childhood. Vaccine 39, 1910–1920 (2021).
Hausman, B. L., Ghebremichael, M., Hayek, P. & Mack, E. ‘poisonous, filthy, loathsome, damnable stuff’: the rhetorical ecology of vaccination concern. The Yale journal of biology and medicine 87, 403 (2014).
Hobson-West, P. ‘trusting blindly can be the biggest risk of all’: organised resistance to childhood vaccination in the uk. Sociology of health & illness 29, 198–215 (2007).
Hoffman, B. L. et al. It’s not all about autism: The emerging landscape of anti-vaccination sentiment on facebook. Vaccine 37, 2216–2223 (2019).
Hoffman, B. L. et al. # doctorsspeakup: Lessons learned from a pro-vaccine twitter event. Vaccine 39, 2684–2691 (2021).
Hopfer, S. & Clippard, J. R. College women’s hpv vaccine decision narratives. Qual. Health Res. 21, 262–277 (2011).
Izzati, A. N. et al. Pro-and anti-vaccination among mothers in deciding children’s immunization: A qualitative study. J. Med. Sci. 9, 385–391 (2021).
Jama, A., Ali, M., Lindstrand, A., Butler, R. & Kulane, A. Perspectives on the measles, mumps and rubella vaccination among somali mothers in stockholm. Int. J. Environ. Res. Public Health 15, 2428 (2018).
Jamal, D. et al. Low vaccination in rural sindh, pakistan: a case of refusal, ignorance or access? Vaccine 38, 4747–4754 (2020).
Jamison, A. M. et al. Vaccine-related advertising in the facebook ad archive. Vaccine 38, 512–520 (2020).
Jenkins, M. C. & Moreno, M. A. Vaccination discussion among parents on social media: A content analysis of comments on parenting blogs. J. Health Commun. 25, 232–242 (2020).
Kaler, A. Health interventions and the persistence of rumour: the circulation of sterility stories in african public health campaigns. Soc. Sci. Med. 68, 1711–1719 (2009).
Kasstan, B. a free people, controlled only by god: Circulating and converting criticism of vaccination in jerusalem. Culture, Medicine, and Psychiatry 46, 277–296 (2022).
Kata, A. Anti-vaccine activists, web 2.0, and the postmodern paradigm–an overview of tactics and tropes used online by the anti-vaccination movement. Vaccine 30, 3778–3789 (2012).
Kaufman, M. The american anti-vaccinationists and their arguments. Bulletin of the History of Medicine 41, 463–478 (1967).
Keelan, J., Pavri, V., Balakrishnan, R. & Wilson, K. An analysis of the human papilloma virus vaccine debate on myspace blogs. Vaccine 28, 1535–1540 (2010).
Khan, S. A. et al. Developing a three-dimensional narrative to counter polio vaccine refusal in charsadda. J. Glob. Health 10 (2020).
Khan, Y. H. et al. Threat of covid-19 vaccine hesitancy in pakistan: the need for measures to neutralize misleading narratives. The American journal of tropical medicine and hygiene 103, 603 (2020).
Kitta, A. Alternative health websites and fake news: Taking a stab at definition, genre, and belief. Journal of American Folklore 131, 405–412 (2018).
Kolla¸taj, W. P., Kolla¸taj, B., Panasiuk, L., Sobieszczanski, J. & Karwat, I. D. Anti-vaccine movements–a form of social activity for health care, ignorance or diversion aimed at destabilizing the health situation? part 1. epidemiological safety. vaccinations–pros and cons. Annals of Agricultural and Environmental Medicine 27, 544 (2020).
Krawczyk, A. et al. Parents’ decision-making about the human papillomavirus vaccine for their daughters: Ii. qualitative results. Hum. Vaccin. Immunother. 11, 330–336 (2015).
Lahouati, M., De Coucy, A., Sarlangue, J. & Cazanave, C. Spread of vaccine hesitancy in france: What about youtube? Vaccine 38, 5779–5782 (2020).
Leader, A. E., Burke-Garcia, A., Massey, P. M. & Roark, J. B. Understanding the messages and motivation of vaccine hesitant or refusing social media influencers. Vaccine 39, 350–356 (2021).
Leask, J.-A. & Chapman, S. ‘an attempt to swindle nature’: press anti-immunisation reportage 1993–1997. Australian and New Zealand journal of public health 22, 17–26 (1998).
Lee, M. S. & Male, M. Against medical advice: the anti-consumption of vaccines. Journal of Consumer Marketing 28, 484–490 (2011).
Lefèvre, H., Schrimpf, C., Moro, M. R. & Lachal, J. Hpv vaccination rate in french adolescent girls: an example of vaccine distrust. Archives of disease in childhood 103, 740–746 (2018).
Lehmann, B. A., Ruiter, R. A. & Kok, G. A qualitative study of the coverage of influenza vaccination on dutch news sites and social media websites. BMC public health 13, 1–13 (2013).
Luthy, K. E., Beckstrand, R. L. & Callister, L. C. Parental hesitation in immunizing children in utah. Public Health Nursing 27, 25–31 (2010).
Madden, K., Nan, X., Briones, R. & Waks, L. Sorting through search results: a content analysis of hpv vaccine information online. Vaccine 30, 3741–3746 (2012).
McClaran, N. & Rhodes, N. Portrayals of vaccination in entertainment television: A content analysis. Health commun. 36, 1242–1251 (2021).
Meharry, P. M., Colson, E. R., Grizas, A. P., Stiller, R. & Vázquez, M. Reasons why women accept or reject the trivalent inactivated influenza vaccine (tiv) during pregnancy. Maternal and child health journal 17, 156–164 (2013).
Mendel-Van Alstyne, J. A., Nowak, G. J. & Aikin, A. L. What is ‘confidence’and what could affect it?: A qualitative study of mothers who are hesitant about vaccines. Vaccine 36, 6464–6472 (2018).
Meyer, S. B. et al. Vaccine hesitancy and web 2.0: Exploring how attitudes and beliefs about influenza vaccination are exchanged in online threaded user comments. Vaccine 37, 1769–1774 (2019).
Mitilian, E., Malli, F. & Verger, P. Image of the new vaccination obligation through the media. Vaccine 38, 498–511 (2020).
Muzembo, B. A. et al. Local perspectives on ebola during its tenth outbreak in dr congo: A nationwide qualitative study. PLoS One 15, e0241120 (2020).
Nugier, A., Limousi, F. & Lydié, N. Vaccine criticism: Presence and arguments on french-speaking websites. Médecine et Maladies Infectieuses 48, 37–43 (2018).
Okuhara, T., Ishikawa, H., Kato, M., Okada, M. & Kiuchi, T. A qualitative analysis of the beliefs of japanese anti-influenza vaccination website authors. Heliyon 4, e00609 (2018).
Penta, M. A. & Baban, A. Dangerous agent or saviour? hpv vaccine representations on online discussion forums in romania. Int. J. Behav. Med. 21, 20–28 (2014).
Petousis-Harris, H. A., Goodyear-Smith, F. A., Kameshwar, K. & Turner, N. Fact or fallacy? immunisation arguments in the new zealand print media. Australian and New Zealand journal of public health 34, 521–526 (2010).
Platonov, K. & Svetlov, K. Conspiracy theories dissemination on sns vkontakte: Covid-19 case. In Electronic Governance and Open Society: Challenges in Eurasia: 7th International Conference, EGOSE 2020, St. Petersburg, Russia, November 18–19, 2020, Proceedings 7, 322-335 (Springer, 2020).
Pless, A., McLennan, S. R., Nicca, D., Shaw, D. M. & Elger, B. S. Reasons why nurses decline influenza vaccination: a qualitative study. BMC nursing 16, 1–7 (2017).
Pop, C. A. Cervical cancer narratives: invoking ‘god’s will’to re-appropriate reproductive rights in present-day romania. Culture, Health & Sexuality 17, 48–62 (2015).
Pop, C. A. Locating purity within corruption rumors: narratives of hpv vaccination refusal in a peri-urban community of southern romania. Medical Anthropology Quarterly 30, 563–581 (2016).
Pullagura, G. R., Violette, R., Houle, S. K. & Waite, N. M. Shades of gray in vaccination decisions–understanding community pharmacists’ perspectives of, and experiences with, influenza vaccine hesitancy in ontario, canada. Vaccine 38, 2551–2558 (2020).
Quinn, S., Jamison, A., Musa, D., Hilyard, K. & Freimuth, V. Exploring the continuum of vaccine hesitancy between african american and white adults: results of a qualitative study. PLoS currents 8 (2016).
Radovanovic, Z. Anti-vaccinationists and their arguments in the balkan countries that share the same language. Srpski arhiv za celokupno lekarstvo 145, 199–204 (2017).
Reich, J. A. Teaching women to question and control: public pedagogies of birth and vaccine refusal. BioSocieties 15, 580–600 (2020).
Reid, J. A. & Mabhala, M. A. Ethnic and minority group differences in engagement with covid-19 vaccination programmes–at pandemic pace; when vaccine confidence in mass rollout meets local vaccine hesitancy. Israel Journal of Health Policy Research 10, 33 (2021).
Rhudy, L. M., Tucker, S. J., Ofstead, C. L. & Poland, G. A. Personal choice or evidence-based nursing intervention: nurses’ decision-making about influenza vaccination. Worldviews on Evidence-Based Nursing 7, 111–120 (2010).
Rochel de Camargo Jr, K. Here we go again: the reemergence of anti-vaccine activism on the internet. Cadernos de saude publica 36, e00037620 (2020).
Rodriguez, N. J. Vaccine-hesitant justifications: too many, too soon, narrative persuasion, and the conflation of expertise. Global Qualitative Nursing Research 3, 2333393616663304 (2016).
Rozbroj, T., Lyons, A. & Lucke, J. Vaccine-hesitant and vaccine-refusing parents’ reflections on the way parenthood changed their attitudes to vaccination. J. community health 45, 63–72 (2020).
Rundblad, G. Why some messages speak better: Child immunization in the news and on the internet. Current Drug Safety 10, 87–93 (2015).
Russell, S. J. et al. Oncolytic measles virotherapy and opposition to measles vaccination. In Mayo Clinic Proceedings, vol. 94, 1834-1839 (Elsevier, 2019).
Schwartz, J. L. New media, old messages: themes in the history of vaccine hesitancy and refusal. AMA Journal of Ethics 14, 50–55 (2012).
Skeppstedt, M., Kerren, A. & Stede, M. Vaccine hesitancy in discussion forums: Computer-assisted argument mining with topic models. In Building Continents of Knowledge in Oceans of Data: The Future of Co-Created eHealth, 366-370 (IOS Press, 2018).
Smith, M. J. Promoting vaccine confidence. Infectious Disease Clinics 29, 759–769 (2015).
Smith, T. C. Vaccine rejection and hesitancy: a review and call to action. In Open forum infectious diseases, vol. 4 (Oxford University Press, 2017).
Smith, T. C. & Reiss, D. R. Digging the rabbit hole, covid-: anti-vaccine themes and the discourse around covid-19. Microbes and infection 22, 608–610 (2020).
Sobo, E. J., Huhn, A., Sannwald, A. & Thurman, L. Information curation among vaccine cautious parents: Web 2.0, pinterest thinking, and pediatric vaccination choice. Medical anthropology 35, 529–546 (2016).
Spier, R. E. Perception of risk of vaccine adverse events: a historical perspective. Vaccine 20, S78–S84 (2001).
Stolle, L. B. et al. Fact vs fallacy: the anti-vaccine discussion reloaded. Advances in therapy 37, 4481–4490 (2020).
Succi, R. Cd. M. Vaccine refusal-what we need to know. Jornal de pediatria 94, 574–581 (2018).
Syiroj, A. T. R., Pardosi, J. F. & Heywood, A. E. Exploring parents’ reasons for incomplete childhood immunisation in indonesia. Vaccine 37, 6486–6493 (2019).
Tagajdid, M. R. et al. Factors influencing uptake of influenza vaccine amongst healthcare workers in a regional center after the a (h1n1) 2009 pandemic: lessons for improving vaccination rates. International Journal of Risk & Safety in Medicine 23, 249–254 (2011).
Tandy, C. B. & Jabson Tree, J. M. Attitudes of east tennessee residents towards general and pertussis vaccination: a qualitative study. BMC Public Health 21, 1–11 (2021).
Thelwall, M., Kousha, K. & Thelwall, S. Covid-19 vaccine hesitancy on english-language twitter. Profesional de la información (EPI) 30 (2021).
Tolley, K. School vaccination wars: The rise of anti-science in the american anti-vaccination societies, 1879–1929. History of Education Quarterly 59, 161–194 (2019).
Tomeny, T. S., Vargo, C. J. & El-Toukhy, S. Geographic and demographic correlates of autism-related anti-vaccine beliefs on twitter, 2009-15. Soc. Sci. Med. 191, 168–175 (2017).
Uibu, M. et al. doctors just don’t care about people! how medical specialists are depicted in a vaccine-critical estonian facebook group. Folklore: Electronic Journal of Folklore 215–238 (2021).
Vamos, C. A., McDermott, R. J. & Daley, E. M. The hpv vaccine: framing the arguments for and against mandatory vaccination of all middle school girls. J. Sch. Health 78, 302–309 (2008).
Velan, B., Kaplan, G., Ziv, A., Boyko, V. & Lerner-Geva, L. Major motives in non-acceptance of a/h1n1 flu vaccination: the weight of rational assessment. Vaccine 29, 1173–1179 (2011).
Venkatraman, A., Garg, N. & Kumar, N. Greater freedom of speech on web 2.0 correlates with dominance of views linking vaccines to autism. Vaccine 33, 1422–1425 (2015).
Vercruysse, J. et al. Parents’ and providers’ attitudes toward school-located provision and school-entry requirements for hpv vaccines. Hum. Vaccin. Immunother. 12, 1606–1614 (2016).
Verger, P., Bocquier, A., Vergélys, C., Ward, J. & Peretti-Watel, P. Flu vaccination among patients with diabetes: motives, perceptions, trust, and risk culture-a qualitative survey. BMC Public Health 18, 1–10 (2018).
Ward, J. K. Rethinking the antivaccine movement concept: a case study of public criticism of the swine flu vaccine’s safety in france. Soc. Sci. Med. 159, 48–57 (2016).
Ward, P. R., Attwell, K., Meyer, S. B., Rokkas, P. & Leask, J. Understanding the perceived logic of care by vaccine-hesitant and vaccine-refusing parents: a qualitative study in australia. PloS one 12, e0185955 (2017).
Wawrzuta, D., Jaworski, M., Gotlib, J. & Panczyk, M. Characteristics of antivaccine messages on social media: systematic review. J. Med. Internet Res. 23, e24564 (2021).
Weitz, L., Bellach, L., Faltum, A., Berger, A. & Maurer, W. Vaccine hesitancy: Report of a student study group. Wiener klinische Wochenschrift 132, 243–252 (2020).
Winslade, C., Heffernan, C. & Atchison, C. Experiences and perspectives of mothers of the pertussis vaccination programme in london. Public Health 146, 10–14 (2017).
Wiyeh, A. B. et al. Social media and hpv vaccination: Unsolicited public comments on a facebook post by the western cape department of health provide insights into determinants of vaccine hesitancy in south africa. Vaccine 37, 6317–6323 (2019).
Wong, L., Wong, P. & AbuBakar, S. Vaccine hesitancy and the resurgence of vaccine preventable diseases: the way forward for malaysia, a southeast asian country. Hum. Vaccin. Immunother. 16, 1511–1520 (2020).
Xu, Z., Ellis, L. & Umphrey, L. R. The easier the better? comparing the readability and engagement of online pro-and anti-vaccination articles. Health Educ. Behav. 46, 790–797 (2019).
Yeung, M. W. & Yau, A. H. ‘this year’s vaccine is only 10% effective’: a study of public discourse on vaccine effectiveness in hong kong. J. Healthc. Commun. 14, 78–89 (2021).
Zuk, P. & Zuk, P. Right-wing populism in poland and anti-vaccine myths on youtube: Political and cultural threats to public health. Global Public Health 15, 790–804 (2020).
Mønsted, B. & Lehmann, S. Algorithmic detection and analysis of vaccine-denialist sentiment clusters in social networks. arXiv preprint arXiv:1905.12908 (2019).
Sharma, K., Zhang, Y. & Liu, Y. Covid-19 vaccines: characterizing misinformation campaigns and vaccine hesitancy on twitter (2021).
Ackermann, D., Chapman, S. & Leask, J. Media coverage of anthrax vaccination refusal by Australian Defence Force personnel. Vaccine 23, 411–417 (2004).
Gruzd, A. & Mai, P. COVID-19 misinformation portal—a rapid response project from the Ryerson University social media lab. COVID19MisInfo.org Portal https://covid19misinfo.org/ (2020).
Acknowledgements
This project has received funding from the European Union’s Horizon 2020 research and innovation programme under grant agreement no. 964728 (JITSUVAX). L.B. and I.G. were funded by the German Federal Ministry of Education and Research and by the Hessian Ministry of Science and the Arts (HMWK) within the projects ‘The Third Wave of Artificial Intelligence – 3AI’, hessian.AI, and within their joint support of the National Research Center for Applied Cybersecurity ATHENE. S.L. also acknowledges support from the Humboldt Foundation through a research award. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
A.F.: conceptualization, data curation, formal analysis, investigation, methodology, supervision, writing—original draft, and writing—review and editing. P.S.: conceptualization, data curation, formal analysis, investigation, methodology, visualization, writing—original draft, and writing—review and editing. D.L.H.: conceptualization, data curation, formal analysis, investigation, methodology, visualization, writing—original draft, and writing—review and editing. L.B.: conceptualization, formal analysis, investigation, methodology, visualization, writing—original draft, and writing—review and editing. I.G.: funding acquisition, supervision, and writing—review and editing. S.L.: conceptualization, formal analysis, funding acquisition, investigation, methodology, supervision, visualization, and writing—review and editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Peer review
Peer review information
Nature Human Behaviour thanks Matthew Hornsey, David Broniatowski and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Peer reviewer reports are available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Table 1: Classification of articles. Supplementary Table 2: Krippendorff ’s alphas. Supplementary Figs. 1–3: Word clouds. Supplementary Figs. 4 and 5: Frequency of attitude roots. Supplementary Table 3: Summary statistics of both datasets. Supplementary Figs. 6 and 7 and Supplementary Table 4: Confirmatory text modelling using LDA. Supplementary Table 5: Text classification on Study 2 fact checks. Supplementary Figs. 8 and 9, and links to the 3D gifs: Visualization of attitude roots.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fasce, A., Schmid, P., Holford, D.L. et al. A taxonomy of anti-vaccination arguments from a systematic literature review and text modelling. Nat Hum Behav 7, 1462–1480 (2023). https://doi.org/10.1038/s41562-023-01644-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41562-023-01644-3