Abstract
We present a panel dataset of COVID-19 vaccine policies, with data from 01 January 2020 for 185 countries and a number of subnational jurisdictions, reporting on vaccination prioritization plans, eligibility and availability, cost to the individual and mandatory vaccination policies. For each of these indicators, we recorded who is targeted by a policy using 52 standardized categories. These indicators document a detailed picture of the unprecedented scale of international COVID-19 vaccination rollout and strategy, indicating which countries prioritized and vaccinated which groups, when and in what order. We highlight key descriptive findings from these data to demonstrate uses for the data and to encourage researchers and policymakers in future research and vaccination planning. Numerous patterns and trends begin to emerge. For example: ‘eliminator’ countries (those that aimed to prevent virus entry into the country and community transmission) tended to prioritize border workers and economic sectors, while ‘mitigator’ countries (those that aimed to reduce the impact of community transmission) tended to prioritize the elderly and healthcare sectors for the first COVID-19 vaccinations; high-income countries published prioritization plans and began vaccinations earlier than low- and middle-income countries. Fifty-five countries were found to have implemented at least one policy of mandatory vaccination. We also demonstrate the value of combining this data with vaccination uptake rates, vaccine supply and demand data, and with further COVID-19 epidemiological data.
Similar content being viewed by others
Main
The COVID-19 pandemic drove an unprecedented effort to develop and deploy vaccines at scale. As of 15 June 2022, 37 COVID-19 vaccines were in Phase 3 clinical trials, authorized for early use or approved for full use (https://www.nytimes.com/interactive/2020/science/coronavirus-vaccine-tracker.html), with some available for use in infants as young as 6 months old1,2. Eleven vaccines have now been given Emergency Use Listing (EUL) from the World Health Organization (WHO)3, and more than 11.9 billion (as of 15 June 2022, https://ourworldindata.org/covid-vaccinations?country=OWID_WRL) COVID-19 vaccine doses have been delivered worldwide4,5,6. Nonetheless, more than 30% of the world population remains unvaccinated3, and COVID-19 vaccines and public health measures to promote them have generated substantial political controversy in many countries7.
Given that vaccines against COVID-19 and other diseases will continue to play a critical role in combating the COVID-19 pandemic and future diseases, there is an enormous need to better understand both how governments use vaccines and the factors that drive or inhibit uptake. Within the latter, the policies and measures that governments adopt to promote vaccination play an important role. This resource article introduces a new dataset from the Oxford COVID-19 Government Response Tracker (OxCGRT) project8 that provides cross-national and longitudinal information on COVID-19 vaccination policies across the world. The new dataset covers vaccine prioritization policies (V1), vaccine availability and eligibility by group (V2), whether there is a cost to individual recipients at the point of use (V3) and mandate policies (V4) (Table 1). Developed in consultation with governments, policymakers, stakeholders in the field and the OxCGRT expert advisory board, this dataset allows researchers and policymakers to systematically compare government vaccination strategies and assess distributional capabilities (see Methods for more information on dataset design). Through combination with other datasets, further analyses, such as on the impact of distribution policies on uptake, are made possible.
The dataset is composed of four indicators that report national-level COVID-19 vaccination policies for 52 population categories from 1 January 2020 to 31 December 2022 for 185 jurisdictions in the national database, as well as subnational jurisdictions (provinces) for Canada and (states) for the United States (subnational-jurisdiction data for other countries are in development and will be added to the online data repository as they become available). Collected by a specially trained team of OxCGRT volunteer data contributors, the dataset has been reviewed for quality assurance and accuracy by core OxCGRT researchers and a specially trained review team. The results presented here focus only on the national-level data. The 52 population categories include general and at-risk age groups (in 5-yr intervals for individuals over 16 yr), occupational categories (based on exposure and transmission risk and economic function—groups of people working in occupations critical to the economic function of the country, including essential workers and airport/border staff) and medical categories (based on vulnerability) (Table 2). These closely reflect the categories listed in the WHO Strategic Advisory Group of Experts on Immunization (SAGE) values framework for the allocation and prioritization of COVID-19 vaccination, a framework that guides the allocation of vaccinations under limited supply to specific population groups to meet specific outcomes.
Here we present some variations and temporal patterns of COVID-19 vaccine prioritization, eligibility, distribution, cost and mandates by group, with the aim of illustrating how the new dataset can offer insights for researchers and policymakers. By mapping variation in vaccination policies over time, this dataset provides a means of responding to critical questions about the role of vaccines in the COVID-19 pandemic. The four indicators are presented in the dataset alongside vaccination rates so that users can easily generate cross-national and within-country comparisons to explore associations between vaccination policies, those prioritized for vaccination and vaccine uptake. The dataset’s jurisdiction–day format purposefully facilitates merging with other data sources. For example, combining these four vaccine policy indicators with data about other kinds of pandemic policies—relating to closures, economic support and health, such as testing—allows for assessment of the interplay of vaccination programmes within the broader context of pandemic management. Combining these data with other social science indicators broadens the possibilities further, towards considerations of the impacts of vaccination policies in different economic, political, cultural or religious contexts, and how controversies towards COVID-19 vaccines may have shaped policy. Comparisons between countries with similar demographics, or those with unique demographics and geography might highlight best practice for future pandemics10.
Results
To motivate use of this new dataset, in this section we illustrate some initial observations using the four vaccine policy indicators. First, we focus on the first two indicators (V1 and V2). We note common patterns in vaccination prioritization strategies according to the broader strategies guiding countries’ pandemic management, and by country income level. We then observe country-level variation in both prioritization and actual distribution by age group and other kinds of vulnerability categories. Second, we consider the additional two indicators (V3 and V4), briefly discussing the cost of vaccination to individuals, before exploring vaccine mandate policies. Although we find limited variation relating to cost across countries—almost all countries provided the vaccine to people free of charge—we detail the diversity of countries’ vaccine mandate policies, ranging from non-existent, to policies specific to certain age groups, occupation groups and populations carrying out specific religious activities, or working in named locations.
Comparing countries’ prioritization plans
The vaccine prioritization (V1) indicator captures the order in which governments planned to deploy COVID-19 vaccines to different categories of people. It depicts the published plans of all countries in the OxCGRT dataset (only Eritrea, of 185 countries, has yet to begin COVID-19 vaccinations or publish a vaccination plan). These plans were primarily used to ration limited supplies at a time when global vaccine supply was constrained. As such, they help reveal the evolving priorities governments held for vaccine deployment.
Broadly, we can distinguish two ideal typical COVID-19 strategies: elimination and mitigation. Roughly, studies have categorized these strategies by observing how eliminators aimed to keep the virus out of the country and to prevent community transmission. In contrast, mitigators sought to reduce the impact of community transmission by flattening the curve and reducing cases and deaths11,12,13,14. Many countries in the WHO West Pacific Region adopted policies closer to the elimination model, perhaps in part due to the region’s previous experience with SARS11,13. Relatedly, it has also been hypothesized that island nations may have been more likely to pursue elimination models during COVID-19 due to their geographical advantage of isolation and ability to seal national borders, although for many low-income countries (LICs) and LMICs, this came at appreciable economic cost11,15,16,17,18. Finally, early responses to the COVID-19 pandemic have also highlighted distinctions between mitigation and elimination strategies based on the Organisation for Economic Co-operation and Development (OECD) countries, such as high-performing surveillance systems with early and targeted contact tracing and widespread efficient testing in eliminator countries12,14.
Interestingly, we observe a clear distinction in the vaccination rollout strategies of countries that have been characterized as pursuing an elimination strategy throughout much of the COVID-19 pandemic, compared to countries that pursued a mitigation strategy11,12,13,14,19. Table 3 highlights how nine selected eliminators (selected as examples from a comprehensive list of eliminators, see Supplementary Table 3), such as Australia and New Zealand, prioritized frontline workers and border staff alongside clinically vulnerable people (those with co-morbidities and/or predispositions to illness) in their first rounds of vaccination (that is, positioned rank 1), while nine selected mitigators (see Supplementary Table 3 for comprehensive list of mitigators) focused instead on vaccinating only clinically vulnerable and elderly populations, along with healthcare workers. Looking across all countries in our dataset, while 11 out of 19 (58%) Western Pacific countries prioritized first-round vaccinations on the basis of economic function, only 42 out of 164 (26%) non-Western Pacific countries did so. When looking at the OECD subset, we observe the same pattern: 2 out of 5 countries that adopted elimination in the early stages of the pandemic (40%) prioritized vaccination on the basis of economic function versus 4 out of 32 (12%) mitigators. Finally, the same descriptive pattern holds for island nations (16 out of 32, 50%) when contrasted to non-island nations, with 16 (50%) island countries adopting economic function prioritized vaccination versus non-island countries (38 out of 151, 25%). In contrast, only 3 Western Pacific countries (16%) prioritized clinically vulnerable people, versus 80 (49%) for countries outside the region. However, we observe no differences in descriptive patterns for either OECD or island country groupings. While 3 out of 5 OECD countries that adopted elimination strategies in the early stages of the pandemic (60%) prioritized clinically vulnerable people, 19 out of 32 mitigators did so. Finally, 44% of island (14 out of 32) and 46% of non-island countries (70 out of 151) prioritized clinically vulnerable people.
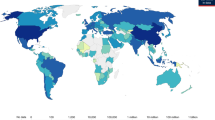
When we map country differences in the most- (or equal-most-) prioritized categories of people (Fig. 1), we observe that almost all countries in our dataset placed healthcare workers among the first to receive COVID-19 vaccines (91% of countries, or 168/185) presumably both to reduce transmission and mitigate health impacts for those at high risk of exposure. Following healthcare workers, 54% (101) of countries also prioritized populations deemed to be clinically vulnerable. Seventy-four countries (40%) prioritized groups of people critical to the economic function of the country, 45 prioritized (24%) categories related to the public function of the country, and 27 countries (15%) focused on educators and/or students for COVID-19 vaccinations.
Countries in blue prioritized certain aspects or functions of population groups as part of their first round of COVID-19 vaccinations (position rank 1). Education (educators, primary/tertiary students, tertiary education students); Clinically vulnerable (clinically vulnerable/chronic illness/significant underlying health condition); Socially vulnerable (ethnic minorities, refugees/migrants, crowded/communal living); Economic function (frontline retail workers, frontline/essential workers, airport/border staff, other high-contact professions, factory workers); Healthcare workforce (healthcare workers, staff in elderly care homes, people living with a vulnerable person); Public function (government officials, police/first responders, military, religious/spiritual leaders).
Comparing countries’ plans with actual distribution
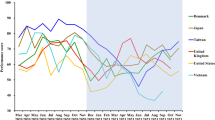
By the end of 2021, 62 (34%) countries had published COVID-19 vaccination rollout plans and prioritization lists, often with rough estimates for the timing of each phase. Of those, 48 countries began vaccination before the end of 2021 (Fig. 2), and by 31 March 2021, 107 more countries had published their COVID-19 vaccination plans and priorities. In countries with access to vaccines, deployment swiftly followed plans (captured by indicator V2, which records the groups actually receiving a vaccine in a country). Because vaccine access was highly related to countries’ income levels20, Fig. 2 groups countries according to the World Bank income classification groups for 2021 (https://datatopics.worldbank.org/world-development-indicators/the-world-by-income-and-region.html). HICs were the first to publish vaccination plans to secure COVID-19 vaccines and to begin administration of vaccines for their populations, reflecting their greater ability to produce and purchase vaccines. Figure 2 shows that the publication of plans and subsequent administration of vaccine doses then followed in upper middle-income countries (UMICs), LMICs and then LICs, respectively. HICs moved quicker to expand vaccination eligibility to the 12+ yr age group than LMICs. It also shows that despite publishing plans and beginning vaccinations at later dates than HICs and UMICs, some LMICs and LICs quickly moved from prioritized vaccinations by age or occupation to universal access (defined in our dataset as being available widely to all those over the age of 16+ yr or 18+ yr, with age floor dependent on vaccine brand). LMICs and LICs have had far fewer vaccine doses available to them than HICs and UMICs (https://data.undp.org/vaccine-equity/accessibility/), so one possible explanation for the swift movement towards universal access in LICs and LMICs may be an attempt to vaccinate larger proportions of their populations in the face of vaccine hesitancy. However, there are conflicting views on whether LMICs and LICs are more or less vaccine hesitant towards COVID-19 vaccines than HICs and UMICs21,22,23. Another possible explanation for the quick move to (ostensibly) universal access (despite low vaccine supply) may have been to reduce public perception of favouring or excluding certain groups in the face of a public health emergency and with varying social and geographic challenges in the distribution of vaccines24,25.
Comparing categories by age and vulnerability status
Only 11 countries in our dataset did not specifically prioritize elderly populations (the age cut-off for ‘elderly’ is defined locally, see Methods) in their plans and rollouts of COVID-19 vaccines (Bangladesh, Burkina Faso, Cambodia, Macau, Namibia, Russia, Trinidad and Tobago, Uganda, Uruguay, Zimbabwe and Taiwan). Long-term care facilities (LTCFs; nursing homes, elderly care homes and so on) are a concept and cultural phenomenon predominantly found in some relatively wealthy countries26. This is reflected in our data (Fig. 3), with most African, South Asian and Middle East countries not prioritizing LTCFs in their plans and rollouts. In contrast, while not prioritizing its elderly population in general, Russia did prioritize vaccinations at LTCFs for elderly people before moving to universal eligibility.
Variation in prioritization and eligibility (V1 and V2) of elderly people and LTCFs (elderly homes) for COVID-19 vaccination before universal eligibility (16/18+ yr vaccine dependent) for COVID-19 vaccination. Following ‘universal’ COVID-19 vaccination eligibility (V1) in most countries, eligibility (V2) for infants (0–4 yr) and children (5–15 yr) were added at later dates. Data current to 15 June 2022.
At the younger end of the age scale, children and infants were not included in initial COVID-19 prioritization plans and indeed, the WHO stated that children were a lower priority group as they are less likely to experience serious symptoms27. Clinical research into the safety and efficacy of vaccines in children came later28. Because clinical trials split children into groups of young children (~5–11 yr,) and adolescents (~12–17 yr)29, many countries’ regulatory agencies approved COVID-19 vaccines for children in similar age groups at around the same time as research emerged and as vaccine supplies allowed (Fig. 2). Children 12 and above first became eligible for COVID-19 vaccinations on 6 May 2021 in the territory of Nunavut, Canada, and Bahrain made the COVID-19 vaccine available to children aged 3+ yr on 17 August 2021. As of 15 June 2022, only 12 countries were vaccinating infants (children aged 0–4 yr), 6 being Central and South American countries (Fig. 3), and 26 countries in our dataset have not been recorded as vaccinating children or infants (ages 0–15 yr).
Countries prioritized many professional categories, some of which (for example, healthcare workers) were gendered to varying extents in different countries. Pregnant people were first made eligible for vaccinations in 2021. They were not initially prioritized for COVID-19 vaccination due to a lack of clinical trial data on the effect on unborn children and pregnant people. From January 2020 to 15 June 2022, 21 countries explicitly prioritized pregnant people in their official vaccination rollout plans (V1) (Fig. 4), and 54 out of 185 countries reported specifically administering vaccinations to pregnant people during their vaccination rollouts (V2).
Some countries prioritized certain groups in their published plans (V1), while other countries added eligibility for these groups ad hoc as vaccinations were already underway (V2). This image shows which countries either specifically prioritized or added eligibility for these groups. Data current to 15 June 2022.
Similarly, strikingly few countries have prioritized refugees, migrants and ethnic minorities in their COVID-19 vaccination plans or actual rollouts (Fig. 4), despite reports of disparities in the risk of COVID-19 infections and in health outcomes among these groups30,31,32,33,34. Australia, Brazil, Canada and New Zealand all prioritized Indigenous populations in their plans and administration of COVID-19 vaccines (Aboriginal and Torres Strait Islanders in Australia, Indigenous People, traditional riverine and quilombola communities in Brazil, First Nations in Canada, Māori and Pacific People and their extended families/whanau that care for them in New Zealand). In early June 2021, Greece began a vaccination programme specifically for refugees starting with the island refugee camps, then moving to the mainland camps. Some African countries with high rates of internal migration have prioritized the vaccination of migrants and ‘travellers’ (a term sometimes used for migrants) (Fig. 4)(https://africacenter.org/spotlight/african-migration-trends-to-watch-in-2022/). Many other countries may have made COVID-19 vaccines available to refugees and migrants but may not have explicitly noted this in official documentation.
Vaccine cost and mandates
The dataset reveals that nearly all countries provided the COVID-19 vaccine free of charge to individuals at the point of delivery (V3). From data freely available online from government sources, we observed that Botswana, India, Pakistan and Turkmenistan required a small fee for COVID-19 vaccination from individuals, in some circumstances. In Taiwan, vaccines were free for those meeting eligibility criteria, but individuals could self-fund vaccination in advance of becoming eligible for free vaccines. Some countries enabled individuals to acquire the vaccination privately if they wished or encouraged vaccine tourism in efforts to boost tourism during the pandemic. In late 2021, Russian tourists were accessing free non-Sputnik vaccines in Croatia via specially arranged tours35. Not long after, Russia began to offer their Sputnik COVID-19 vaccine at a cost to tourists (although visas to visit the country were an issue for some)36. Cities and states of the United States, Indonesia, Cuba, the Maldives and the UAE began to use free COVID-19 vaccinations to increase tourism, and travel agencies in the United Kingdom, India and the United States (among others) offered package deals for individuals not yet eligible in their own country to access the vaccine in another37,38,39. These cases are not recorded in our V3 ordinal indicator data but are captured in qualitative coding notes within the dataset.
We define mandatory COVID-19 vaccination as a government policy requirement to be vaccinated against COVID-19 to work in a specific occupation, or for a specific age group of citizens to be vaccinated. We see these policies as distinct from COVID-19 passports or certification to gain entry to non-essential services or for international travel based on demonstrating immunity or negative test results. These ‘passport’ style policies are defined in the OxCGRT database as ‘differentiated policies’ and are part of the OxCGRT Non-Pharmaceutical Intervention (NPI) dataset8,40. For 10 of these original indicators, we report two policies, one for vaccinated and another for non-vaccinated individuals, viewing requirements to present passes as a de facto closure (see online documentation and Methods for further detail).
COVID-19 vaccine mandates (V4) were first introduced in Jakarta, Indonesia, in February 2021 for all adults41. As of 15 June 2022, 55 countries (29%) of our dataset have currently, or had at one time, at least one vaccine mandate policy. Figure 5 shows that mandatory vaccination policies accelerated in implementation around July 2021, commonly according to occupation (83%), with age-based mandates being far less widespread (17%).
Introduction of mandatory COVID-19 vaccine (V4) for occupational groups, general population (captured if any age group mandated) and vulnerable groups and/or socially vulnerable groups (refer to Table 2 for specific categories). The nations that introduced mandatory vaccinations are grouped by World Bank income groupings. Data current to 15 June 2022.
The most common groups to have been mandated for COVID-19 vaccination were related to occupation: government officials (36), healthcare workers (29), staff at LTCFs (15) and educators (22). Hence, in most countries, mandates only affected a small and specific proportion of the population, as opposed to COVID-19 passports which affected the whole population to control their access to services. Six countries (Germany, Ethiopia, Kuwait, New Zealand, Russia and Tonga) mandated vaccines for socially vulnerable and or other vulnerable populations (see Table 2). Nine countries, including Indonesia, Tajikistan and Turkmenistan mandated COVID-19 vaccination for the entire adult population. Ecuador mandated vaccination for all those over 5 yr and in Costa Rica, all those aged 3–18 yr must be vaccinated ("×" symbol in Fig. 5). The qualitative notes section of this new vaccine dataset records how some countries introduced specific vaccine mandates for particular groups relevant to their local context, such as those observing the Hajj in Saudi Arabia, Jahh in Bangladesh, and maritime and port workers in Singapore.
Discussion
Systematic tracking of COVID-19 vaccination policies and their variation is critical to understand and compare the strategies that countries undertook, and to learn lessons for future pandemics and ongoing vaccination needs. However, collecting such data presented certain challenges due to the complexity and specific considerations of each country/government. We review and address some of these limitations in this section.
First, not all vaccination documents and details are publicly accessible, and language translation barriers are common. As such, recorded sources may range from publicly available news sources, and in some instances, the social media accounts of governments. The detailed notes we have published alongside all entries contain archived sources for future reference and for confirmation of policies.
Second, translating and interpreting heterogeneous policies into the broad categories requires contextual judgement on the part of our specially trained data contributors. As a result, similar policies risk varying interpretations. An initial exercise to determine contributor interpretation variance determined that 90% of entries were consistently interpreted (see Methods).
Third, the 52 categories selected for the V1–V4 indicators (16 general age categories, 14 at-risk age categories and 22 health and occupational categories) are not exhaustive; as such, we publish a ‘best fit’ table in our interpretation guide to aid the classification of groups of people into our categories (https://github.com/OxCGRT/covid-policy-tracker/blob/master/documentation/interpretation_guide.md) (see also Supplementary Table 4). Referral to the detailed qualitative notes may provide more context for which group has been prioritized/made eligible for COVID-19 vaccination.
Fourth, we record an age range as prioritized and/or eligible and/or mandated (V1/V2/V4) if any age within that range is prioritized, eligible for, or mandated to be vaccinated. For example, if 10-yr-olds are prioritized, we would publish ‘5–15 yr young people’ for V1. This choice demonstrates the trade-off between granularity and excess complexity. Therefore, the presence of the ‘5–15 yr young people’ age range category could mean everyone 5+ yr are prioritized, or only people aged 15 yr. Detailed notes in the dataset indicate more granular age floors.
Finally, some vaccination policies apply only in targeted geographic regions. To deal with this variation, we do not require jurisdiction-wide application to code a policy as existing. Instead, if a category of people were prioritized or made eligible for a COVID-19 vaccination in a targeted region of a jurisdiction, they are recorded in our database for the whole jurisdiction. This means that data recorded may not represent the entire jurisdiction. These decisions are detailed in qualitative notes. The dataset includes subnational vaccine policy data for some of the countries with the greatest subnational variation, such as the United States.
Methods
In this section we describe the design, structure, collection, publication and review of the panel dataset of COVID-19 vaccine policies, with the jurisdiction–day as the unit of analysis. All OxCGRT data are available on GitHub and are licensed under the Creative Commons Attribution CC BY standard. Data users should refer to the project website for updated documentation and methodologies (https://github.com/OxCGRT/covid-policy-tracker). Excel (v.16), Stata (v.17.0) and R (v.4.1.3) software were used for all analysis and images produced in this resource article.
Indicators
In late 2020, the OxCGRT team began to consider the COVID-19 vaccine policies and strategies that might be deployed globally. Extensive consultations with government officials, policymakers, experts and stakeholders in the relevant fields, consideration of critical gaps in existing data at the time, and capacity to collect such information resulted in a focus on four priority policies to measure (vaccine indicators V1–V4): who was prioritized for vaccines, who was eligible and receiving vaccines and in what order, who was paying for vaccines, and who was mandated to be vaccinated. Additional indicators for future consideration could include which vaccines were approved/deployed in each country, prioritization for additional/booster vaccinations, vaccine dose timing (manufacturer recommendations vs timeline chosen by country for subsequent doses), government vaccination incentives, vaccination education strategies/programmes and internal vs external funding for vaccines.
Vaccine prioritization (V1) records the ranked position for different groups within a country’s prioritization plan. This is the official plan of the official order in which categories are to be vaccinated. This is recorded regardless of whether a country has capacity to distribute and administer vaccines. Vaccination eligibility/availability (V2) is a categorical/binary variable that records which categories of people, regardless of their position in a prioritized rollout plan, are currently receiving vaccinations. This is recorded as a non-zero value if there is evidence that people in this category are being vaccinated, whether this is happening in a targeted geographical region or nationwide. There must be de facto evidence that this is happening to record a non-zero value in V2. For ‘elderly’ groups, we used local elderly age definitions using qualitative notes where available. In the absence of local guidance on elderly age range, a default of 65+ yr was used. Vaccine financial support (V3) is recorded on an ordinal scale. It reports how vaccines are funded for each category selected in V2 as currently receiving vaccination (1 for full cost to individual, 2 for partially funded by government, 3 for fully funded by government/free). Mandatory vaccination (V4) is a binary variable which reports the existence of a requirement for a category of people to be vaccinated. These are government policy requirements to be vaccinated against COVID-19 to work in a specific occupation, or for a specific group to be vaccinated. This is a mandatory vaccination required as part of occupation or citizenship, and we do not record policies that only ‘encourage’ voluntary vaccination to access non-essential services, facilities or freedoms. For example, if healthcare workers must be vaccinated to attend their place of work, this is recorded in V4. As detailed in our interpretation guidance, if there is a vaccine mandate in place for workers of certain occupations, and non-vaccinated people in this occupation have the option of testing regularly to opt out of vaccination, we still record this as a mandate in V4. If vaccination is mandatory in a subnational region as a result of an official national or local government policy, we record this in V4. We do not report enforcement of vaccine mandates, just the policy.
The vaccination policy dataset also contains summary indicators. These use an ordinal scale to report one number per indicator to offer a succinct summary on the basis of data entered for variables in the main V1–V4 dataset. These are summarized in our codebook (see Supplementary Information). V2, V3 and V4 policies are reported as non-zero values on the date when the policy came into effect, as opposed to the date they were announced. We report the V1 government rollout prioritization plan on the date the policy was published. For the analysis in this paper, the detailed qualitative notes section was used to manually find specific age floors for when different ages became eligible for vaccination, rather than using the age ranges in the quantitative data due to the limitations described above.
In March 2022, the OxCGRT NPI dataset and data structure was altered to reflect the different policies for unvaccinated and vaccinated people (for COVID-19), where passes or proof of either negative testing or vaccination were required to access different areas of public life (https://github.com/OxCGRT/covid-policy-scratchpad/tree/master/differentiated_vaccination_policies). For ten indicators (C1–8, H6 and H8), both the policy values for non-vaccinated and vaccinated people are reported if there are different policies in place. If there is no differentiation, one value is reported. These differentiated values relate only to ‘voluntary access’ to elements of public life, such as attending large events or entertainment and dining venues, which are controlled by testing, evidence of previous immunity or vaccination status through a form of certification or proof.
It is valuable to record both mandatory vaccine policies and voluntary vaccine pass/passport policies. This differentiated coding is reported in our NPI dataset with ‘V’ and ‘NV’ designations (for example, ‘C1V_School closing’ and C1NV_School closing’) and is distinct from the ‘V4 - mandatory vaccination’ indicator reported in this paper.
Data collection
We collected and published data on publicly available sources, which are freely available through internet searches. These are found on government websites, policy briefs and reputable news outlets. The best-quality sources are original policy documents and high-quality media outlets. These sources are codified into the OxCGRT data protocol and entered into the database. A detailed qualitative note (written in English) and web-archived source are provided for context.
The V1–V4 data for the national dataset were initially collected by OxCGRT researchers and a small group of experienced and specially trained volunteer data collectors who received specific training. As of 1 January 2022, data collection for V1–V4 was integrated into the core OxCGRT data collection process, which involves an international team of hundreds of volunteer data collectors covering 90+ unique languages. Where language was a barrier, and where English sources could not be found, local speakers from the pool of OxCGRT contributors were consulted, or translation tools such as Google Translate were utilized. The majority of data collectors are/were postgraduate students at universities around the world. Each data collector completed a bespoke online e-learning course, which took around 45 min to complete, covering the V1–V4 indicators, key coding interpretation points and data quality. Every week of data collection was reviewed by a member of the OxCGRT team for quality and accuracy, and was further reviewed by a trained V1–V4 specific volunteer reviewer (also trained via a bespoke reviewer training e-learning course) and confirmed in the database over the medium to longer term. On GitHub, we published both a codebook and an interpretation guide to standardize interpretation and ensure that all coders were making the same logical choices for data entry. We also published a ‘best fit’ table which records where categories have been substituted when there is a category announced in a policy that is not listed in V1/2, ensuring the standardization of ‘best fit’ interpretation (Supplementary Table 4). This highlights the importance of the ‘notes’ function for each indicator, enabling an in-depth qualitative analysis of the data beyond the numerical summaries. Qualitative notes in our comma-separated values files (CSVs) can be used to find archived original policy documents and specific groups prioritized in each country if a best fit has been used.
Data publication and summary indicators
The data are published in a standalone ‘Vaccines_full.csv’ on GitHub, which includes all the 52 categories for V1–V4. They are also summarized in 9 summary indicators, which report one single number for V1 (vaccination prioritization), V2 (vaccination eligibility/availability) categories (overall summary, general population age floor, at-risk age floor, medically clinically vulnerable (non-elderly), education, frontline workers (non-healthcare), frontline workers (healthcare)) and V3. These summary indicators are included in most of our data CSVs on GitHub, including the NPI dataset ‘OxCGRT_nat_latest.csv’. The data are published in real time and updated each week by the team of international data collectors.
Independent data quality check
We conducted a data quality and accuracy check, where two core team researchers checked the data and original source material for 100 randomly selected data entry points, focusing on the period of time when the majority of new policies and policy changes were being made, and during which the majority of data were entered for all four vaccination policy indicators. The researchers independently verified that 90% of the original data entries in the database were correct, by analysing original source material and checking this alongside the database entries. The remaining 10 entries were corrected. Specifics such as date of announcement vs date of policy effect, accuracy of selected groups and ages, and ensuring that any recorded mandates were in fact government mandates were among the various checks in this independent data quality review process.
As part of the weekly data update cycle, a small team of specially trained reviewers are tasked with checking and confirming data entered. As part of this review process, changes to the data are made retroactively, meaning values on past dates may change. As a result, we recommend downloading the most recent data and stating the download date when using them for analysis. The data used for this paper up to 15 June 2022 have been checked thoroughly by the authors. On the rare occasion where data could not be verified or confirmed by local sources, or via translation, they were not included. An unintentional consequence of this is that a group that was prioritized/eligible/mandated to receive a COVID-19 vaccine may not have been captured by our dataset.
Comparison to other data sources
We do not know of any other datasets publishing systematic data on COVID-19 vaccine policies. This unique source therefore adds considerable value to other datasets. For example, the Reuters COVID-19 vaccination tracker, although no longer updating data, reported the prioritization plan (similar to V1 - vaccine prioritization), availability and eligibility (similar to V2 - vaccination eligibility/availability) of different groups for vaccination in each country, although this does not provide the original archived source material, dates or a time series dataset to evidence when groups became eligible (https://www.reuters.com/graphics/world-coronavirus-tracker-and-maps/vaccination-rollout-and-access/). The Africa CDC Vaccine Dashboard also reports the date vaccination campaign commenced (similar to V2) in African nations, although it does not provide original archived source material, or state when which groups began to receive vaccines (https://africacdc.org/covid-19-vaccination/). Coronanet includes questions on the number of priority groups for vaccine distribution (similar to V1) but only through 2021 (https://www.coronanet-project.org/assets/CoronaNet_Codebook.pdf).
Vaccine policy data are particularly useful when combined with information on the number of vaccine doses administered. For example, the OxCGRT vaccine policy data are displayed as part of Our World in Data’s COVID-19 vaccinations website resource3, which combines country-specific vaccination data into a single resource. Our data can be compared to variables such as proportion of the population that has received one dose, vaccination uptake rates and number of doses administered, to consider the effects of vaccination policies on these. Our H7 indicator, which is a summary of our V2 vaccination policy indicator, is also displayed here. The data are also used by the United Nations Development Programme (UNDP) and WHO’s Global Dashboard for Vaccine Equity (https://data.undp.org/vaccine-equity/), demonstrating their value in informing an interactive accessible tool to reflect the data on the COVID-19 rollout to ensure equitable access.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
The vaccine policy data are available on GitHub (use the download tab to download linked file): https://github.com/OxCGRT/covid-policy-tracker/blob/master/data/OxCGRT_vaccines_full.csv All other information (including methodology and documentation) is available at https://github.com/OxCGRT.
References
Halasa, N. B. et al. Maternal vaccination and risk of hospitalization for Covid-19 among infants. N. Engl. J. Med. 387, 109–119 (2022).
Tanne, J. H. Covid-19: Moderna will ask for authorisation for vaccine for infants and children. BMJ https://doi.org/10.1136/bmj.o798 (2022).
Mathieu, E. et al. A global database of COVID-19 vaccinations. Nat. Hum. Behav. 5, 947–953 (2021).
Baden, L. R. et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N. Engl. J. Med. 384, 403–416 (2021).
Haas, E. J. et al. Impact and effectiveness of mRNA BNT162b2 vaccine against SARS-CoV-2 infections and COVID-19 cases, hospitalisations, and deaths following a nationwide vaccination campaign in Israel: an observational study using national surveillance data. Lancet 397, 1819–1829 (2021).
Ledford, H. Six months of COVID vaccines: what 1.7 billion doses have taught scientists. Nature 594, 164–167 (2021).
Fonseca, E. M. D., Shadlen, K. C. & Bastos, F. I. The politics of COVID-19 vaccination in middle-income countries: lessons from Brazil. Soc. Sci. Med. 281, 114093 (2021).
Hale, T. et al. A global panel database of pandemic policies (Oxford COVID-19 Government Response Tracker). Nat. Hum. Behav. 5, 529–538 (2021).
Emanuel, E. J. et al. An ethical framework for global vaccine allocation. Science 369, 1309–1312 (2020).
Kominers, S. D. & Tabarrok, A. Vaccines and the Covid-19 pandemic: lessons from failure and success. Oxf. Rev. Econ. Policy 38, 719–741 (2022).
Helliwell, J. F., Huang, H., Wang, S. & Norton, M. in World Happiness Report, 2021 Ch. 2 (WER, 2021); https://worldhappiness.report/ed/2021/happiness-trust-and-deaths-under-covid-19/
Oliu-Barton, M. et al. SARS-CoV-2 elimination, not mitigation, creates best outcomes for health, the economy, and civil liberties. Lancet 397, 2234–2236 (2021).
Asia Pacific Strategy for Emerging Diseases and Public Health Emergencies: Advancing Implementation of the International Health Regulations (2005): Working Together Towards Health Security (World Health Organization, Regional Office for the West Pacific, 2017).
Baker, M. G., Wilson, N. & Blakely, T. Elimination could be the optimal response strategy for covid-19 and other emerging pandemic diseases. Brit. Med. J. https://doi.org/10.1136/bmj.m4907 (2020).
Kousi, T. et al. COVID-19 pandemic in Africa’s island nations during the first 9 months: a descriptive study of variation in patterns of infection, severe disease, and response measures. BMJ Glob. Health 7, e006821 (2022).
Jefferies, S. et al. COVID-19 in New Zealand and the impact of the national response: a descriptive epidemiological study. Lancet Public Health 5, e612–e623 (2020).
Henrickson, M. Kiwis and COVID-19: the Aotearoa New Zealand response to the global pandemic. Int. J. Community Soc. Dev. 2, 121–133 (2020).
Fouda, A., Mahmoudi, N., Moy, N. & Paolucci, F. The COVID-19 pandemic in Greece, Iceland, New Zealand, and Singapore: health policies and lessons learned. Health Policy Technol. 9, 510–524 (2020).
Aknin, L. B. et al. Policy stringency and mental health during the COVID-19 pandemic: a longitudinal analysis of data from 15 countries. Lancet Public Health 7, e417–e426 (2022).
Kuehn, B. M. High-income countries have secured the bulk of COVID-19 vaccines. JAMA 325, 612 (2021).
Mutombo, P. N. et al. COVID-19 vaccine hesitancy in Africa: a call to action. Lancet Glob. Health 10, e320–e321 (2022).
Solís Arce, J. S. et al. COVID-19 vaccine acceptance and hesitancy in low- and middle-income countries. Nat. Med. 27, 1385–1394 (2021).
Aw, J., Seng, J. J. B., Seah, S. S. Y. & Low, L. L. COVID-19 vaccine hesitancy—a scoping review of literature in high-income countries. Vaccines 9, 900 (2021).
Mesa-Vieira, C., Botero-Rodríguez, F., Padilla-Muñoz, A., Franco, O. H. & Gómez-Restrepo, C. The Dark Side of the Moon: global challenges in the distribution of vaccines and implementation of vaccination plans against COVID-19. Maturitas 149, 37–39 (2021).
Acharya, K. P., Ghimire, T. R. & Subramanya, S. H. Access to and equitable distribution of COVID-19 vaccine in low-income countries. npj Vaccines 6, 54 (2021).
Ren, P. Life quality in care homes: Chinese and Danish older adults’ perspectives. Curr. Psychol. https://doi.org/10.1007/s12144-022-02921-6 (2022).
Episode #42 – vaccines and children. WHO’s Science in 5 on COVID-10 http://www.who.int/emergencies/diseases/novel-coronavirus-2019/media-resources/science-in-5/episode-42---vaccines-and-children (2021).
First COVID-19 vaccine approved for children aged 12 to 15 in EU. European Medicines Agency https://www.ema.europa.eu/en/news/first-covid-19-vaccine-approved-children-aged-12-15-eu (2021).
Interim Recommendations for Use of the Pfizer-BioNTech COVID-19 Vaccine, BNT162b2, under Emergency Use Listing: Interim Guidance (WHO, 2021); https://apps.who.int/iris/handle/10665/341786
Kirby, T. Evidence mounts on the disproportionate effect of COVID-19 on ethnic minorities. Lancet Resp. Med. 8, 547–548 (2020).
Iacobucci, G. Covid-19: increased risk among ethnic minorities is largely due to poverty and social disparities, review finds. Brit. Med. J. https://doi.org/10.1136/bmj.m4099 (2020).
Mathur, R. et al. Ethnic differences in SARS-CoV-2 infection and COVID-19-related hospitalisation, intensive care unit admission, and death in 17 million adults in England: an observational cohort study using the OpenSAFELY platform. Lancet 397, 1711–1724 (2021).
The Impact of COVID-19 on Indigenous Peoples Policy Brief No.70 (UN-DESA, 2020); https://www.un.org/development/desa/dpad/wp-content/uploads/sites/45/publication/PB_70.pdf
Bohnet, H. & Rüegger, S. Refugees and Covid‐19: beyond health risks to insecurity. Schweiz. Z. Polit. 27, 353–368 (2021).
Grgurinovic, M. Russian ‘COVID-19 Tourists’ flood Croatia seeking jabs. Balkan Insight https://balkaninsight.com/2021/11/19/russian-covid-tourists-flood-croatia-seeking-jabs/ (2021).
These countries are now offering COVID-19 vaccines for tourists. Schengen Visa News https://www.schengenvisainfo.com/news/these-countries-are-now-offering-covid-19-vaccines-for-tourists/ (2021).
Vaccine tourism: COVID-19 vaccine disparities spurring a new model of medical travel. Medical Tourism Magazine https://www.magazine.medicaltourism.com/article/vaccine-tourism-covid-19-vaccine-inequity-spurring-a-new-model-of-medical-travel (2021).
Abu Dhabi opens up free COVID-19 vaccines to tourists. Reuters https://www.reuters.com/world/middle-east/abu-dhabi-opens-up-free-covid-19-vaccines-tourists-2021-06-22/ (2021).
Kaewkitipong, L., Chen, C. & Ractham, P. Examining factors influencing COVID-19 vaccine tourism for international tourists. Sustainability 13, 12867 (2021).
Hale, T. et al. Variation in Government Responses to COVID-19. Version 14.1 Blavatnik School of Government Working Paper (BSG, Univ. of Oxford, 2022); https://www.bsg.ox.ac.uk/sites/default/files/2022-08/BSG-WP-2020-032-v14.1.pdf
Arys, A. & Claire, J. Indonesia to punish those who refuse to take COVID-19 vaccine. Bloomberg https://www.bnnbloomberg.ca/indonesia-to-punish-those-who-refuse-to-take-covid-19-vaccine-1.1565097 (2021).
Acknowledgements
We thank the Oxford Martin School at the University of Oxford for funding the vaccination policy indicator design and collection; our research colleagues on the project, M. DiFolco, R. Nagesh, R. Barnes and M. Luciano; our database and software developer, T. Boby; our project manager, J. Elms; and our large team of dedicated volunteer data collectors who have committed thousands of hours to data collection and without whom we would not have been able to do it. A full list of volunteers is available at https://www.bsg.ox.ac.uk/research/covid-19-government-response-tracker. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
E.C.-B. and H.T. conceptualized the project. E.C.-B., H.T., K.G., H.Z., A. Pott, A.W. and T.B. curated the data. E.C.-B., H.T., B.A. and K.G. conducted formal data analysis. E.C.-B. and H.T. developed the methodology. E.C.-B., H.T. and B.A. provided resources. E.C.-B. and H.T. wrote the original draft. E.C.-B., H.T., B.A, A. Petherick, T.H. and T.P. edited the manuscript. A. Petherick, T.H. and T.P. supervised the project. All named authors read and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Human Behaviour thanks Katie Attwell, Elizabeth King and Jugal Kishore for their contribution to the peer review of this work. Peer reviewer reports are available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Tables 1–4. Detailed codebook description, best fit table for vaccine categories and full eliminator vs mitigator table.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cameron-Blake, E., Tatlow, H., Andretti, B. et al. A panel dataset of COVID-19 vaccination policies in 185 countries. Nat Hum Behav 7, 1402–1413 (2023). https://doi.org/10.1038/s41562-023-01615-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41562-023-01615-8
This article is cited by
-
COVID-19 vaccination policy dataset
Nature Human Behaviour (2023)