Abstract
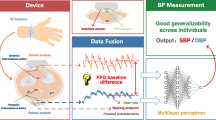
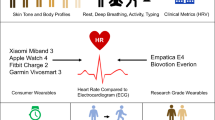
Cardiovascular health is typically monitored by measuring blood pressure. Here we describe a wireless on-skin system consisting of synchronized sensors for chest electrocardiography and peripheral multispectral photoplethysmography for the continuous monitoring of metrics related to vascular resistance, cardiac output and blood-pressure regulation. We used data from the sensors to train a support-vector-machine model for the classification of haemodynamic states (resulting from exposure to heat or cold, physical exercise, breath holding, performing the Valsalva manoeuvre or from vasopressor administration during post-operative hypotension) that independently affect blood pressure, cardiac output and vascular resistance. The model classified the haemodynamic states on the basis of an unseen subset of sensor data for 10 healthy individuals, 20 patients with hypertension undergoing haemodynamic stimuli and 15 patients recovering from cardiac surgery, with an average precision of 0.878 and an overall area under the receiver operating characteristic curve of 0.958. The multinodal sensor system may provide clinically actionable insights into haemodynamic states for use in the management of cardiovascular disease.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$99.00 per year
only $8.25 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
The data used for the training of the classification model are presented in its entirety in Fig. 5 and are available from the corresponding authors on reasonable request and Institutional Review Board approval.
Code availability
Code used for analysis and to produce figures is also available upon reasonable request to the corresponding authors; however, implementations of methods described in the text exist in public repositories described in the data analysis section and in referenced work.
References
Heidenreich, P. A. et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 79, e263–e421 (2022).
January, C. T. et al. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society in Collaboration With the Society of Thoracic Surgeons. Circulation 140, e125–e151 (2019).
Truby, L. K. & Rogers, J. G. Advanced heart failure: epidemiology, diagnosis, and therapeutic approaches. Heart Fail. 8, 523–536 (2020).
Pinsky, M. R. & Payen, D. Functional hemodynamic monitoring. Crit. Care 9, 566–572 (2005).
Teboul, J. L. et al. Less invasive hemodynamic monitoring in critically ill patients. Intensive Care Med. 42, 1350–1359 (2016).
Cotter, G. et al. The role of cardiac power and systemic vascular resistance in the pathophysiology and diagnosis of patients with acute congestive heart failure. Eur. J. Heart Fail. 5, 443–451 (2003).
Delong, C. & Sharma, S. Physiology, Peripheral Vascular Resistance (StatPearls Publishing, 2022).
Keville, M. P. et al. Arterial or cuff pressure: clinical predictors among patients in shock in a critical care resuscitation unit. Am. J. Emerg. Med. 46, 109–115 (2021).
Tran, Q. K. et al. Discrepancy between invasive and noninvasive blood pressure measurements in patients with sepsis by vasopressor status. West. J. Emerg. Med. 23, 358–367 (2022).
Chen, Y. et al. Right heart catheterization-related complications: a review of the literature and best practices. Cardiol. Rev. 28, 36–41 (2020).
Desai, A. S. et al. Ambulatory hemodynamic monitoring reduces heart failure hospitalizations in ‘real-world’ clinical practice. J. Am. Coll. Cardiol. 69, 2357–2365 (2017).
Abraham, J. et al. Association of ambulatory hemodynamic monitoring of heart failure with clinical outcomes in a concurrent matched cohort analysis. JAMA Cardiol. 4, 556–563 (2019).
Malasinghe, L. P., Ramzan, N. & Dahal, K. Remote patient monitoring: a comprehensive study. J. Ambient Intell. Humaniz. Comput. 10, 57–76 (2019).
Noah, B. et al. Impact of remote patient monitoring on clinical outcomes: an updated meta-analysis of randomized controlled trials. npj Digital Med. 1, 20172 (2018).
Yetisen, A. K. et al. Wearables in medicine. Adv. Mater. 30, 1706910 (2018).
Olmedo-Aguirre, J. O. et al. Remote healthcare for elderly people using wearables: a review. Biosensors 12, 73 (2022).
Bayoumy, K. et al. Smart wearable devices in cardiovascular care: where we are and how to move forward. Nat. Rev. Cardiol. 18, 581–599 (2021).
Pevnick, J. M., Birkeland, K., Zimmer, R., Elad, Y. & Kedan, I. Wearable technology for cardiology: an update and framework for the future. Trends Cardiovasc. Med. 28, 144–150 (2018).
Prieto-Avalos, G. et al. Wearable devices for physical monitoring of heart: a review. Biosensors 12, 292 (2022).
Huhn, S. et al. The impact of wearable technologies in health research: scoping review. JMIR Mhealth Uhealth 10, e34384 (2022).
Boubouchairopoulou, N., Ntineri, A., Kollias, A., Destounis, A. & Stergiou, G. S. Blood pressure variability assessed by office, home, and ambulatory measurements: comparison, agreement, and determinants. Hypertens. Res. 44, 1617–1624 (2021).
Stergiou, G. S. et al. Hypertension evaluation of the accuracy of cuffless blood pressure measurement devices: challenges and proposals. Hypertension 78, 1161–1167 (2021).
Stergiou, G. S. et al. Cuffless blood pressure measuring devices: review and statement by the European Society of Hypertension Working Group on Blood Pressure Monitoring and Cardiovascular Variability. J. Hypertens. 40, 1449–1460 (2022).
Schutte, A. E., Kollias, A. & Stergiou, G. S. Blood pressure and its variability: classic and novel measurement techniques. Nat. Rev. Cardiol. 19, 643–654 (2022).
Stergiou, G. S. et al. Methodology and technology for peripheral and central blood pressure and blood pressure variability measurement: current status and future directions – position statement of the European Society of Hypertension Working Group on blood pressure monitoring and cardiovascular variability. J. Hypertens. 34, 1665–1677 (2016).
Ma, Y. et al. Relation between blood pressure and pulse wave velocity for human arteries. Proc. Natl Acad. Sci. USA 115, 11144–11149 (2018).
Mukkamala, R. et al. Towards ubiquitous blood pressure monitoring via pulse transit time: theory and practice HHS public access. IEEE Trans. Biomed. Eng. 62, 1879–1901 (2015).
Wibmer, T. et al. Blood pressure monitoring during exercise: comparison of pulse transit time and volume clamp methods. Blood Press. 24, 353–360 (2015).
Finnegan, E. et al. Pulse arrival time as a surrogate of blood pressure. Sci. Rep. 11, 22767 (2021).
Proença, J., Muehlsteff, J., Aubert, X. & Carvalho, P. Is pulse transit time a good indicator of blood pressure changes during short physical exercise in a young population? Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2010, 598–601 (2010).
Kounalakis, S. N. & Geladas, N. D. The role of pulse transit time as an index of arterial stiffness during exercise. Cardiovasc. Eng. 9, 92–97 (2009).
Polónia, J., Barbosa, L., Silva, J. A. & Maldonado, J. Different influences on central and peripheral pulse pressure, aortic wave reflections and pulse wave velocity of three different types of antihypertensive drugs. Rev. Port. Cardiol. 22, 1485–1492 (2003).
Kelly, R. P., Millasseau, S. C., Ritter, J. M. & Chowienczyk, P. J. Vasoactive drugs influence aortic augmentation index independently of pulse-wave velocity in healthy men. Hypertension 37, 1429–1433 (2001).
Borner, A., Murray, K., Trotter, C. & Pearson, J. Baseline aortic pulse wave velocity is associated with central and peripheral pressor responses during the cold pressor test in healthy subjects. Physiol. Rep. 5, e13357 (2017).
Elias, S. O. & Ajayi, R. E. Effect of sympathetic autonomic stress from the cold pressor test on left ventricular function in young healthy adults. Physiol. Rep. 7, e13985 (2019).
Parati, G., Stergiou, G. S., Dolan, E. & Bilo, G. Blood pressure variability: clinical relevance and application. J. Clin. Hypertens. 20, 1133–1137 (2018).
Lantelme, P., Mestre, C., Lievre, M., Gressard, A. & Milon, H. Heart rate: an important confounder of pulse wave velocity assessment. Hypertension 39, 1083–1087 (2002).
Papaioannou, T. G. et al. The influence of resting heart rate on pulse wave velocity measurement is mediated by blood pressure and depends on aortic stiffness levels: insights from the Corinthia study. Physiol. Meas. 40, 055005 (2019).
Sherwood, A. et al. Methodological guidelines for impedance cardiography. Psychophysiology 27, 1–23 (1990).
Kouz, K., Scheeren, T. W. L., de Backer, D. & Saugel, B. Pulse wave analysis to estimate cardiac output. Anesthesiology 134, 119–126 (2021).
Hametner, B. & Wassertheurer, S. Pulse waveform analysis: is it ready for prime time? Curr. Hypertens. Rep. 19, 1–7 (2017).
Liu, J. et al. Multi-wavelength photoplethysmography method for skin arterial pulse extraction. Biomed. Opt. Express 7, 4313 (2016).
Liu, J. et al. Multi-wavelength photoplethysmography enabling continuous blood pressure measurement with compact wearable electronics. IEEE Trans. Biomed. Eng. 66, 1514–1525 (2019).
Liu, J. et al. PCA-based multi-wavelength photoplethysmography algorithm for cuffless blood pressure measurement on elderly subjects. IEEE J. Biomed. Health Inf. 25, 663–673 (2021).
Spigulis, J., Gailite, L., Lihachev, A. & Erts, R. Simultaneous recording of skin blood pulsations at different vascular depths by multiwavelength photoplethysmography. Appl. Opt. 56, 1754–1759 (2007).
Aidar, F. J. et al. Can post-exercise hemodynamic response be influenced by different recovery methods in paraplegic sportsmen? Int. J. Environ. Res. Public Health 19, 1772 (2022).
Francisco, M. A. et al. Hemodynamics of postexercise versus post-hot water immersion recovery. J. Appl. Physiol. 130, 1362–1372 (2021).
Churchill, T. W. The impact of exercise and athletic training on vascular structure and function. Curr. Treat. Options Cardiovasc. Med. 22, 1–11 (2020).
Bauer, P. et al. Blood pressure response and vascular function of professional athletes and controls. Sports Med. Int. Open 5, E45–E52 (2021).
McDuff, D. et al. Non-contact imaging of peripheral hemodynamics during cognitive and psychological stressors. Sci. Rep. 10, 1–13 (2020).
Chung, H. U. et al. Skin-interfaced biosensors for advanced wireless physiological monitoring in neonatal and pediatric intensive-care units. Nat. Med. 26, 418–429 (2020).
Lee, K. H. et al. Mechano-acoustic sensing of physiological processes and body motions via a soft wireless device placed at the suprasternal notch. Nat. Biomed. Eng. 4, 148–158 (2020).
Finlayson, L. et al. Depth penetration of light into skin as a function of wavelength from 200 to 1000 nm. Photochem. Photobiol. 98, 974–981 (2022).
Rwei, A. Y. et al. A wireless, skin-interfaced biosensor for cerebral hemodynamic monitoring in pediatric care. Proc. Natl Acad. Sci. USA 117, 31674–31684 (2020).
Nishimura, R. A. & Tajik, A. J. The Valsalva maneuver and response revisited. Mayo Clin. Proc. 61, 211–217 (1986).
Bennett, T., Hosking, D. J. & Hampton, J. R. Vasomotor responses to the Valsalva manoeuvre in normal subjects and in patients with diabetes mellitus. Br. Heart J. 42, 422–428 (1979).
Awad, A. A. et al. Different responses of ear and finger pulse oximeter wave form to cold pressor test. Anesth. Analg. 92, 1483–1486 (2001).
Lovallo, W. The cold pressor test and autonomic function: a review and integration. Psychophysiology 12, 268–282 (1975).
Heistad, D. D., Abboud, F. M. & Eckstein, J. W. Vasoconstrictor response to simulated diving in man. J. Appl. Physiol. 25, 542–549 (1968).
Kellogg, D. L., Crandall, C. G., Liu, Y., Charkoudian, N. & Johnson, J. M. Nitric oxide and cutaneous active vasodilation during heat stress in humans. J. Appl. Physiol. 85, 824–829 (1998).
Kim, M. Y. et al. Acute reduction of pulse wave velocity after sauna in adults in a community. J. Korean Acad. Fam. Med. 27, 384–390 (2006).
Lee, E. et al. Sauna exposure leads to improved arterial compliance: findings from a non-randomised experimental study. Eur. J. Prev. Cardiol. 25, 130–138 (2018).
Laukkanen, T. et al. Acute effects of sauna bathing on cardiovascular function. J. Hum. Hypertens. 32, 129–138 (2017).
Teixeira, L., Ritti-Dias, R. M., Tinucci, T., Mion, D. & de Moraes Forjaz, C. L. Post-concurrent exercise hemodynamics and cardiac autonomic modulation. Eur. J. Appl. Physiol. 111, 2069–2078 (2011).
Vatner, S. F. & Pagani, M. Cardiovascular adjustments to exercise: hemodynamics and mechanisms. Prog. Cardiovasc. Dis. 19, 91–108 (1976).
Desebbe, O. et al. Control of postoperative hypotension using a closed-loop system for norepinephrine infusion in patients after cardiac surgery: a randomized trial. Anesth. Analg. 134, 964–973 (2022).
Klabunde, R. E. Cardiovascular Physiology Concepts (Wolters Kluwer, Lippincott Williams & Wilkins, 2021).
Hofmann, H., Wickham, H. & Kafadar, K. Letter-value plots: boxplots for large data. J. Comput. Graph. Stat. 26, 469–477 (2017).
Brunner, E. & Munzel, U. Rank-score tests in factorial designs with repeated measures. J. Multivar. Anal. 70, 286–317 (1999).
Mitchell, L. A., MacDonald, R. A. R. & Brodie, E. E. Temperature and the cold pressor test. J. Pain 5, 233–237 (2004).
Reddy, S. Explainability and artificial intelligence in medicine. Lancet Digit. Health 4, e214–e215 (2022).
Lundberg, S. M., Allen, P. G. & Lee, S.-I. A unified approach to interpreting model predictions. Adv. Neural Inf. Process. Syst. 30, 4765–4774 (2017).
Newlin, D. B. & Levenson, R. W. Pre-ejection period: measuring beta-adrenergic influences upon the heart. Psychophysiology 16, 546–552 (1979).
Garrard, C. L., Weissler, A. M. & Dodge, H. T. The relationship of alterations in systolic time intervals to ejection fraction in patients with cardiac disease. Circulation 42, 455–462 (1970).
Harris, C. R. et al. Array programming with NumPy. Nature 585, 357–362 (2020).
Virtanen, P. et al. SciPy 1.0: fundamental algorithms for scientific computing in Python. Nat. Methods 17, 261–272 (2020).
McKinney, W. Data structures for statistical computing in Python. In Proc. 9th Python in Science Conf. (eds van der Walt, S. & Millman, K. J.) 56–61 (2010).
Pedregosa, F. et al. Scikit-learn: machine learning in Python. J. Mach. Learn. Res. 12, 2825–2830 (2011).
Hunter, J. D. Matplotlib: a 2D graphics environment. Comput. Sci. Eng. 9, 90–95 (2007).
Waskom, M. seaborn: statistical data visualization. J. Open Source Softw. 6, 3021 (2021).
Maeda, Y., Sekine, M. & Tamura, T. The advantages of wearable green reflected photoplethysmography. J. Med. Syst. 35, 829–834 (2011).
Lee, J. et al. Comparison between red, green and blue light reflection photoplethysmography for heart rate monitoring during motion. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2013, 1724–1727 (2013).
Scholkmann, F., Boss, J. & Wolf, M. An efficient algorithm for automatic peak detection in noisy periodic and quasi-periodic signals. Algorithms 5, 588–603 (2012).
Acknowledgements
We thank M. Banet and J. Martucci for their invaluable expertise and insights throughout the development and execution of this project. A.T. discloses support for the research described in this study from the National Heart, Lung and Blood Institute of the National Institutes of Health (grant number F30HL157066). The work was also supported in part by the National Center for Advancing Translational Sciences (NCATS; grant UM1TR004407 to J.P.).
Author information
Authors and Affiliations
Contributions
A.T. and D.F. conceptualized the work. A.T., D.F., J.Y.L., H.A., J.T., H.U.C., S.S.K. and C.W. developed the methodology. A.T., D.F., H.A., Y.L., I.H., M.R., J.W., H.L. and J.P. performed experiments. A.T. and D.F. visualized data. A.T., D.F. and J.A.R acquired funding. J.P., F.S.A., P.M.M. and J.A.R. supervised the project. A.T. and D.F. wrote the manuscript. A.T., D.F., J.P., F.S.A. and J.A.R. edited the manuscript.
Corresponding authors
Ethics declarations
Competing interests
J.Y.L., H.U.C. and J.A.R. own equity in Sibel Health and hold patents (US20210361165A1, USA 2021 pending; US20210386300A1, USA 2021 pending; WO2023043866A1, WIPO 2023) associated with this company. The other authors declare no competing interests.
Peer review
Peer review information
Nature Biomedical Engineering thanks Justin Estepp, Yftach Gepner and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary tables, figures and video captions.
Supplementary Video 1
3D scatterplot showing the grouping of haemodynamic pressors according to sensor data.
Supplementary Video 2
Demonstration of the system.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Franklin, D., Tzavelis, A., Lee, J.Y. et al. Synchronized wearables for the detection of haemodynamic states via electrocardiography and multispectral photoplethysmography. Nat. Biomed. Eng 7, 1229–1241 (2023). https://doi.org/10.1038/s41551-023-01098-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41551-023-01098-y
This article is cited by
-
Motion artefact management for soft bioelectronics
Nature Reviews Bioengineering (2024)
-
Sensing haemodynamics via wearables in sync
Nature Biomedical Engineering (2023)