Abstract
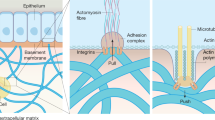
The fibrotic encapsulation of implants involves the mechanical activation of myofibroblasts and of pro-fibrotic transforming growth factor beta 1 (TGF-β1). Here, we show that both softening of the implant surfaces and inhibition of the activation of TGF-β1 reduce the fibrotic encapsulation of subcutaneous silicone implants in mice. Conventionally stiff silicones (elastic modulus, ~2 MPa) coated with a soft silicone layer (elastic modulus, ~2 kPa) reduced collagen deposition as well as myofibroblast activation without affecting the numbers of macrophages and their polarization states. Instead, fibroblasts around stiff implants exhibited enhanced intracellular stress, increased the recruitment of αv and β1 integrins, and activated TGF-β1 signalling. In vitro, the recruitment of αv integrin to focal adhesions and the activation of β1 integrin and of TGF-β were higher in myofibroblasts grown on latency-associated peptide (LAP)-coated stiff silicones than on soft silicones. Antagonizing αv integrin binding to LAP through the small-molecule inhibitor CWHM-12 suppressed active TGF-β signalling, myofibroblast activation and the fibrotic encapsulation of stiff subcutaneous implants in mice.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$99.00 per year
only $8.25 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout








Similar content being viewed by others
Data availability
The main data supporting the results of this study are available within the paper and its Supplementary Information. The data used to produce the figures are available from Figshare with the identifier https://doi.org/10.6084/m9.figshare.14319758. The raw and analysed datasets generated during the study are too large to be publicly shared, but are available for research purposes from the corresponding author upon reasonable request.
Code availability
The custom Fiji (ImageJ) macro used to analyse the recruitment of active β1 integrin to focal adhesions is available on GitHub at https://github.com/NinaNoskovicova/Noskovicova-N.-et-al.-2021-NBE.
References
Majd, H. et al. Novel micropatterns mechanically control fibrotic reactions at the surface of silicone implants. Biomaterials 54, 136–147 (2015).
Visscher, L. E. et al. Breast augmentation and reconstruction from a regenerative medicine point of view: state of the art and future perspectives. Tissue Eng. Part B Rev. 23, 281–293 (2017).
Veiseh, O. & Vegas, A. J. Domesticating the foreign body response: recent advances and applications. Adv. Drug Deliv. Rev. 144, 148–161 (2019).
Klopfleisch, R. & Jung, F. The pathology of the foreign body reaction against biomaterials. J. Biomed. Mater. Res. A 105, 927–940 (2017).
Franz, S., Rammelt, S., Scharnweber, D. & Simon, J. C. Immune responses to implants—a review of the implications for the design of immunomodulatory biomaterials. Biomaterials 32, 6692–6709 (2011).
Morris, A. H. & Kyriakides, T. R. Matricellular proteins and biomaterials. Matrix Biol. 37, 183–191 (2014).
Borenstein, A. & Friedman, O. Combined breast implant explantation and multilevel mastopexy technique. Plast. Reconstr. Surg. Glob. Open 7, e2429 (2019).
Pakshir, P. & Hinz, B.The big five in fibrosis: macrophages, myofibroblasts, matrix, mechanics, and miscommunication. Matrix Biol. 68–69, 81–93 (2018).
Hinz, B. Myofibroblasts. Exp. Eye Res. 142, 56–70 (2016).
Hinz, B., Celetta, G., Tomasek, J. J., Gabbiani, G. & Chaponnier, C. Alpha-smooth muscle actin expression upregulates fibroblast contractile activity. Mol. Biol. Cell 12, 2730–2741 (2001).
Pakshir, P. et al. The myofibroblast at a glance. J. Cell Sci. 133, jcs227900 (2020).
Hinz, B. The extracellular matrix and transforming growth factor-β1: tale of a strained relationship. Matrix Biol. 47, 54–65 (2015).
Lodyga, M. & Hinz, B. TGF-β1—a truly transforming growth factor in fibrosis and immunity. Semin. Cell Dev. Biol. 101, 123–139 (2020).
Annes, J. P., Chen, Y., Munger, J. S. & Rifkin, D. B. Integrin αvβ6-mediated activation of latent TGF-β requires the latent TGF-β binding protein-1. J. Cell Biol. 165, 723–734 (2004).
Shi, M. et al. Latent TGF-β structure and activation. Nature 474, 343–349 (2011).
Henderson, N. C. et al. Targeting of αv integrin identifies a core molecular pathway that regulates fibrosis in several organs. Nat. Med. 19, 1617–1624 (2013).
Sarrazy, V. et al. Integrins αvβ5 and αvβ3 promote latent TGF-β1 activation by human cardiac fibroblast contraction. Cardiovasc. Res. 102, 407–417 (2014).
Munger, J. S. et al. The integrin αvβ6 binds and activates latent TGF-β1: a mechanism for regulating pulmonary inflammation and fibrosis. Cell 96, 319–328 (1999).
Mu, D. et al. The integrin αvβ8 mediates epithelial homeostasis through MT1–MMP-dependent activation of TGF-β1. J. Cell Biol. 157, 493–507 (2002).
Dong, X. et al. Force interacts with macromolecular structure in activation of TGF-β. Nature 542, 55–59 (2017).
Wipff, P. J., Rifkin, D. B., Meister, J. J. & Hinz, B. Myofibroblast contraction activates latent TGF-β1 from the extracellular matrix. J. Cell Biol. 179, 1311–1323 (2007).
Buscemi, L. et al. The single-molecule mechanics of the latent TGF-β1 complex. Curr. Biol. 21, 2046–2054 (2011).
Hillard, C., Fowler, J. D., Barta, R. & Cunningham, B. Silicone breast implant rupture: a review. Gland Surg. 6, 163–168 (2017).
Swezey, E., Shikhman, R. & Moufarrege, R. Breast Implant Rupture (StatPearls, 2020).
Zhu, J. et al. Structure of a complete integrin ectodomain in a physiologic resting state and activation and deactivation by applied forces. Mol. Cell 32, 849–861 (2008).
Goffin, J. M. et al. Focal adhesion size controls tension-dependent recruitment of α-smooth muscle actin to stress fibers. J. Cell Biol. 172, 259–268 (2006).
Klingberg, F. et al. Prestress in the extracellular matrix sensitizes latent TGF-β1 for activation. J. Cell Biol. 207, 283–297 (2014).
Hinz, B., McCulloch, C. A. & Coelho, N. M. Mechanical regulation of myofibroblast phenoconversion and collagen contraction. Exp. Cell Res. 379, 119–128 (2019).
Li, C. X. et al. MicroRNA-21 preserves the fibrotic mechanical memory of mesenchymal stem cells. Nat. Mater. 16, 379–389 (2017).
Achterberg, V. F. et al. The nano-scale mechanical properties of the extracellular matrix regulate dermal fibroblast function. J. Invest. Dermatol. 134, 1862–1872 (2014).
Quesnel, K. et al. CCN1 expression by fibroblasts is required for bleomycin-induced skin fibrosis. Matrix Biol. 3, 100009 (2019).
Paszek, M. J. et al. Tensional homeostasis and the malignant phenotype. Cancer Cell 8, 241–254 (2005).
Avula, M. N., Rao, A. N., McGill, L. D., Grainger, D. W. & Solzbacher, F. Foreign body response to subcutaneous biomaterial implants in a mast cell-deficient Kitw-Sh murine model. Acta Biomater. 10, 1856–1863 (2014).
Duffield, J. S., Lupher, M., Thannickal, V. J. & Wynn, T. A. Host responses in tissue repair and fibrosis. Annu. Rev. Pathol. 8, 241–276 (2013).
Wipff, P. J. et al. The covalent attachment of adhesion molecules to silicone membranes for cell stretching applications. Biomaterials 30, 1781–1789 (2009).
Werner, S., Lutzkendorf, J., Muller, T., Muller, L. P. & Posern, G. MRTF-A controls myofibroblastic differentiation of human multipotent stromal cells and their tumour-supporting function in xenograft models. Sci. Rep. 9, 11725 (2019).
Foster, C. T., Gualdrini, F. & Treisman, R. Mutual dependence of the MRTF–SRF and YAP–TEAD pathways in cancer-associated fibroblasts is indirect and mediated by cytoskeletal dynamics. Genes Dev. 31, 2361–2375 (2017).
Bialik, J. F. et al. Profibrotic epithelial phenotype: a central role for MRTF and TAZ. Sci. Rep. 9, 4323 (2019).
Klingberg, F. et al. The fibronectin ED-A domain enhances recruitment of latent TGF-β-binding protein-1 to the fibroblast matrix. J. Cell Sci. 131, jcs201293 (2018).
Reed, N. I. et al. The αvβ1 integrin plays a critical in vivo role in tissue fibrosis. Sci. Transl. Med. 7, 288ra279 (2015).
Magness, S. T., Bataller, R., Yang, L. & Brenner, D. A. A dual reporter gene transgenic mouse demonstrates heterogeneity in hepatic fibrogenic cell populations. Hepatology 40, 1151–1159 (2004).
Tsukui, T. et al. Collagen-producing lung cell atlas identifies multiple subsets with distinct localization and relevance to fibrosis. Nat. Commun. 11, 1920 (2020).
Murray, I. R. et al. αv integrins on mesenchymal cells regulate skeletal and cardiac muscle fibrosis. Nat. Commun. 8, 1118 (2017).
Sun, Z., Guo, S. S. & Fassler, R. Integrin-mediated mechanotransduction. J. Cell Biol. 215, 445–456 (2016).
Hannan, R. T., Peirce, S. M. & Barker, T. H. Fibroblasts: diverse cells critical to biomaterials integration. ACS Biomater. Sci. Eng. 4, 1223–1232 (2018).
Akilbekova, D. & Bratlie, K. M. Quantitative characterization of collagen in the fibrotic capsule surrounding implanted polymeric microparticles through second harmonic generation imaging. PloS ONE 10, e0130386 (2015).
Tarpila, E., Ghassemifar, R., Fagrell, D. & Berggren, A. Capsular contracture with textured versus smooth saline-filled implants for breast augmentation: a prospective clinical study. Plast. Reconstr. Surg. 99, 1934–1939 (1997).
Stevens, W. G. et al. Risk factor analysis for capsular contracture: a 5-year Sientra study analysis using round, smooth, and textured implants for breast augmentation. Plast. Reconstr. Surg. 132, 1115–1123 (2013).
Shin, B. H. et al. Silicone breast implant modification review: overcoming capsular contracture. Biomater. Res. 22, 37 (2018).
Harvey, A. G., Hill, E. W. & Bayat, A. Designing implant surface topography for improved biocompatibility. Expert Rev. Med. Devices 10, 257–267 (2013).
Wixtrom, R. N., Garadi, V., Leopold, J. & Canady, J. W. Device-specific findings of imprinted-texture breast implants: characteristics, risks, and benefits. Aesthet. Surg. J. 40, 167–173 (2020).
Buonomo, O. C. et al. Comparison of round smooth and shaped micro-textured implants in terms of quality of life and aesthetic outcomes in women undergoing breast reconstruction: a single-centre prospective study. Updates Surg. 72, 537–546 (2020).
Liu, X. et al. Comparison of the postoperative incidence rate of capsular contracture among different breast implants: a cumulative meta-analysis. PloS ONE 10, e0116071 (2015).
Barr, S., Hill, E. W. & Bayat, A. Development, fabrication and evaluation of a novel biomimetic human breast tissue derived breast implant surface. Acta Biomater. 49, 260–271 (2017).
Ramin, M. A., Latxague, L., Sindhu, K. R., Chassande, O. & Barthelemy, P. Low molecular weight hydrogels derived from urea based-bolaamphiphiles as new injectable biomaterials. Biomaterials 145, 72–80 (2017).
Minev, I. R. et al. Biomaterials. Electronic dura mater for long-term multimodal neural interfaces. Science 347, 159–163 (2015).
Schweller, R. M., Wu, Z. J., Klitzman, B. & West, J. L. Stiffness of protease sensitive and cell adhesive PEG hydrogels promotes neovascularization In Vivo. Ann. Biomed. Eng. 45, 1387–1398 (2017).
Moshayedi, P. et al. The relationship between glial cell mechanosensitivity and foreign body reactions in the central nervous system. Biomaterials 35, 3919–3925 (2014).
Sindhu, K. R. et al. New injectable self-assembled hydrogels that promote angiogenesis through a bioactive degradation product. Acta Biomater. 115, 197–209 (2020).
Godbout, C. et al. The mechanical environment modulates intracellular calcium oscillation activities of myofibroblasts. PloS ONE 8, e64560 (2013).
Curtis, J. & Colas, A. in Biomaterials Science 3rd edn (eds Ratner, B. D. et al.) 1106–1116 (Academic Press, 2013).
Mayesh, J. P. & Vicari, A. R. in Biomaterials Science 3rd edn (eds Ratner, B. D. et al.) 1431–1443 (Academic Press, 2013).
Swarts, E., Kop, A. M., Nilasaroya, A., Keogh, C. V. & Cooper, T. Rupture of poly implant prothese silicone breast implants: an implant retrieval study. Plast. Reconstr. Surg. 131, 480e–489e (2013).
Charalambous, M., Daoud, R. & Karat, I. Advances in Medical and Surgical Engineering (eds Ahmed, W. et al.) 141–147 (Academic Press, 2020).
Merkel, R., Kirchgessner, N., Cesa, C. M. & Hoffmann, B. Cell force microscopy on elastic layers of finite thickness. Biophys. J. 93, 3314–3323 (2007).
Buxboim, A., Ivanovska, I. L. & Discher, D. E. Matrix elasticity, cytoskeletal forces and physics of the nucleus: how deeply do cells ‘feel’ outside and in? J. Cell Sci. 123, 297–308 (2010).
Dutta, B., Goswami, R. & Rahaman, S. O. TRPV4 plays a role in matrix stiffness-induced macrophage polarization. Front. Immunol. 11, 570195 (2020).
Scott, R. A., Kiick, K. L. & Akins, R. E. Substrate stiffness directs the phenotype and polarization state of cord blood derived macrophages. Acta Biomater. 122, 220–235 (2021).
Janmey, P. A., Fletcher, D. A. & Reinhart-King, C. A. Stiffness sensing by cells. Physiol. Rev. 100, 695–724 (2020).
Discher, D. E. et al. Matrix mechanosensing: from scaling concepts in ‘omics data to mechanisms in the nucleus, regeneration, and cancer. Annu. Rev. Biophys. 46, 295–315 (2017).
Dondossola, E. et al. Examination of the foreign body response to biomaterials by nonlinear intravital microscopy. Nat. Biomed. Eng. 1, 0007 (2016).
Wynn, T. A. & Vannella, K. M. Macrophages in tissue repair, regeneration, and fibrosis. Immunity 44, 450–462 (2016).
Correa-Gallegos, D. et al. Patch repair of deep wounds by mobilized fascia. Nature 576, 287–292 (2019).
Shook, B. A. et al. Myofibroblast proliferation and heterogeneity are supported by macrophages during skin repair. Science 362, eaar2971 (2018).
Arora, P. D., Narani, N. & McCulloch, C. A. The compliance of collagen gels regulates transforming growth factor-β induction of α-smooth muscle actin in fibroblasts. Am. J. Pathol. 154, 871–882 (1999).
Li, A. G. et al. Elevation of transforming growth factor beta (TGFβ) and its downstream mediators in subcutaneous foreign body capsule tissue. J. Biomed. Mater. Res. A 82, 498–508 (2007).
Kuhn, A. et al. Periprosthetic breast capsules contain the fibrogenic cytokines TGF-β1 and TGF-β2, suggesting possible new treatment approaches. Ann. Plast. Surg. 44, 387–391 (2000).
Higgins, D. M. et al. Localized immunosuppressive environment in the foreign body response to implanted biomaterials. Am. J. Pathol. 175, 161–170 (2009).
DiEgidio, P. et al. Biomedical implant capsule formation: lessons learned and the road ahead. Ann. Plast. Surg. 73, 451–460 (2014).
Mazaheri, M. K., Schultz, G. S., Blalock, T. D., Caffee, H. H. & Chin, G. A. Role of connective tissue growth factor in breast implant elastomer capsular formation. Ann. Plast. Surg. 50, 263–268 (2003).
Park, S. et al. Acute suppression of TGF-β with local, sustained release of tranilast against the formation of fibrous capsules around silicone implants. J. Control. Release 200, 125–137 (2015).
Gancedo, M., Ruiz-Corro, L., Salazar-Montes, A., Rincon, A. R. & Armendariz-Borunda, J. Pirfenidone prevents capsular contracture after mammary implantation. Aesthetic Plast. Surg. 32, 32–40 (2008).
Travis, M. A. & Sheppard, D. TGF-β activation and function in immunity. Annu. Rev. Immunol. 32, 51–82 (2014).
Wipff, P. J. & Hinz, B. Integrins and the activation of latent transforming growth factor β1—an intimate relationship. Eur. J. Cell Biol. 87, 601–615 (2008).
Giacomini, M. M., Travis, M. A., Kudo, M. & Sheppard, D. Epithelial cells utilize cortical actin/myosin to activate latent TGF-β through integrin αvβ6-dependent physical force. Exp. Cell Res. 318, 716–722 (2012).
Hinz, B. It has to be the αv: myofibroblast integrins activate latent TGF-β1. Nat. Med. 19, 1567–1568 (2013).
Basta, J. et al. Pharmacologic inhibition of RGD-binding integrins ameliorates fibrosis and improves function following kidney injury. Physiol. Rep. 8, e14329 (2020).
Henderson, N. C. & Sheppard, D. Integrin-mediated regulation of TGFβ in fibrosis. Biochim. Biophys. Acta 1832, 891–896 (2013).
Kim, K. K., Sheppard, D. & Chapman, H. A. TGF-β1 signaling and tissue fibrosis. Cold Spring Harb. Perspect. Biol. 10, a022293 (2018).
Minagawa, S. et al. Selective targeting of TGF-β activation to treat fibroinflammatory airway disease. Sci. Transl. Med. 6, 241ra279 (2014).
Wang, J. et al. Atypical interactions of integrin αvβ8 with pro-TGF-β1. Proc. Natl Acad. Sci. USA 114, E4168–E4174 (2017).
Cormier, A. et al. Cryo-EM structure of the αvβ8 integrin reveals a mechanism for stabilizing integrin extension. Nat. Struct. Mol. Biol. 25, 698–704 (2018).
Asano, Y. et al. Increased expression of integrin αvβ5 contributes to the establishment of autocrine TGF-β signaling in scleroderma fibroblasts. J. Immunol. 175, 7708–7718 (2005).
Asano, Y. et al. Involvement of αvβ5 integrin-mediated activation of latent transforming growth factor β1 in autocrine transforming growth factor beta signaling in systemic sclerosis fibroblasts. Arthritis Rheum. 52, 2897–2905 (2005).
Tatler, A. L. et al. Integrin αvβ5-mediated TGF-β activation by airway smooth muscle cells in asthma. J. Immunol. 187, 6094–6107 (2011).
Scotton, C. J. et al. Increased local expression of coagulation factor X contributes to the fibrotic response in human and murine lung injury. J. Clin. Invest. 119, 2550–2563 (2009).
Zaveri, T. D., Lewis, J. S., Dolgova, N. V., Clare-Salzler, M. J. & Keselowsky, B. G. Integrin-directed modulation of macrophage responses to biomaterials. Biomaterials 35, 3504–3515 (2014).
Kang, H. et al. Immunoregulation of macrophages by dynamic ligand presentation via ligand–cation coordination. Nat. Commun. 10, 1696 (2019).
Jenney, C. R. & Anderson, J. M. Adsorbed serum proteins responsible for surface dependent human macrophage behavior. J. Biomed. Mater. Res. 49, 435–447 (2000).
Barr, S., Hill, E. W. & Bayat, A. Functional biocompatibility testing of silicone breast implants and a novel classification system based on surface roughness. J. Mech. Behav. Biomed. Mater. 75, 75–81 (2017).
Zollinger, A. J. & Smith, M. L. Fibronectin, the extracellular glue. Matrix Biol. 60–61, 27–37 (2017).
Ringer, P., Colo, G., Fassler, R. & Grashoff, C. Sensing the mechano-chemical properties of the extracellular matrix. Matrix Biol. 64, 6–16 (2017).
Kong, F., Garcia, A. J., Mould, A. P., Humphries, M. J. & Zhu, C. Demonstration of catch bonds between an integrin and its ligand. J. Cell Biol. 185, 1275–1284 (2009).
Friedland, J. C., Lee, M. H. & Boettiger, D. Mechanically activated integrin switch controls α5β1 function. Science 323, 642–644 (2009).
Van Putten, S. M. et al. Endotoxin contamination delays the foreign body reaction. J. Biomed. Mater. Res. A 98, 527–534 (2011).
Spiegel, A. J., Kania, K. & Hamilton, K. L. 2020 special issue: twenty years of breast reconstruction: past, present, and future. Breast J. 26, 39–41 (2020).
Yim, H. W., Nguyen, A. & Kim, Y. K. Facial contouring surgery with custom silicone implants based on a 3D prototype model and CT-Scan: a preliminary study. Aesthetic Plast. Surg. 39, 418–424 (2015).
Sakai, T. et al. Plasma fibronectin supports neuronal survival and reduces brain injury following transient focal cerebral ischemia but is not essential for skin-wound healing and hemostasis. Nat. Med. 7, 324–330 (2001).
Lodyga, M. et al. Cadherin-11-mediated adhesion of macrophages to myofibroblasts establishes a profibrotic niche of active TGF-β. Sci. Signal. 12, eaa03469 (2019).
Balestrini, J. L., Chaudhry, S., Sarrazy, V., Koehler, A. & Hinz, B. The mechanical memory of lung myofibroblasts. Integr. Biol. 4, 410–421 (2012).
Sawada, Y. & Sheetz, M. P. Force transduction by Triton cytoskeletons. J. Cell Biol. 156, 609–615 (2002).
Hinz, B., Dugina, V., Ballestrem, C., Wehrle-Haller, B. & Chaponnier, C. Alpha-smooth muscle actin Is crucial for focal adhesion maturation in myofibroblasts. Mol. Biol. Cell 14, 2508–2519 (2003).
O’Reilly, D. R., Miller, L. K. & Luckow, V. A. Baculovirus Expression Vectors—A Laboratory Manual (Oxford Univ. Press, 1992).
Acknowledgements
We are very grateful to A. Modarressi (Plastic, Reconstructive and Aesthetic Surgery Division, University Hospitals Geneva, Geneva, Switzerland) for providing expert advice on breast implant materials and medical complications. We thank G. Gabbiani (University of Geneva) for kindly providing the α-SMA antibody, H. Ni (St. Michael’s Hospital, Toronto) for the anti-fibrin antibodies, C.-H. Heldin (University of Uppsala, Sweden) for the LTBP-1 antibody and J. Murphy-Ullrich for providing the LAP expression construct. The FN−/− MEFs were a kind gift from M. Costell (Universitat de València, Spain) and R. Fässler (Max Planck Institute of Biochemistry, Munich, Germany). The col1a1 transgenic mice were provided by D. Brenner (University of California, San Diego). We also thank J. Firmino and D. Rajshankar at the Collaborative Advanced Microscopy Labs of Dentistry (CAMiLoD; Faculty of Dentistry, University of Toronto) and S. Plotnikov (Cell and Systems Biology, University of Toronto) for outstanding help with image acquisition and data analysis. We gratefully acknowledge F. Younesi (Hinz laboratory), F. Sarraf and N. Valiquette (Histology service, Faculty of Dentistry, University of Toronto) and the staff of the Centre for Phenogenomics (Mount Sinai Hospital, Toronto) for excellent technical histology support. The research of B.H. is supported by a foundation grant from the Canadian Institutes of Health Research (375597) and support from the John R. Evans Leaders Fund (grant numbers 36050, 38861 and 38430), as well as innovation funds (Fibrosis Network; grant number 36349) from the Canada Foundation for Innovation (CFI) and Ontario Research Fund (ORF). M.E. is supported by an Ontario Graduate Scholarship (OGS). R.S. is supported by a grant from the Mathematics of Information Technology and Complex Systems (MITACS; IT13623).
Author information
Authors and Affiliations
Contributions
N.N., S.v.P., A.K. and B.H. conceived of the study idea. N.N., R.S., S.v.P., M.E., A.K., S.B., N.M.C. and B.H. developed the methodology. N.N., R.S., S.v.P., M.E. and A.K. performed the formal analysis and data visualization. D.G. and P.R. provided resources. B.H. was responsible for project administration, supervision and funding acquisition. N.N. and S.v.P. prepared the original draft of the manuscript. N.N., R.S., S.v.P., S.B., N.M.C., D.G., P.R., C.A.M. and B.H. reviewed and edited the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Peer review information Nature Biomedical Engineering thanks David Lagares and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Figs. 1–9.
Rights and permissions
About this article
Cite this article
Noskovicova, N., Schuster, R., van Putten, S. et al. Suppression of the fibrotic encapsulation of silicone implants by inhibiting the mechanical activation of pro-fibrotic TGF-β. Nat Biomed Eng 5, 1437–1456 (2021). https://doi.org/10.1038/s41551-021-00722-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41551-021-00722-z
This article is cited by
-
Fibroblast and myofibroblast activation in normal tissue repair and fibrosis
Nature Reviews Molecular Cell Biology (2024)
-
Mechanical stiffness promotes skin fibrosis through Piezo1-mediated arginine and proline metabolism
Cell Death Discovery (2023)
-
Controlled swelling of biomaterial devices for improved antifouling polymer coatings
Scientific Reports (2023)
-
Cell–extracellular matrix mechanotransduction in 3D
Nature Reviews Molecular Cell Biology (2023)
-
Adhesive bioelectronics for sutureless epicardial interfacing
Nature Electronics (2023)