Abstract
Commercial pharmacogenetic testing panels capture a fraction of the genetic variation underlying medication metabolism and predisposition to adverse reactions. In this study we compared variation in six pharmacogenes detected by whole genome sequencing (WGS) to a targeted commercial panel in a cohort of 308 individuals with family history of pediatric heart disease. In 1% of the cohort, WGS identified rare variants that altered the interpretation of metabolizer status and would thus prevent potential errors in gene-based dosing.
Similar content being viewed by others
Pharmacogenetic (PGx) testing can be employed to optimize drug selection and dosing by factoring in genetic influences on drug metabolism and response, reducing side effects and enhancing therapeutic outcomes compared to a generic “one-size-fits-all” treatment approach1,2. Pharmacogenes, such as the family of cytochrome P450 (CYP) enzyme-encoding genes are highly polymorphic, with significant variation observed across various racial and ethnic groups3,4,5. Rare variants account for roughly 30–40% of functional PGx variation6. Ensuring that PGx testing captures these variations within the global population is essential for providing precise and reliable gene-drug-based dosing recommendations5,7.
Targeted genotyping and sequencing have catalyzed PGx testing due to the availability of low-cost commercial panels relative to whole genome sequencing (WGS)8,9. While uptake of commercial PGx panels has expanded access to testing, targeted genotyping assays in particular, capture just a fraction of the variation that influences response and adverse reaction to medications5,8. This pitfall is pronounced when targeted PGx genotyping panels are applied to individuals of non-European descent5. The disparity in representation can be attributed to factors such as the reference genome and historic disproportionality of European ancestry in genetic research3,10. Despite the widespread use of human reference genome GRCh38, ~70% of GRCh38.p13 is derived from a single individual, which results in an inadequate representation of genetic diversity10. Consequently, this limitation hinders a comprehensive understanding of population-specific variation and the accurate sequencing of polymorphic regions10,11. Another significant concern arises from the overrepresentation of European ancestry in PGx research, in contrast to the under-documentation of clinically actionable alleles that are relatively common in other genetic ancestral groups3. Nevertheless, functionally characterized, clinically actionable variants with low general population frequency are also often omitted from panels12. Collectively, the gap in representation reflected in commercial PGx panels may further exacerbate health disparities in non-European origin populations3,11. Bridging the diversity gap will improve pharmacotherapy guidance for all patients5,11.
Recent studies have demonstrated the benefit of a WGS-guided approach to capture clinically actionable PGx variants in diverse populations in addition to uncovering variants that warrant functional characterization12,13. To further explore the utility of WGS in pharmacogenetic applications, we evaluated the concordance of PGx diplotype calls between a commercial targeted genotyping panel and WGS in a cohort of individuals with cardiac disease (n = 308) from diverse racial and ethnic backgrounds.
Self-reported maternal and paternal ancestry data was available for 245 (80%) study participants (Table 1). Of these participants, 84% were classified as having a single ancestry, and 16% were classified as having multiple ancestries. Among participants with a single reported ancestry, European was most frequently reported (74%), followed by South Asian (12%).
Analysis of WGS data and targeted panel calls revealed discordant haplotype assignments in three unrelated participants (denoted A–C) of different self-reported ancestral backgrounds. These individuals exhibited variants in CYP2C9 and CYP2C19 that were captured by WGS, but not by the commercial panel. Identification of the rare alleles in these participants by WGS consequently altered the interpretation of metabolizer status. A deletion of ~70 kb, encompassing the first four exons of CYP2C19, was identified in participant A of North European and Jewish Ashkenazi ancestry (Table 2). The commercial panel is designed to detect single nucleotide variants and small insertions/deletions, which explains the inability to detect the deletion in this participant. Deletions involving CYP2C19, such as CYP2C19*37 (partial deletion) are rare, with an estimated heterozygote frequency of 0.046% in the general population14. In participant B of South Asian ancestry, WGS identified CYP2C9*14, a decreased function allele (Table 2). Notably, CYP2C9*14 while globally rare, is more common among South Asian populations in gnomAD (Table 3). The commercial panel does not interrogate this allele, explaining the incorrect assignment of *1. The CYP2C9*3 allele was detected by both technologies (Table 2). Furthermore, WGS captured rare variants defining CYP2C19*34 in participant B; an allele of uncertain function without actionable clinical recommendations (Tables 2 and 3). Uncertain function alleles are not interrogated by the commercial panel and were thus assigned *1. In participant C of Jamaican ancestry, WGS identified variants defining CYP2C19*22, a rare no-function allele not interrogated by the commercial panel (Tables 2 and 3).
One ongoing challenge in the interpretation of genomic data is the paucity of knowledge about variants in various ancestral populations3,11. Here we demonstrate that the identification of rare alleles by WGS prevents potential errors in gene-based dosing. For example, CYP2C19*37, CYP2C19*22, and CYP2C9*14 alleles reduce the activity of their respective enzymes, thereby leading to distinct medication metabolism patterns for participants A–C. Consequently, the alleles identified by WGS altered the determination of metabolizer statuses. Reduced CYP2C19 enzyme activity in participants A and C would warrant deviation from standard dosing, or avoidance of certain medications such as the antiplatelet medication, clopidogrel15. Significantly reduced CYP2C9 enzyme activity in participant B would also warrant deviation from standard dosing of certain medications or selection of alternative therapies. For example, this may influence medications such as non-steroidal anti-inflammatory drugs (NSAIDs) and HMG-CoA reductase inhibitors (statins) that are broken down by this enzyme pathway16,17. Although dosing guidance is not available for uncertain function alleles, this finding in participant B emphasizes the critical need to functionally characterize rare variants in various racial and ethnic groups3.
Our findings highlight how the absence of ancestrally specific variants from a commercial panel may lead to inaccurate information for medication guidance. The discordant haplotype assignments were attributed to variant omission in the panel design and may be a result of outdated evidence. The PGx Working Group of the Association for Molecular Pathology (AMP) Clinical Practice Committee recommends a set of variants that should serve as the basis for clinical PGx panels. As per the last review of CYP2C9 published in 2018, CYP2C9*14 was considered an allele of uncertain function18. A more recent review by the Clinical Pharmacogenetics Implementation Consortium (CPIC) in 2019 found moderate evidence for decreased enzyme activity associated with this allele, which is denoted by the Pharmacogene Variation Consortium (PharmVar) and the Pharmacogenomics Knowledgebase (PharmGKB). This warrants the inclusion of CYP2C9*14 in PGx panels, to expand coverage of clinically actionable PGx variants, particularly in individuals of South Asian ancestry who carry this variant more frequently. The CPIC annotated, non-functioning CYP2C19*22 allele, has been observed in individuals of African/African American ancestry in gnomAD, although it was not included in the most recent recommendations by AMP, likely attributable to low population frequency (Table 3). Deletions of CYP2C19 are also not included in the most recent recommendations by AMP19. This may be a result of the scarcity of literature detailing the functional consequence of CYP2C19 deletions. Despite this, partial and full CYP2C19 deletions have been annotated by CPIC as ‘no function’ alleles based on the presumption of a resulting non-functional protein. Pipelines for the detection of copy number variation in pharmacogenes like CYP2D6 have already been validated12. Copy number variation in CYP2C19 is not typically assayed by targeted PGx tests, although it may be advisable for commercial and clinical laboratories to consider this based on accumulating reports of this variation in the general population14. Next-generation sequencing, particularly WGS, can identify variation across diverse populations and offers the ability to re-interrogate data as additional functional variants are elucidated and as new gene-drug guidance becomes available3,12. Until WGS is adopted in routine practice, targeted panels need to be continuously updated to reflect the rapidly evolving literature and must extend coverage to variation that is representative of diverse and under-served populations.
The significance of representative genetic testing cannot be overemphasized. The development of a comprehensive human pangenome reference serves as a crucial stride towards promoting inclusivity in genetics10. Likewise, commercial genetic testing panels should prioritize the detection of clinically significant PGx variants across diverse racial and ethnic groups, specifically when this information is used for clinical care. To prevent further mis-assignments of metabolizer status as observed in the individuals reported herein, ongoing evaluation of ancestrally specific genetic variants should be foundational in designing and updating genetic testing panels.
Methods
Families with pediatric heart disease were recruited through the Ted Rogers Cardiac Genome Clinic (CGC) at a single site, The Hospital for Sick Children, Division of Cardiology. The study was conducted in collaboration with the Division of Clinical Pharmacology and Toxicology at The Hospital for Sick Children. This study was conducted in accordance with all relevant ethical regulations including the Declaration of Helsinki. The study was approved by the research ethics board of The Hospital for Sick Children (REB #1000053844 and #1000053445) and the University Health Network (REB#: 16-6282). Written informed consent was obtained on behalf of all participants. Details of the CGC cohort and ongoing PGx pilot study have been previously described20,21. Self-reported maternal and paternal ancestry was captured during the initial genetics assessment and pedigree analysis. Maternal and paternal ancestries were transformed into ancestral categories by investigators. Since the last publication in 202121, an additional 308 participants have been enrolled as of June 2023. The results reported herein are from newly enrolled participants.
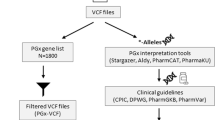
Banked DNA from whole blood was used for genetic analyses. PGx data was evaluated by WGS via the HiSeq X system (Illumina, Inc., San Diego, CA, USA) and by orthogonal targeted genotyping via the VeriDose® Core MassARRAY panel (Agena Bioscience, San Diego, CA, USA). Variants from six pharmacogenes (CYP2D6, CYP2C9, CYP2C19, CYP3A5, SLCO1B1, VKORC1) were analyzed. Evaluation of the six pharmacogenes was restricted to variation that has been annotated by PharmVar (https://www.pharmvar.org/) and PharmGKB (https://www.pharmgkb.org/). PGx haplotypes for the CYP genes are designated using the star (*) allele nomenclature system. In accordance with standard practice, a default assignment of ∗1 wild-type allele, or *3 for CYP3A5, was made if none of the tested variants were detected by the commercial panel or in the absence of WGS-identified PGx variants with known functional status18,22. Impact on metabolism, or metabolizer status, for each participant, was determined using established genotype-to-phenotype translation tables from CPIC. PGx haplotypes and inferred metabolizer statuses derived from WGS data were compared to those generated by the MassARRAY Typer Analyzer (version 5.0.2) and iPLEX ADME PGx Pro (version 3.99.105) software to assess concordance between the two technologies.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
Additional de-identified data may be shared upon reasonable request and with fulfilled legal requirements (approval from all ethics committees and data transfer agreements).
References
Duarte, J. D. & Cavallari, L. H. Pharmacogenetics to guide cardiovascular drug therapy. Nat. Rev. Cardiol. 18, 649–665 (2021).
Klein, M. E., Parvez, M. M. & Shin, J.-G. Clinical implementation of pharmacogenomics for personalized precision medicine: barriers and solutions. J. Pharm. Sci. 106, 2368–2379 (2017).
McInnes, G. et al. Pharmacogenetics at scale: an analysis of the UK Biobank. Clin. Pharmacol. Ther. 109, 1528–1537 (2021).
Zhou, Y. & Lauschke, V. M. The genetic landscape of major drug metabolizing cytochrome P450 genes—an updated analysis of population-scale sequencing data. Pharmacogenom. J. 22, 284–293 (2022).
Luo, S. et al. Comprehensive allele genotyping in critical pharmacogenes reduces residual clinical risk in diverse populations. Clin. Pharmacol. Ther. 110, 759–767 (2021).
Kozyra, M., Ingelman-Sundberg, M. & Lauschke, V. M. Rare genetic variants in cellular transporters, metabolic enzymes, and nuclear receptors can be important determinants of interindividual differences in drug response. Genet. Med. 19, 20–29 (2017).
Hoshitsuki, K. et al. Challenges in clinical implementation of CYP2D6 genotyping: choice of variants to test affects phenotype determination. Genet. Med. 22, 232–233 (2020).
Tilleman, L., Weymaere, J., Heindryckx, B., Deforce, D. & Nieuwerburgh, F. V. Contemporary pharmacogenetic assays in view of the PharmGKB database. Pharmacogenomics 20, 261–272 (2019).
van der Lee, M., Kriek, M., Guchelaar, H.-J. & Swen, J. J. Technologies for pharmacogenomics: a review. Genes (Basel). 11, 1456 (2020).
Wang, T. et al. The Human Pangenome Project: a global resource to map genomic diversity. Nature 604, 437–446 (2022).
Luczak, T., Stenehjem, D. & Brown, J. Applying an equity lens to pharmacogenetic research and translation to under-represented populations. Clin. Transl. Sci. 14, 2117–2123 (2021).
Lopes, J. L. et al. Targeted genotyping in clinical pharmacogenomics: what is missing.J. Mol. Diagn. 24, 253–261 (2022).
Cohn, I. et al. Genome sequencing as a platform for pharmacogenetic genotyping: a pediatric cohort study. npj. Genom. Med. 2, 19 (2017).
Botton, M. R. et al. Structural variation at the CYP2C locus: characterization of deletion and duplication alleles. Hum. Mutat. 40, e37–e51 (2019).
Lee, C. R. et al. Clinical pharmacogenetics implementation consortium guideline for CYP2C19 genotype and clopidogrel therapy: 2022 update. Clin. Pharmacol. Ther. 112, 959–967 (2022).
Theken, K. N. et al. Clinical Pharmacogenetics Implementation Consortium Guideline (CPIC) for CYP2C9 and Nonsteroidal Anti-Inflammatory Drugs. Clin Pharmacol Ther. 108, 191–200 (2020).
Cooper-DeHoff, R. M. et al. The clinical pharmacogenetics implementation consortium guideline for SLCO1B1, ABCG2, and CYP2C9 genotypes and statin-associated musculoskeletal symptoms. Clin. Pharmacol. Ther. 111, 1007–1021 (2022).
Pratt, V. M. et al. Recommendations for clinical CYP2C9 genotyping allele selection: a joint recommendation of the association for molecular pathology and College of American Pathologists. J. Mol. Diagn. 21, 746–755 (2019).
Pratt, V. M. et al. Recommendations for clinical CYP2C19 genotyping allele selection: a report of the association for molecular pathology. J. Mol. Diagn. 20, 269–276 (2018).
Reuter, M. S. et al. The Cardiac Genome Clinic: implementing genome sequencing in pediatric heart disease. Genet. Med. J. Am. Coll. Med. Genet. 22, 1015–1024 (2020).
Cohn, I. et al. Assessment of the implementation of pharmacogenomic testing in a pediatric tertiary care setting. JAMA Netw. Open 4, e2110446–e2110446 (2021).
Gaedigk, A., Casey, S. T., Whirl-Carrillo, M., Miller, N. A. & Klein, T. E. Pharmacogene variation consortium: a global resource and repository for pharmacogene variation. Clin. Pharmacol. Ther. 110, 542–545 (2021).
Acknowledgements
We thank the families for their participation and the many healthcare professionals involved in their care. We would also like to thank Sierra Scodellaro, Marci Schwartz, Olivia Moran, and Kaitlin Stanley for their ongoing contributions to this study. This study was supported by the SickKids Foundation. The funder played no role in study design, data collection, analysis and interpretation of the data, or the writing of this manuscript.
Author information
Authors and Affiliations
Contributions
I.C., R.K.J., and R.H.K. conceptualized and administered the study. I.C. acquired funding and supervised the study. R.M. performed genetic analyses and variant extraction. R.M. and I.C. performed data curation. I.C., A.K., and G.M. interpreted data. A.K. and G.M. drafted the manuscript. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kennedy, A., Ma, G., Manshaei, R. et al. A call for increased inclusivity and global representation in pharmacogenetic testing. npj Genom. Med. 9, 13 (2024). https://doi.org/10.1038/s41525-024-00403-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41525-024-00403-1