Abstract
Risk-reducing endocrine therapy use, though the benefit is validated, is extremely low. The FDA has approved tamoxifen and raloxifene for a 5-year Breast Cancer Risk Assessment Tool (BCRAT) risk ≥ 1.67%. We examined the threshold at which high-risk women are likely to be using endocrine risk-reducing therapies among Athena Breast Health Network participants from 2011–2018. We identified high-risk women by a 5-year BCRAT risk ≥ 1.67% and those in the top 10% and 2.5% risk thresholds by age. We estimated the odds ratio (OR) of current medication use based on these thresholds using logistic regression. One thousand two hundred and one (1.2%) of 104,223 total participants used medication. Of the 33,082 participants with 5-year BCRAT risk ≥ 1.67%, 772 (2.3%) used medication. Of 2445 in the top 2.5% threshold, 209 (8.6%) used medication. Participants whose 5-year risk exceeded 1.67% were more likely to use medication than those whose risk was below this threshold, OR 3.94 (95% CI = 3.50–4.43). The top 2.5% was most strongly associated with medication usage, OR 9.50 (8.13–11.09) compared to the bottom 97.5%. Women exceeding a 5-year BCRAT ≥ 1.67% had modest medication use. We demonstrate that women in the top 2.5% have higher odds of medication use than those in the bottom 97.5% and compared to a risk of 1.67%. The top 2.5% threshold would more effectively target medication use and is being tested prospectively in a randomized control clinical trial.
Similar content being viewed by others
Introduction
Prevention trials have shown unequivocally that endocrine risk-reducing medications (such as selective estrogen receptor modulators and aromatase inhibitors) lower breast cancer risk1,2,3,4,5,6,7,8. According to the US Preventative Services Task Force (USPSTF), preventive therapy is recommended for high-risk women, and even younger women9,10,11,12. However, uptake remains low, for numerous reasons. These reasons include the fear of side effects, resistance to taking a medicine that is used for cancer treatment, objection to taking a medicine at all, the consistent reminder that they are high risk, and failure to appreciate the benefit that they would receive (by both primary care physicians and the woman at risk)13,14,15. Studies have also suggested that patient adherence and use of prevention therapy is correlated to the absolute risk and targeting high-risk groups who would be amenable to risk-reducing therapy13,16,17.
A primary care physician’s recommendation often plays a significant role in a patient’s decision-making; risk models were developed to determine risk level and who should consider risk-reducing therapy18. The Breast Cancer Risk Assessment Tool (BCRAT) risk model was developed by the National Cancer Institute for use in the National Surgical Adjuvant Breast and Bowel Project (NSABP) P-01 breast cancer prevention trial. As a result, the Food and Drug Administration (FDA) approved the use of selective estrogen receptor modulators (SERMs) tamoxifen and raloxifene in women with a 5-year BCRAT risk of 1.67% or greater, based on the average 5-year breast cancer risk for a 50-year-old white female7,19,20. FDA approval of tamoxifen and raloxifene in women with a 5-year BCRAT risk of 1.67% or greater has not led to widespread prescription and uptake of risk-reducing therapy13,21.
In the ensuing years, many newer risk models have been developed to identify risk for breast cancer, include BOADICEA, Tyrer-Cuzick, and Breast Cancer Surveillance Consortium (BCSC)22,23,24. The aforementioned models can be modified by genetic, genomic, or polygenic risk, but research findings are still undergoing validation. For example, a number of high and intermediate penetrance susceptibility genes (e.g., ATM, CHEK2, and PALB2) have been found to be associated with breast cancer. The science of single-nucleotide polymorphisms (SNPs) in stratifications of risk are also modifying models that could impact screening and risk assessment25,26,27. To date, some studies have demonstrated that SNPs can improve BCRAT, Tyrer-Cuzick, and BCSC risk models26,28,29,30,31,32,33.
Most risk models are not necessarily calibrated at specific risk thresholds. We identified that the highest risk group—e.g., top 10% risk by age—identifies a group at much higher risk for breast cancer, where women might be motivated to take endocrine risk reduction34. Though risk models have improved, it is still not well studied how best to target prevention medications effectively at those who are likely to take them. There is a lack of agreement in published studies on whether risk-reducing therapy use increases when women are at high risk13. Since absolute thresholds (such as the FDA approval for tamoxifen and raloxifene) are more likely to overrepresent older women, we hypothesize that age-based thresholds may also include younger women who would benefit from risk-reducing therapy.
The Athena Breast Health Network retrospectively assessed the usage of endocrine risk-reduction therapy by the threshold of risk by age. This program started in 2010, and thus the BCRAT risk model was standard at that time. We sought to determine at what risk threshold therapy is already used by women before standardized active outreach/high-risk counseling, as this may suggest the threshold that primary care providers prescribe, and women use, these therapies. We use a screening registry cohort to compare risk-reducing therapy usage at their time of enrollment in the cohort across three risk thresholds: (1) absolute 5-year BCRAT risk of over 1.67%, (2) top 10% risk by age, and (3) top 2.5% risk by age.
Results
Descriptive statistics
Table 1 shows the demographic characteristics of the Athena sample. Of the 104,223 participants, 1210 (1.2%) indicated endocrine risk-reduction use. The highest risk-reducing therapy usage was in risk threshold 3 (top 2.5% risk by age), where 209 of 2445 women (8.6%) used risk-reducing therapy. The lowest risk-reducing therapy usage was in risk threshold 1 (5-year BCRAT risk ≥ 1.67%), where 772 of 33,082 women (2.3%) reported medication use. The average risk was higher in the age-based threshold groups (thresholds 2 and 3). Mean age was slightly older in threshold 1 (61, SD = 7.6), while the age-based thresholds were consistent with the overall sample. The sample was mostly white and non-Hispanic.
Table 2 describes the distribution of women in various risk strata and their use of risk-reducing medication. The percentage of chemoprevention users in each nonoverlapping risk strata increases from 0.6% among those not meeting the 5-year BCRAT risk to 8.6% among those in the top 2.5% of risk by age. Still, the proportion of no endocrine risk reduction used remained consistent across the strata, with over 90% of women in each nonoverlapping threshold not currently using risk reduction.
The mean risks of each risk threshold stratified by risk-reducing therapy use are provided in Table 3. Notably, among participants indicating risk-reducing therapy use, lifetime score in risk threshold 3 (mean lifetime BCRAT risk = 27.73% or 5-year BCRAT risk = 5.68%) was nearly 1.7 times that of risk threshold 1 (mean lifetime BCRAT risk = 15.90% or 5-year BCRAT risk = 3.52%).
In addition, as described in Supplementary Table 1 and Supplementary Fig. 1, the mean 5-year BCRAT risk varied with each of the different age categories for a given risk by age.
Regression analysis
The results from three bivariate logistic regression models for risk-reducing therapy adoption and predicted probabilities from marginal effects are presented in Table 4. The models were all significant using the likelihood-ratio chi-squared test to P-value < 0.01. Additional regression models, including adjustments by age and continuous 5-year risk, are included in Supplementary Table 2.
Meeting threshold 1 was associated with nearly 4 times higher odds of adopting medication than if a participant did not meet threshold 1 (Odds ratio [OR] = 3.90; 95% confidence interval [95% CI]: 3.50–4.43). The predicted probability of a woman meeting risk threshold 1 reporting medication use was 2.33% (95% CI: 2.17–2.50; actual use in the dataset: 2.38%).
Satisfying threshold 2 was associated with over five times higher odds of reporting medication use than if a participant did not meet threshold 2 (OR = 5.20; 95% CI: 4.61–5.87). The predicted probability of a woman meeting risk threshold 2 reporting risk-reducing therapy was higher, at 4.21% (95% CI: 3.81–4.61; actual use in the dataset: 4.20%).
Satisfying threshold 3 was associated with 9.5 times higher odds of adopting medication than if a participant were not in threshold 3 (OR = 9.50; 95% CI: 8.13–11.09). The predicted probability of an average woman in threshold 3 using risk- reducing therapy was 8.55% (95% CI: 7.44–9.66; actual use in the dataset: 9.34%).
Discussion
This paper suggests that stratifying risk by age categories was associated with a higher medication use compared with the absolute risk threshold of a 5-year risk ≥ 1.67%. Participants within the top 2.5% of risk by their age (risk threshold 3) had higher odds of risk-reducing therapy use than those below this threshold. Notably, among participants indicating medication use, the lifetime score in risk threshold 3 (mean lifetime score = 27.7%) was 1.7 times that of risk threshold 1 (mean lifetime score = 15.9%).
Our age-based, elevated risk thresholds set for the top 2.5% were generally consistent with the USPSTF recommendation that the benefit of risk-reducing therapy outweighs the risk for women with an absolute 3% 5-year breast cancer risk12. However, our top 2.5% by age threshold also captured women ages 35–44 who fell below this USPSTF threshold. Using the absolute USPSTF threshold would have decreased the percentage of women from this younger age category who should be targeted for medication, per our findings. Therefore, age-based risk thresholds may better target prevention among younger women, whose risks may be high for their age categories, but not enough to meet the absolute risk cut-off. These younger women identified through the risk thresholds method are likely to benefit for a longer time course as well, as the pharmacologic benefit of endocrine risk reduction would last beyond the 5 years of active therapy11. This risk assessment approach parallels a strategy proposed for cardiovascular disease prevention to move beyond treatment solely on risk models, where risk increases with age35.
Our study confirms a strategy to identify those high-risk women who are inclined to use risk-reducing therapy for population health21. Prior studies have mainly focused on assessing which components of risk scores are associated with higher risk-reducing therapy use14. The risk thresholds approach could be especially helpful to primary care physicians. First, it provides these care providers with a more efficient method of identifying individuals who are most likely to benefit from prevention. Second, previous literature suggests that sharing how a woman’s risk compares to others their own age could improve their understanding of risk34. This may help to ameliorate concerns highlighted in studies that have shown that risk assessment could be better communicated to women to increase uptake, with improved cultural humility or low literacy friendly language15,36,37.
This study’s findings are also neither specific to the risk model we used nor does it suggest a comparison between modern risk models. Instead, it proposes a method for identifying, targeting, and messaging endocrine risk-reducing therapy toward women identified as part of higher risk by age thresholds. These women are already more likely to take endocrine risk-reducing medication. Our results about identifying elevated risk thresholds by age should be replicable using other modern and current risk models, such as Tyrer-Cuzick, BOADICEA, and Breast Cancer Surveillance Consortium (BCSC)22,23,24.
There remain limitations with our study. It is generally difficult to capture all aspects that influence a person’s decision to adopt or adhere to endocrine risk-reducing therapy, which also involves understanding the risk of known side effects. Athena screening registry data were cross-sectional, prior any Athena high-risk consultations. Therefore, it is impossible to ascertain how much information women received about their risk at a different primary care provider or screening clinic. The calculated risk score for each woman is not necessarily the woman’s risk when she started on endocrine risk-reducing medication, so this may have informed a woman’s decision to take endocrine risk-reducing medication previously. Due to the cross-sectional design, this study also does not assess drug uptake or compliance. Further research needs to be done to assess the efficacy of standardized breast health specialist consultations and to better understand the factors impacting decision-making. A study design with prospective follow-up on the use of endocrine risk-reducing medication among healthy women is needed to confirm our conclusions.
Our analysis is also limited to logistic regression-based solely on risk threshold, which was calculated based on distributions within the Athena screening registry sample. The present sample is limited in its racial diversity (largely white and non-Hispanic), and its geography (participants based in the west and midwestern United States). This study also could be strengthened by predictions with more comprehensive risk factors and the use of a validated large-sample longitudinal, prospective studies, such as those included in the Nurses’ Health Study34. Additionally, our retrospective analysis was conducted using 5-year BCRAT risk estimates, because it was standard during the early years of data collection. There also are issues with the BCRAT risk model, highlighted previously, which could be improved upon by more modern risk models and the inclusion of other breast density, genomic, genetic, and polygenic risk factors.
Our study suggests that women in the top 2.5% of risk by age (mean 5-year BCRAT risk of 5.68% or mean lifetime BCRAT risk of 27.73%) are using endocrine risk-reducing medication. The use (8.2%) in this subset, while higher than the national average, is still low. Using age-stratified, percentile-based risk thresholds may be helpful to target endocrine risk-reducing medication and risk-reducing strategies.
To test this finding prospectively and address the limitations of this retrospective analysis, Athena investigators developed the Women Informed to Screen Depending On Measures of risk (WISDOM) Study. The WISDOM Study is a pragmatic, randomized control trial (NCT02620852), recruiting a diversity of participants across the United States representative of the national population. The third principal aim of the study tests if identifying and providing an enriched approach—with direct educational outreach to women in the narrowly defined the top 2.5% of risk by age—increases endocrine risk-reducing medication uptake and acceptability among high-risk women compared to standard risk assessment38. The risk thresholds by age will be calculated using the BCSC risk model combined with a polygenic risk score (PRS). To support this aim, a risk-based prevention framework was created. The women in the top 2.5% of risk by age will have direct outreach by a Breast Health Specialist. Investigators developing a standardized presentation of risk and delivering educational materials about risk-reducing strategies through an online risk assessment tool, which will be publicly available once validated39. Additionally, risk-reducing lifestyle interventions may be appropriate for an expanded risk group informed by the WISDOM Study. These efforts will hopefully lead to greater use of risk reduction options among populations who would benefit the most.
This and subsequent studies will enable more comprehensive follow-up of women who develop breast cancer who are both above and below these risk thresholds. More women in absolute numbers who develop breast cancer may be below the top 2.5% risk threshold and may be less likely to take up endocrine risk-reducing medication. However, understanding these nuances will ultimately improve our ability to stratify and communicate breast cancer risk, and target risk-reducing options to appropriate high-risk individuals.
Methods
Clinical procedures and measurements
The Athena Breast Health Network (Athena) was established in 2009 across the University of California (UC) medical centers (Davis, Irvine, Los Angeles, San Diego, San Francisco), and later added the Sanford Health system in the midwestern United States to recruit a national cohort of women screened with mammography or other technologies40. One of Athena’s principal strategic aims is to integrate risk assessment into the breast cancer screening process and identify those at high risk to offer preventive options25.
Every woman screened for breast cancer at a participating Athena clinic is required to complete an online intake survey prior to each mammography screening appointment. The survey includes questions regarding a woman’s age, demographic information, family cancer history, and other breast cancer risk factors. In addition, the survey contained a question about the use of risk-reducing medication use, such as SERMs (tamoxifen, raloxifene) and AIs (anastrozole, exemestane, letrozole). Self-reported survey data were taken from each survey and imported into a data warehouse, run by the Salesforce Cloud. The inputs were automatically calculated and stored as 5-year, 10-year, and lifetime BCRAT risk, which was considered standard at the start of the Network.
Once the intake survey was completed, Athena participants received active outreach via telephone if their 5-year BCRAT risk was in the top 10% by age. Breast health specialists (genetic counselors and preventive medicine specialists with expertise in breast cancer risk assessment) provided education on breast cancer risk using a personalized risk assessment framework34. The content of the telephone call included a review of the participant’s individual risk and protective factors, clarification of their entered data, and discussion of recommendations for breast cancer prevention and early detection. Breast health specialists explained how the risk model and/or family history criteria were applied to participants; and, engaged in a personalized discussion of early detection and risk reduction options.
The Athena Salesforce platform includes a module for the breast health specialists to document which risk-specific elements were discussed during the phone call, and which (if any) referrals were recommended during the call. Genetic testing was recommended when appropriate based on National Comprehensive Cancer Network (NCCN) National Clinical Practice Guidelines in Oncology41,42. The module generated a consult note that was then uploaded to the participant’s electronic medical record. The cost of the BHS consultation was covered by some payers; when insurance did not cover the consultation, the cost was covered by the Athena program.
Study population
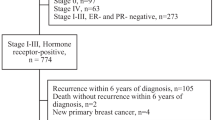
The Athena screening registry was conducted in accordance with protocols approved by the Institutional Review Board (IRB) of the University of California, San Francisco (11–06402). Informed consent was waived by the IRB, given there was no more than minimal risk to human subjects, and involves no procedures for which written consent is normally required outside of the research context. Participants were screened at UC Irvine, UC Los Angeles, UC San Francisco, UC San Diego, and Sanford Health between January 2011 and October 2018. Preliminary data collection was conducted in 2019. A maximum analytic sample of 104,223 women aged 35–74 was retained (Fig. 1) after excluding women with history of ductal carcinoma in situ (DCIS) or invasive breast cancer, for whom no risk was calculated, for those who did not meet age criteria. If a woman completed multiple surveys (e.g., if they had another mammogram in a subsequent year), we only considered the earliest entry.
The inclusion and exclusion criteria for the analytic sample in Athena Network registry. (1) refers to threshold 1: FDA approval for tamoxifen and raloxifene is 5-year risk score > 1.67; (2) refers to threshold 2: Use of Top 10% of Risk by Age; (3) refers to threshold 3: Use of Top 2.5% of Risk by Age.
Dependent variable
The dependent variable of interest, present medication use, refers to the self-reported use of risk-reducing therapy before screening at an Athena site and Athena high-risk counseling. The therapies included in this category are SERMs (tamoxifen and raloxifene) and aromatase inhibitors (exemestane, letrozole, and anastrozole). This information was self-reported on the Athena intake survey. The use of risk-reducing therapy was cataloged as a binary variable (i.e., “currently using risk-reducing medications” or “not currently using risk-reducing medications”).
Independent variables
Three risk thresholds were of interest: 5-year BCRAT score ≥ 1.67% (risk threshold 1), top 10% risk by age (risk threshold 2), and top 2.5% risk by age (risk threshold 3).
To calculate whether a particular sample met a particular risk threshold, we used the calculated 5-year risks and lifetime risks (estimated to age 90) for each participant using the BCRAT risk model. Inputs used in the BCRAT model to calculate risk scores are age, race/ethnicity, age of first menstrual period, first live birth, first-degree relatives with breast cancer, and previous breast biopsy19,43,44. Both 5-year and lifetime BCRAT risk estimates were provided because different expressions of risk may be salient to patients or their doctors, as documented in the literature34,45,46,47,48,49,50.
For risk threshold 1, we considered if women met the 5-year BCRAT risk score ≥ 1.67%. For risk thresholds 2 and 3, samples were grouped by age at survey completion (categories are ages 35–44, 45–54, 55–64, and 65–74). The risk threshold was calculated by mapping the distribution of risk by age category within the Athena cohort, and determining the top 10% and 2.5% (risk thresholds 2 and 3, respectively) of risk cut-offs by age grouping (see Supplementary Table 1 and Supplementary Fig. 1 for further details).
Statistical analysis
All statistical analyses were performed using Stata version 16.151. We used each of the three risk thresholds to predict self-reported current risk-reducing therapy use. The unit of analysis is an individual participant. A logistic regression model estimated risk-reducing therapy use based on each of the risk thresholds. Odds ratios (ORs) for all regression coefficient estimates were calculated. In addition to odds ratios, predicted probabilities were also calculated to assess the logistic regression model and provide an estimated probability of risk-reducing therapy use based on the average individual in each risk threshold. Predicted probabilities can be used for diagnostics and validation of the logistic regression model52. To control for Type I error, we set our significance level at p value < 0.05, with 95% confidence intervals.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
The data generated and analysed during this study are described in the following data record: https://doi.org/10.6084/m9.figshare.1477867553. Relevant data code that support the analysis of data for the study are available in the figshare repository at https://doi.org/10.6084/m9.figshare.14444546.54,55 Data analysis was conducted with Stata 16.1.
Code availability
Code that supports the analysis of data are available from the corresponding author upon reasonable request.
References
Cuzick, J. et al. Use of anastrozole for breast cancer prevention (IBIS-II): long-term results of a randomised controlled trial. The Lancet 395, 117–122 (2020).
Land, S. R. et al. Patient-reported symptoms and quality of life during treatment with tamoxifen or raloxifene for breast cancer prevention: the NSABP Study of Tamoxifen and Raloxifene (STAR) P-2 trial. JAMA 295, 2742–2751 (2006).
Cuzick, J. et al. Tamoxifen for prevention of breast cancer: extended long-term follow-up of the IBIS-I breast cancer prevention trial. Lancet Oncol. 16, 67–75 (2015).
Goss, P. E. et al. Exemestane for breast-cancer prevention in postmenopausal women. N. Engl. J. Med. 364, 2381–2391 (2011).
Fisher, B. et al. Tamoxifen for the prevention of breast cancer: current status of the National Surgical Adjuvant Breast and Bowel Project P-1 study. J. Natl. Cancer Inst. 97, 1652–1662 (2005).
Powles, T. J., Ashley, S., Tidy, A., Smith, I. E. & Dowsett, M. Twenty-year follow-up of the Royal Marsden randomized, double-blinded tamoxifen breast cancer prevention trial. J. Natl. Cancer Inst. 99, 283–290 (2007).
Waters, E. A., McNeel, T. S., McCaskill Stevens, W. & Freedman, A. N. Use of tamoxifen and raloxifene for breast cancer chemoprevention in 2010. Breast Cancer Res. Treat. 134, 875–880 (2012).
Visvanathan, K. et al. Use of pharmacologic interventions for breast cancer risk reduction: American Society of Clinical Oncology clinical practice guideline. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 31, 2942–2962 (2013).
Gail, M. H. et al. Weighing the risks and benefits of tamoxifen treatment for preventing breast cancer. J. Natl. Cancer Inst. 91, 1829–1846 (1999).
Freedman, A. N. et al. Benefit/risk assessment for breast cancer chemoprevention with raloxifene or tamoxifen for women age 50 years or older. J. Clin. Oncol. 29, 2327–2333 (2011).
Crew, K. D., Albain, K. S., Hershman, D. L., Unger, J. M. & Lo, S. S. How do we increase uptake of tamoxifen and other anti-estrogens for breast cancer prevention? NPJ Breast Cancer 3, 1–7 (2017).
Owens, D. K. et al. Medication use to reduce risk of breast cancer: US preventive services task force recommendation statement. JAMA 322, 857–867 (2019).
Smith, S. G. et al. Factors affecting uptake and adherence to breast cancer chemoprevention: a systematic review and meta-analysis. Ann. Oncol. 27, 575–590 (2016).
Flanagan, M. R. et al. Chemoprevention uptake for breast cancer risk reduction varies by risk factor. Ann. Surg. Oncol. 26, 2127–2135 (2019).
Donnelly, L. S. et al. Uptake of tamoxifen in consecutive premenopausal women under surveillance in a high-risk breast cancer clinic. Br. J. Cancer 110, 1681–1687 (2014).
Serrano, D., Bonanni, B. & Brown, K. Therapeutic cancer prevention: achievements and ongoing challenges - a focus on breast and colorectal cancer. Mol. Oncol. 13, 579–590 (2019).
Hum, S., Wu, M., Pruthi, S. & Heisey, R. Physician and patient barriers to breast cancer preventive therapy. Curr. Breast Cancer Rep. 8, 158–164 (2016).
Holmberg, C. et al. NRG oncology/national surgical adjuvant breast and bowel project decision-making project-1 results: decision making in breast cancer risk reduction. Cancer Prev. Res. (Phila. Pa.) 10, 625–634 (2017).
Rockhill, B., Spiegelman, D., Byrne, C., Hunter, D. J. & Colditz, G. A. Validation of the Gail et al. model of breast cancer risk prediction and implications for chemoprevention. J. Natl. Cancer Inst. 93, 358–366 (2001).
Estimating Breast Cancer Risk | Susan G. Komen® (2021). https://ww5.komen.org/BreastCancer/GailAssessmentModel.html.
Narod, S. A. Personalised medicine and population health: breast and ovarian cancer. Hum. Genet. 137, 769–778 (2018).
Lee, A. et al. BOADICEA: a comprehensive breast cancer risk prediction model incorporating genetic and nongenetic risk factors. Genet. Med. 21, 1708–1718 (2019).
Brentnall, A. R., Cuzick, J., Buist, D. S. M. & Bowles, E. J. A. Long-term Accuracy of Breast Cancer Risk Assessment Combining Classic Risk Factors and Breast Density. JAMA Oncol. 4, e180174 (2018).
Tice, J. A. et al. Validation of the breast cancer surveillance consortium model of breast cancer risk. Breast Cancer Res. Treat. 175, 519–523 (2019).
Shieh, Y. et al. Breast cancer screening in the precision medicine era: risk-based screening in a population-based trial. J. Natl Cancer Inst. 109, 1–8, https://doi.org/10.1093/jnci/djw290 (2017).
Mavaddat, N. et al. Prediction of breast cancer risk based on profiling with common genetic variants. J. Natl. Cancer Inst. 107, 1–15 (2015).
Brentnall, A. R. et al. A case-control evaluation of 143 single nucleotide polymorphisms for breast cancer risk stratification with classical factors and mammographic density. Int. J. Cancer 146, 2122–2129 (2020).
Michailidou, K. et al. Genome-wide association analysis of more than 120,000 individuals identifies 15 new susceptibility loci for breast cancer. Nat. Genet. 47, 373–380 (2015).
Michailidou, K. et al. Large-scale genotyping identifies 41 new loci associated with breast cancer risk. Nat. Genet. 45, 353–361 (2013). 361e1-362e1.
Zhang, X. et al. Addition of a polygenic risk score, mammographic density, and endogenous hormones to existing breast cancer risk prediction models: a nested case–control study. PLOS Med. 15, e1002644 (2018).
Shieh, Y. et al. Breast cancer risk prediction using a clinical risk model and polygenic risk score. Breast Cancer Res. Treat. 159, 513–525 (2016).
Cuzick, J. et al. Impact of a panel of 88 single nucleotide polymorphisms on the risk of breast cancer in high-risk women: results from two randomized tamoxifen prevention trials. J. Clin. Oncol. 35, 743–750 (2016).
Jantzen, R. et al. Validation of breast cancer risk assessment tools on a French-Canadian population-based cohort. BMJ Open 11, e045078 (2021).
Ozanne, E. M., Klemp, J. R. & Esserman, L. J. Breast cancer risk assessment and prevention: a framework for shared decision-making consultations. Breast J. 12, 103–113 (2006).
Lagerweij, G. R. et al. A new selection method to increase the health benefits of CVD prevention strategies. Eur. J. Prev. Cardiol. 25, 642–650 (2018).
Evans, D. G., Harvie, M., Bundred, N. & Howell, A. Uptake of breast cancer prevention and screening trials. J. Med. Genet. 47, 853–855 (2010).
Kaplan, C. P. et al. Breast cancer risk reduction options: awareness, discussion, and use among women from four ethnic groups. Cancer Epidemiol. Biomark. Prev. 15, 162–166 (2006).
Esserman, L. J., WISDOM Study and Athena Investigators. The WISDOM Study: breaking the deadlock in the breast cancer screening debate. NPJ Breast Cancer 3, 34 (2017).
Keane, H. et al. Development and pilot of an online, personalized risk assessment tool for a breast cancer precision medicine trial. npj Breast Cancer 7, 1–9, https://doi.org/10.1038/sr1523-021-00288-8 (2021).
Elson, S. L. et al. The Athena Breast Health Network: developing a rapid learning system in breast cancer prevention, screening, treatment, and care. Breast Cancer Res. Treat. 140, 417–425 (2013).
Daly, M. B. et al. NCCN Guidelines Insights: Genetic/Familial High-Risk Assessment: Breast and Ovarian, Version 2.2017. J. Natl. Compr. Cancer Netw. JNCCN 15, 9–20 (2017).
NCCN Framework for Resource Stratification of NCCN Guidelines (2021). https://www.nccn.org/framework/.
Costantino, J. P. et al. Validation studies for models projecting the risk of invasive and total breast cancer incidence. J. Natl. Cancer Inst. 91, 1541–1548 (1999).
Breast Cancer Risk Assessment Tool. Breast Cancer Risk Assessment Tool (2017). https://www.cancer.gov/bcrisktool.
Haas, J. S. et al. Perceived risk of breast cancer among women at average and increased risk. J. Womens Health 14, 845–851 (2005).
Fagerlin, A., Zikmund-Fisher, B. J. & Ubel, P. A. How making a risk estimate can change the feel of that risk: shifting attitudes toward breast cancer risk in a general public survey. Patient Educ. Couns. 57, 294–299 (2005).
Gunn, C. M. et al. Understanding decision making about breast cancer prevention in action: the intersection of perceived risk, perceived control, and social context: NRG oncology/NSABP DMP-1. Med. Decis. Mak. 39, 217–227 (2019).
Witteman, H. O., Zikmund-Fisher, B. J., Waters, E. A., Gavaruzzi, T. & Fagerlin, A. Risk estimates from an online risk calculator are more believable and recalled better when expressed as integers. J. Med. Internet Res. 13, e54 (2011).
Zikmund-Fisher, B. J., Fagerlin, A. & Ubel, P. A. Risky feelings: Why a 6% risk of cancer doesn’t always feel like 6%. Patient Educ. Couns. 81, S87–S93 (2010). S1.
Ozanne, E. M., Howe, R., Omer, Z. & Esserman, L. J. Development of a personalized decision aid for breast cancer risk reduction and management. BMC Med. Inform. Decis. Mak. 14, 4 (2014).
Stata Statistical Software. StataCorp (2017).
Bewick, V., Cheek, L. & Ball, J. Statistics review 14: logistic regression. Crit. Care 9, 112 (2005).
Huilgol, Y. S. et al. Metadata record for the article: elevated risk thresholds predict endocrine risk reducing medication use in the Athena screening registry. figshare (2021).
Huilgol, Y. S. et al. Elevated risk thresholds predict endocrine risk reducing medication use in the Athena screening registry. figshare (2021).
Huilgol, Y. S. et al. Abstract P5-08-01: breast cancer risk thresholds as a predictor of chemoprevention uptake in the Athena Breast Health Network. Cancer Res. 80, P5-08–01 (2020).
Acknowledgements
We acknowledge the central Athena Program Management Office staff. The authors are grateful to the Athena member institution-based program managers, data staff, and Breast Health Specialists for their assistance with data collection. The Athena Breast Health Network is supported by the University of California Office of the President (P0043830 to L.J.E.) and the Safeway Foundation (to L.J.E.). The WISDOM Study is supported by the Patient-Centered Outcomes Research Institute (PCS-1402–10749 to L.J.E) and National Cancer Institute (K08KCA237829 to Y.S. and R01CA237533 to L.J.E.). Data collection and sharing for the WISDOM Study are supported by the National Cancer Institute–funded Breast Cancer Surveillance Consortium (HHSN261201100031C). Part of this work has been presented at the annual San Antonio Breast Cancer Symposium in December 2019 and was awarded the Coltman Scholars Award for outstanding submissions by a clinical scientist-in-training (Huilgol et al., abstract P5-08-01).
Author information
Authors and Affiliations
Consortia
Contributions
Conceptualization (Y.S.H, H.K., L.J.E.); Resources (L.J.E.); Data Acquisition (H.A.C., A.D.B., S.H., A.N., B.A.P., L.J.V., L.J.E.); Data Curation (L.S.); Formal Analysis (Y.S.H., H.K.); Supervision (L.J.E.); Funding Acquisition (Athena Breast Health Network Investigators and Advocate Partners, L.J.E.); Methodology (Y.S.H., L.S., L.J.E.); Writing—Original Draft (Y.S.H., L.J.E.); Project Administration (A.S.F., I.A., M.C.); Writing—Review and Editing (All Authors)
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Huilgol, Y.S., Keane, H., Shieh, Y. et al. Elevated risk thresholds predict endocrine risk-reducing medication use in the Athena screening registry. npj Breast Cancer 7, 102 (2021). https://doi.org/10.1038/s41523-021-00306-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41523-021-00306-9