Abstract
Quorum cheating, a socio-microbiological process that is based on mutations in cell density-sensing (quorum-sensing) systems, has emerged as an important contributor to biofilm-associated infection in the leading human pathogen Staphylococcus aureus. This is because inactivation of the staphylococcal Agr quorum-sensing system leads to pronounced biofilm formation, increasing resistance to antibiotics and immune defense mechanisms. Since biofilm infections in the clinic usually progress under antibiotic treatment, we here investigated whether such treatment promotes biofilm infection via the promotion of quorum cheating. Quorum cheater development was stimulated by several antibiotics used in the treatment of staphylococcal biofilm infections more strongly in biofilm than in the planktonic mode of growth. Sub-inhibitory concentrations of levofloxacin and vancomycin were investigated for their impact on biofilm-associated (subcutaneous catheter-associated and prosthetic joint-associated infection), where in contrast to a non-biofilm-associated subcutaneous skin infection model, a significant increase of the bacterial load and development of agr mutants was observed. Our results directly demonstrate the development of Agr dysfunctionality in animal biofilm-associated infection models and reveal that inappropriate antibiotic treatment can be counterproductive for such infections as it promotes quorum cheating and the associated development of biofilms.
Similar content being viewed by others
Introduction
Healthcare-associated (nosocomial) infections (HAIs) affect an average of 7.6% of hospitalized patients in high-income countries1. In the United States, the mortality due to HAIs has been estimated at ~99,000 annual deaths2 and remains substantial despite some recent decline3. In low-income countries, HAI incidence and mortality are even higher1,4. Many HAIs stem from infections of indwelling medical devices, such as surgical implants, prosthetic devices, and urinary tract, intravenous, or central line-associated catheters5. The frequently fatal outcome of device-associated infections is mostly due to bloodstream infections that originate from the infected devices6,7. For example, central line-associated bloodstream infections (CLABSIs), one of the most deadly types of HAIs, have a mortality rate of 12–25%8. Device-associated infections are notoriously difficult to treat due to the formation of biofilms. Biofilms are bacterial agglomerations that can cover the device’s interior and exterior surface and exhibit pronounced resistance to antibiotics9,10,11,12. For that reason, device-associated infections have remained particularly difficult to treat even by modern drug development strategies13.
One of the most frequent causes of device-associated infections is Staphylococcus aureus14. In comparison to other bacteria often found in these infections, such as the closely related coagulase-negative staphylococci, device-associated infections with S. aureus typically show more severe clinical progression and outcome due to the more pronounced virulence of S. aureus14,15,16. S. aureus is infamous for its exceptional recalcitrance towards antibiotic treatment17, which is in part due to specific antibiotic resistance genes, such as mecA in methicillin-resistant S. aureus (MRSA)17,18. However, even antibiotics that normally efficiently kill MRSA, such as vancomycin, have strongly reduced activity against MRSA in biofilms19,20, and biofilms formed by methicillin-sensitive S. aureus (MSSA) also show pronounced resistance to antibiotic treatment21,22. Therefore, understanding the mechanisms of antibiotic resistance in biofilm infection is essential to improve therapeutic strategies for this major nosocomial pathogen.
Over the last decades, there has been intensive research into the molecular underpinnings of biofilm formation. In S. aureus and other biofilm-forming pathogens, this has led to the identification of a wide variety of molecules that in a structural, metabolic, or regulatory capacity, participate in biofilm formation23,24. For example, quorum-sensing (QS) systems, which adapt bacterial physiology to the changing conditions brought upon by increasing cell density, have a key role in biofilm development in many bacteria25,26. In S. aureus, there is one QS system, which is called Agr for accessory gene regulator27,28. Agr controls several factors that contribute to biofilm development, among them proteases and nucleases that degrade the biofilm matrix and phenol-soluble modulins (PSMs), which are amphipathic peptides that structure biofilms by preventing non-covalent interactions between matrix macromolecules23,29,30. The absence of PSMs leads to decreased formation of biofilm channels and overall thicker and more compact biofilms, to a similarly pronounced degree as seen in agr mutants, indicating a key role of PSMs in biofilm development31. We also confirmed the role of Agr and PSMs in S. aureus and S. epidermidis in models of biofilm-associated infections25,31,32,33,34. However, these represent rather rare examples in which biofilm infection models were used to confirm the validity of in vitro findings25. Generally, the dynamics of biofilm infection remain incompletely understood.
We previously reported that Agr-dysfunctional S. aureus mutants develop in vitro to a considerable extent32. The development of QS-dysfunctional mutants such as S. aureus Agr-dysfunctional mutants are commonly called “quorum cheating” and was first observed for the QS systems of Pseudomonas aeruginosa35. Quorum cheating describes the socio-microbiological phenomenon that some bacteria in a population shut off the costly, QS-controlled secretion of degradative enzymes that are needed for nutrient acquisition, relying on other members of the population until a balanced equilibrium of cheaters and non-cheaters develops36.
While established predominantly using in vitro research, there is evidence that similar principles of quorum cheating and quorum cheating control also apply to in vivo infection37,38. Importantly, we and others have reported that Agr-dysfunctional mutants can be frequently found in S. aureus infection isolates and particularly in those isolated from biofilm-associated infections or blood infections, which often stem from biofilms on infected indwelling devices39,40,41,42,43. Recent animal research in our laboratory has indicated that the development of agr mutants in biofilm-associated infections does not entirely follow predictions from socio-microbiological models32 inasmuch as it is strongly dependent on the specific in vivo setting, with the increased biofilm formation of agr mutants mediating increased resistance to innate immunity mechanisms. In accordance with this apparent key importance of Agr dysfunctionality for immune evasion in a biofilm setting, we also recently found, using analysis of sequential isolates, that Agr-dysfunctional mutants develop during human clinical PJI40, an observation made afterward in similar form in cystic fibrosis44. Notably, in our previous study, clinical biofilms were virtually 100% composed of agr mutants (“quorum cheaters”) rather than of an equilibrium of Agr-functional and -dysfunctional bacteria as the socio-microbiological model would have predicted32. The fact that in this recent clinical study, patients were commonly under antibiotic therapy prompted us to investigate in the present study, using animal models of biofilm infection, whether antibiotic therapy plays a role in the development of antibiotic-resistant biofilms via a possible stimulation of quorum-cheating effects.
Results
Quorum cheater development in biofilm and planktonic settings in vitro
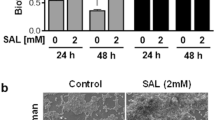
We first analyzed the development of Agr-dysfunctional mutants under treatment with subinhibitory concentrations of antibiotics in vitro, using the common approach to determine hemolytic capacity as a proxy for Agr dysfunctionality32,39,41,45 (Fig. 1a). We used ¼× MIC concentrations for the planktonic and 5× (planktonic) MICs for the biofilm mode of growth40. These concentrations were chosen as they produced similarly modest growth inhibition under the conditions of the experimental setup (Supplementary Fig. 1). Vancomycin (Van), levofloxacin (Lev), and clindamycin (Cli) were chosen as antibiotics for this experiment because these were most frequently used for PJI in our clinic and because we also had used them in our previous study on antibiotic tolerance mediated by Agr-dysfunctional biofilms40. We used the MRSA strain LAC (USA300) for our experiments, which is nowadays a widely used standard strain in S. aureus pathogenesis research. USA300 isolates are the most common cause of community-associated MRSA and a leading cause of hospital-associated MRSA infections in the United States46.
a Experimental setup. For planktonic growth, cultures of S. aureus LAC were inoculated daily into new TSB media at 1/200 volume for 9 days. Levofloxacin (Lev), vancomycin (Van), or clindamycin (Cli) were supplied at ¼× MIC. For biofilm growth, cultures of S. aureus LAC were inoculated at 1/200 volume from pre-cultures into microtiter plate wells containing 200 μl of TSBg each and grown for 48 h to form a biofilm. Then, the supernatant was gently removed, and 200 μl TSBg containing Lev, Van, or Cli was dispensed into the wells at 5× MIC In the following 9 days, every 3 days, the old supernatant was gently removed and replaced with fresh TSBg (200 μl) with the respective antibiotics. b, c Results for planktonic (b) and biofilm (c) growth. Agr dysfunctionality was assessed by hemolysis on sheep agar plates. n = 3/group and time point. Error bars show the mean ± SD. Statistical analysis is done by two-way ANOVAs with Dunnett’s post-tests versus control values.
In this experiment, we passaged cultures by daily inoculation of fresh growth media with 1/200 volume of the cultures in the planktonic mode setup. For the biofilm setup, as biofilms cannot be quantitatively transferred, we exchanged the supernatant on top of the biofilms grown in microtiter plate wells every three days with fresh growth medium. We found that the applied subinhibitory concentrations of antibiotics revealed significant effects on the development of quorum cheaters (Fig. 1b, c). Furthermore—although the planktonic and biofilm experimental setups are certainly difficult to directly compare—these antibiotic-dependent effects appeared earlier (already at 3 versus only at 6 days) and were more pronounced (a consistent increase of ~50% over the 3–9 days’ time range) in the biofilm than a planktonic mode of growth.
Impact of low-dose antibiotic concentrations on the development of biofilm- and non-biofilm-associated infection
Then, we proceeded to our main goal of analyzing quorum cheating under antibiotic treatment during experimental infection. To that end, we again used strain LAC (USA300) and mouse infection models of biofilm-associated and non-biofilm-associated subcutaneous skin infection (Fig. 2a). Except for device insertion, these two models are very similar and thus offer the possibility to compare for the effect of device (biofilm) involvement. Antibiotic treatment was initiated at day 6 post-infection (in both skin abscess and catheter infection models) and repeated another two times every 24 h, for a total of 3 days, after which CFU was counted. For the investigation of the impact of antibiotics, we focused on Van and Lev and used a low-dose regimen corresponding to ~1/8 of the mouse body weight-corrected dose suggested for the clinical treatment of bone and joint infections47. This was intended to mimic the situation frequently encountered during the treatment of device-associated infections, where the applied dosage is subinhibitory due to increased tolerance to antibiotics of the device-associated biofilms, resulting in the persistence of the infection. The low-dose regimen was also necessary because of the comparison to non-catheter-associated skin infection, where higher doses would have rapidly killed all bacteria.
a Experimental setup. Female, 6–8 weeks old C57BL/6 were used. For antibiotic treatment, mice received antibiotics starting on day 6 after infection (catheter and skin abscess models) every 24 h for 3 days until the end of the experiment. Controls received no antibiotic. Mice received intraperitoneal injections of 0.25 ml containing 0.3 mg ml−1 Van (3.75 mg kg−1) or oral doses of 0.4 ml containing 0.04 mg ml−1 Lev (0.8 mg kg−1). All mice in one infection type were infected with the same CFU (skin abscess, ~1 × 107 CFU; catheter infection, 1 × 103–104 CFU with actual adherent bacterial numbers tested.) b, c Results obtained with infection by S. aureus LAC wild-type with and without antibiotics. d, e Results obtained with infection by S. aureus LAC wild-type versus isogenic Δagr mutant. f, g Results obtained with infection by S. aureus LAC Δagr with and without antibiotics. n = 6 (b, d, f); n = 8 (c, e, g). h Representative infected or control (no infection) catheter pieces stained with PI or WGA-Alexa FluorTM 350. Statistical analysis is 1-way ANOVA (b, f) or Kruskal–Wallis (c, g), with Dunnett’s post-tests versus data obtained with wild-type control, Mann–Whitney test (d), and unpaired, two-tailed t-test (e). Parametric versus non-parametric tests were chosen based on normal distribution (Shapiro–Wilk) tests for the data in the respective comparisons. Error bars show the geometric mean and geometric SD.
As intended, treatment with Van or Lev only slightly and did not significantly reduce CFU in the skin abscess model (Fig. 2b). Contrastingly, in the biofilm-associated subcutaneous catheter model, CFU was increased by the addition of antibiotics, which was significant for Lev (Fig. 2c). Hypothesizing that the underlying reasons were associated with quorum cheating and its effect on biofilm-mediated resistance, we first determined the behavior of a constructed isogenic QS (Δagr) mutant versus wild-type LAC. In accordance with what we showed previously32, the Δagr mutant had strongly and significantly decreased infectivity in the skin abscess model (Fig. 2d), as expected from the control by Agr of several virulence factors that are known to be crucial in that setting, such as PSMs or α-toxin48,49. In contrast, the Δagr strain showed significantly higher infectivity than the wild-type strain in the biofilm-associated catheter infection model (Fig. 2e). In the skin abscess model, both Van and Lev treatment led to significantly reduced CFU (Fig. 2f), indicating that in vivo resistance to the used antibiotic concentrations is strongly diminished in the Δagr strain, a likely consequence of the strongly diminished bacterial survival capacities that are associated with Agr dysfunctionality in that setting32,49. Notably, the significant increase in CFU in the biofilm-associated catheter infection model that we observed with antibiotic treatment and infection by wild-type S. aureus was not observed with the isogenic Δagr strain (Fig. 2g), suggesting that Agr quorum sensing is causally related to this phenomenon. We also stained catheters with PI or WGA-Alexa FluorTM 350, which stain biofilm extracellular DNA or polysaccharide, respectively, confirming that antibiotics increased biofilm formation in the LAC but not Δagr-infected animals (Fig. 2h).
The short-duration experiment (6 plus 3 days) was chosen to be able to compare directly to non-biofilm-associated skin infection, in which pathogenesis-related phenotypes occur early. However, because effects in the catheter infection model were not very pronounced at 9 (6 plus 3) days post-infection, only reaching significance for Lev in the important comparison shown in Fig. 2c, we performed an additional catheter infection experiment in which we prolonged the infection and took samples at 6 plus 1, 3, or 9 days to obtain time-dependent data (Fig. 3a). The phenomenon of increased infectivity under antibiotic treatment developed over time, reaching significance at 3 and 9 days for Lev and at 9 days for Van, but was completely absent in mice that were infected with Δagr instead of wild-type S. aureus (Fig. 3b, c).
a Experimental setup. Mice were implanted with catheters with 1 × 103–104 adherent bacterial CFU and received intraperitoneal injections of 0.25 ml containing 0.3 mg ml−1 Van (3.75 mg kg−1) or oral doses of 0.4 ml containing 0.04 mg ml−1 Lev (0.8 mg kg−1) daily for 9 days after infection. Controls received no antibiotic. Different groups of mice (n = 6/group) were euthanized on days 1, 3, or 9 after initiation of antibiotic treatment. b, c CFU on the catheters in the different groups after euthanizing. Statistical analysis is by Mann–Whitney tests. Error bars show the geometric mean and geometric SD. d, e Agr (QS) dysfunctionality was assessed by hemolysis on sheep agar plates. Statistical analysis is by Fisher’s exact test at every time point based on the underlying raw data (hemolysis phenotype) of analyzed clones.
Furthermore, we used an additional biofilm-associated infection model, a model of PJI, to corroborate our results obtained in the catheter infection model (Fig. 4a). In this model, we also observed significantly increased CFU in Δagr as compared to LAC-infected animals and increased CFU in LAC but not Δagr-infected animals under antibiotic treatment (reaching statistical significance with Lev) (Fig. 4b–d).
a Experimental setup. Female, 6–8 weeks old C57BL/6 were used. For antibiotic treatment, mice received antibiotics starting on day 14 after infection every 24 h for 7 days until the end of the experiment. Controls received no antibiotic. Mice received intraperitoneal injections of 0.25 ml containing 0.3 mg ml−1 Van (3.75 mg kg−1) or oral doses of 0.4 ml containing 0.04 mg ml−1 Lev (0.8 mg kg−1). All mice were infected with the same CFU (~1 × 107 CFU in 50 μl, intra-articular injection). b Results obtained with infection by S. aureus LAC wild-type with and without antibiotics. c Results obtained with infection by S. aureus LAC wild-type versus isogenic Δagr mutant. d Results obtained with infection by S. aureus LAC Δagr with and without antibiotics. n = 8. Statistical analysis is 1-way ANOVA with Dunnett’s post-tests versus data obtained with wild-type control (b, d) and by unpaired, two-tailed t-test (c). Error bars show the geometric mean and geometric SD.
Development of quorum cheaters during biofilm- and non-biofilm-associated infection with low-dose antibiotic concentrations
If our hypothesis is correct that QS dysfunctionality underlies the observed increased infectivity under antibiotic treatment in the biofilm-associated models, we expect to detect the development of quorum cheaters during infection with wild-type S. aureus. To confirm this hypothesis, we determined the hemolytic capacity of isolates as a readout for Agr functionality at the end of the infection. While Agr-dysfunctional mutants were not detected in non-catheter (non-biofilm)-associated skin infection under any condition, they developed in a catheter (biofilm)-associated infection at significantly higher rates (Table 1). Importantly, the rate of Agr-dysfunctional mutant development in catheter-associated infection was further increased significantly under treatment with Lev or Van. Similar observations were made in the PJI model, where no Agr-dysfunctional mutants were observed without, but at significant rates with Lev or Van treatment (Table 1). All non-hemolytic clones interpreted as agr mutants were confirmed by DNA sequencing to harbor non-synonymous mutations in the Agr system (Tables 2 and 3). As reported previously for agr mutations that occur in vitro or in vivo32,40,41, mutations mapped to the agrA or agrC genes. Interestingly, we frequently detected the same mutation in two or more isolates from one mouse, indicating the proliferation of agr-mutated clones. Finally, while the percentage of QS mutants after 6 plus 3 days of intervention was still low, it is important to stress that in our time-extended antibiotic intervention model, the percentage of QS mutants that were detected after 6 plus 9 days was substantial (Lev > 10%; Van > 2% of the entire population) (Fig. 3d, e). The mouse biofilm-associated infection models can barely be further extended because the infections heal. Nevertheless, these data indicate that QS mutants can develop and substantially proliferate during antibiotic treatment of biofilm-associated infection. Because the biofilm phenotypes we observed with low-dose antibiotics can theoretically also be due to reduced Agr expression under those conditions, we analyzed whether low-dose antibiotic treatment leads to changes in agr expression. While it is difficult to estimate the actual in vivo concentrations at the biofilm infection site, we used the 5× MIC concentrations we had employed in the in vitro experiment shown in Fig. 1c for that purpose. We believe that the moderate growth inhibition observed with those concentrations in vitro indicates that they are at least as high as those encountered in vivo because we did not observe growth inhibition in vivo with the used antibiotic concentrations at the initial 1-day time points. There was no inhibition of agr expression, as measured by qRT-PCR of the agrA gene, by 5× MIC of Lev, Van, or Cli (Supplementary Fig. 2). For all three antibiotics, agr expression, in fact, rather increased.
Altogether, our findings show that antibiotic treatment can exacerbate device-associated S. aureus infection and mechanistically link this phenomenon to the increased frequency of development and proliferation of biofilms composed of Agr-dysfunctional mutants that exhibit increased antibiotic resistance.
Discussion
The exceptional capacity of S. aureus and other pathogens to colonize indwelling medical devices to cause persistent, antibiotic-resistant biofilm infections has mainly been attributed to the presence of specific genes, such as those coding for biofilm matrix polysaccharides or proteins25,50,51. While such biofilm-associated factors are certain prerequisites for the initiation and persistence of biofilm infection, and the infection environment can also lead to changes in their expression52, recent work performed in our laboratories and elsewhere indicates that device-associated infection is a dynamic process with genetic adaptations that play an important role in the progress of such infections. Specifically, mutations in the Agr QS system have now been recognized as defining genetic adaptations developing during and exacerbating S. aureus device-associated infection by their increased propensity to form biofilms31,32,34,40,53,54, explaining the frequent isolation of such mutants from these infections34,39,41.
Because clinical device-associated infections commonly progress under antibiotic treatment, in this study, we aimed to directly investigate whether antibiotic treatment can impact device-associated infections by potentially stimulating quorum cheating, i.e., stimulating the rise of agr mutants. In vitro, antibiotics led to earlier and more pronounced development of quorum cheaters in biofilm than in the planktonic mode of growth. More importantly, we show that a low-dose antibiotic regimen exacerbated biofilm-associated infection and was associated with a concomitant rise and proliferation of agr mutants.
Our findings are consistent with a model (shown in Fig. 5) in which the persistence of spontaneously arising Agr-dysfunctional QS mutants during biofilm-associated infection is promoted by antibiotic treatment. As our previous investigations have shown32,40, biofilms composed of agr mutants have increased resistance to antibiotics and leukocyte attacks; thus, the development of Agr-dysfunctional biofilms during clinical biofilm-associated infection is likely to be explained by the selective pressure exerted by a combination of these two mechanisms.
Naturally, skin-colonizing S. aureus contaminates the indwelling medical device (shown as a subcutaneous catheter, as an example) during insertion. Initial colonization of the device by contaminating bacteria ensues. Spontaneous mutations in the agr locus happen in some bacteria, producing Agr-dysfunctional S. aureus. During prolonged infection under selective pressure by antibiotics (vancomycin, levofloxacin), Agr-dysfunctional mutants outgrow wild-type members of the population. As a result, a strong biofilm forms, considerably increasing antibiotic resistance and resistance to leukocyte attacks. This leads to the exacerbation of device infection, which can involve bacteremia and systemic dissemination.
These findings have important clinical implications. The most striking message from our study is that antibiotic treatment at concentrations that do not eradicate the infection—which is the very problem encountered in the case of device-associated infections—can trigger the rise of Agr-dysfunctional quorum cheater mutants and thereby further exacerbate the infection.
Our study has limitations. We only used selected antibiotics for our study. However, we believe that our results can be generalized because (i) the antibiotics we chose cover those frequently used in the clinic, (ii) represent entirely different modes of action (DNA synthesis, cell wall synthesis), and (iii) antibiotic tolerance by biofilm formation is generally recognized to be non-specific. Furthermore, due to limits of how long mouse biofilm-associated experimental infection can be maintained, we were not able to prolong infection until the complete overtake of quorum cheaters that we saw in chronic clinical biofilm infection40 could be observed. However, given the considerable expansion of quorum cheaters that we observed in the mouse model during 2 weeks of infection, we believe it is reasonable to assume further spread to the point observed in long-term human infection. In addition, the strong increase under antibiotic treatment, which represents the main message of this study, was clearly visible during the monitored timeframe. Finally, we acknowledge that there may be additional mechanisms unrelated to biofilm formation that facilitate survival of Agr-dysfunctional mutants in persistent infection, such as intracellular survival in host cells, which has been linked to PSMs55. While intracellular persistence was not addressed in our study, it has been linked to factors other than Agr, such as small colony variants or the regulator Rsp56,57, mutations associated with which were not identified in our previous human study that monitored mutations arising during biofilm infection40.
Methods
Bacterial strains and growth conditions
S. aureus LAC (pulsed-field type USA300) was obtained from NARSA (Network on Antimicrobial Resistance in S. aureus). The isogenic agr mutant of S. aureus USA300 LAC has been described previously48. The entire agr system is deleted in this mutant, which has been produced via phage transduction from strain RN691158. All strains were stored in tryptic soy broth (TSB and BD) supplemented with 30% glycerol at −80 °C. For pre-cultures, which were used to inoculate main cultures in the various experiments as indicated, bacteria were grown on solid agar plates containing TSB for ~24 h, from which single clones were used for inoculation. Planktonic cultures were grown under shaking conditions (200 rpm) in TSB, and biofilm cultures in microtiter plates in TSBg (TSB plus 0.5% glucose) without shaking. All bacterial cultures were grown at 37 °C.
Analysis of QS dysfunctionality and agr sequencing
Similarly to several previous studies32,39,41,45, we used hemolytic activity upon plating on sheep blood agar as a readout for Agr functionality. Most mutants that lose hemolytic capacity reportedly show spontaneous mutations in the Agr system32,39,41,45. In key in vivo experiments, we sequenced the agrA and agrC genes of the non-hemolytic clones with primers agrACforward (5′-GCTATACAGTGCATTTGCTAG-3′) and agrACreverse (5′-TCGCAGCTTATAGTACTTGTG-3′).
In-vitro development of Agr-dysfunctional mutants
For the planktonic mode of growth, cultures were grown in TSB for 24 h in 15 ml round-bottom tubes, and fresh cultures were inoculated every day for 9 days using 1/200 volume of the previous culture in only TSB (control) or TSB with levofloxacin (Lev), vancomycin (Van), or clindamycin (Cli) at ¼ MIC. The MICs determined for strain LAC against antibiotics used in this study were: 1 μg/ml (Van), 4 μg/ml (Lev), and 0.3 μg/ml (Cli). On days 3, 6, and 9, dilutions were plated on sheep blood agar, and hemolysis was evaluated after overnight incubation at 37 °C. For the biofilm mode of growth, cultures of S. aureus LAC were inoculated at 1/200 volume from pre-cultures into microtiter plate wells containing 200 μl of TSBg and grown for 48 h to form a biofilm. Then, the supernatant was gently removed, and 200 μl TSBg containing Lev, Van, or Cli was dispensed into the wells at 5× MIC. In the following 9 days, every 3 days, the old supernatant was gently removed and replaced with fresh TSBg (200 μl) with the respective antibiotics.
Antimicrobial resistance profiles
The antimicrobial susceptibilities of isolates were determined by the disc diffusion method on Mueller–Hinton agar according to Clinical and Laboratory Standards Institute (CLSI) guidelines. S. aureus ATCC29213 was used as a quality control.
Quantitative real-time reverse transcription polymerase chain reaction (qRT-PCR)
The total RNA of S. aureus was extracted using an RNA extraction reagent (Takara RR047A), then complementary DNA was synthesized from the total RNA by using the RT reagent Kit (Takara, RR037A). Amplification of the resulting complementary DNA sample was performed with the TB Green® Fast qPCR Mix (Takara, RR430A). The 7500 Sequence Detector (Applied Biosystems) was used to perform reactions in MicroAmp Optical 96-well reaction plates. Oligonucleotides used were as follows (5′–3′): gyrB-F, CAAATGATCACAGCATTTGGTACAG, gyrB-R, CGGCATCAGTCATAATGACGAT, agrA-F, GCACATACACGCTTACAATTATTA, agr-R, ACACTGAATTACTGCCACGTTTTAA.
Animal experiments
Female C57BL/6 mice were purchased from JSJ Corp. (originally introduced from Jackson Laboratory) and used for all mouse experiments. All mice were between 6 and 8 weeks of age at the time of use. All animals were euthanized by CO2 at the end of the studies. In the antibiotic treatment experiments, mice received antibiotics every 24 h starting on day 6 after infection (catheter and skin infection models) or day 14 after infection (PJI) every 24 h until the end of the experiment. Controls received no antibiotic. Van and Lev were dissolved in water to a concentration of 0.3 mg ml−1 or 0.04 mg ml−1, respectively, and solutions were filter-sterilized. Mice received intraperitoneal injections of 0.25 ml containing 0.3 mg ml−1 Van (3.75 mg kg−1) or oral doses of 0.4 ml containing 0.04 mg ml−1 Lev (0.8 mg kg−1). Investigators were blinded to group allocation when determining CFU.
Skin abscess model. About 1 × 107 CFU of bacteria in 50 μl of PBS were injected subcutaneously into the left and/or right flank of shaved mice. To determine the bacterial load, abscesses on day 9 were surgically removed, cut into small pieces and split into four separate tubes containing 500 mg of borosilicate glass beads and 500 μl of sterile PBS. The skin pieces were homogenized in a FastPrep 96 (MP Bio) homogenizer, 5 × 1 min at 1800 rpm. The homogenates were then plated, incubated at 37 °C for 24 h, and enumerated.
Catheter infection model. The catheter infection model was performed essentially as described previously32. Briefly, 1-cm catheter pieces (Surflo® Teflon i.v. catheters, 14 ×2”) were coated with equal numbers of bacteria. Adherence was tested in control experiments and was in the same range ( ~ 1 × 103–104). Catheters were then inserted under the dorsal skin of mice. Catheters were removed carefully from the skin on days 7, 9, and 15 after infection, and CFU on the catheters and the directly adjacent tissue were determined by plating as above after performing a validated sonication protocol to disrupt bacterial agglomerates on the catheters and homogenizing the tissue samples using the FastPrep 96 (MP Bio) homogenizer, 5 × 1 min. The sonication protocol consisted of sonication of harvested catheters for 5 min in 1 ml PBS in 2 ml tubes in an Ultra Sonic Cleaner, followed by vortexing for 15 min on a Vortex-Genie2. Some catheters obtained on day 9 after infection were also fixed with 2.5% glutaraldehyde in 0.1 M PBS for 30 min and then stained either with 10 μM propidium iodide (Yeasen, Shanghai) (staining extracellular DNA) for 15 min or 2.5 μg/ml wheat germ agglutinin (WGA)-Alexa FluorTM 350 (Invitrogen, W11263) (staining staphylococcal biofilm exopolysaccharide) for 20 min. Stained catheters were then washed with PBS and longitudinally placed in wells of a 96-well sterile, tissue culture-treated microplate with black well walls and an optically clear cyclic olefin bottom and imaged using an Agilent BioTek Lionheart FX Automated Microscope using the confocal channel (555 nm laser for the PI-stained staphylococcal biofilm and 350 nm laser for the WGA-stained staphylococcal biofilm) with the 4× objective.
PJI model. For the PJI model, mice underwent unilateral proximal tibial implant insertion with a 10-mm syringe needle from a 1-ml BD insulin syringe (29 G × 1/2”, 0.33 mm × 12.7 mm) using a previously described surgical technique59. Following press-fit implant insertion and arthrotomy closure, a gas-tight syringe (65 RN, Hamilton) was utilized to administer a 50-μl intra-articular injection of bacteria with ~ 1 × 107 CFU. Beginning CFU dosing was verified through parallel syringe injections placed directly in triplicate onto sheep blood agar plates. On day 21 after infection, mice were euthanized by CO2. Each of the whole unilateral tibial implant with the syringe needle and the directly surrounding tissue was removed and CFU were determined by plating as above, after performing a validated sonication protocol (see above) to disrupt bacterial agglomerates on the total unilateral tibial implant, and homogenizing the tissue samples using the FastPrep 96 (MP Bio) homogenizer, 5 × 1 min.
Statistics
Statistical analysis was performed using GraphPad Prism version 9.3.1 for Mac OS. Unpaired, two-tailed t-tests or Mann–Whitney tests were used for the comparison of two groups depending on the results of Shapiro–Wild tests for normality of distribution, and 1-way or 2-way ANOVAs, or Kruskal–Wallis tests, as applicable and depending on Shapiro-Wilk tests, for the comparison of more than two groups. The specific tests used are indicated in the figure legends. For arithmetic scales, error bars depict the standard deviation (SD) and lines depict the mean. For logarithmic scales, the geometric mean with the geometric SD is depicted. All replicates are independent.
Graphics software and pictures
Illustrations were made using Biorender and Adobe Illustrator under NIAID licenses. Mouse pictures are from Vecteezy.com.
Inclusion and ethics
All animal work complied with all relevant ethical regulations and was approved by the Ethics Committee of Ren Ji Hospital, School of Medicine, Shanghai Jiao Tong University, Shanghai, China (Approval Number: KY2021-225-B).
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
All data generated or analyzed during this study are included in this published article or in the supplementary information files. The S. aureus LACΔagr strain is available from Dr. Min Li or Dr. Michael Otto subject to a simple transfer agreement.
References
WHO. Report on the burden of endemic health care-associated infection worldwide. (2011).
Klevens, R. M. et al. Estimating health care-associated infections and deaths in U.S. hospitals, 2002. Public Health Rep. 122, 160–166 (2007).
CDC. Healthcare-Associated Infections (HAIs). https://www.cdc.gov/winnablebattles/report/HAIs.html.
Allegranzi, B. et al. Burden of endemic health-care-associated infection in developing countries: systematic review and meta-analysis. Lancet 377, 228–241 (2011).
Darouiche, R. O. Device-associated infections: a macroproblem that starts with microadherence. Clin. Infect. Dis. 33, 1567–1572 (2001).
Luzum, M., Sebolt, J. & Chopra, V. Catheter-associated urinary tract infection, Clostridioides difficile Colitis, central line-associated bloodstream infection, and methicillin-resistant Staphylococcus aureus. Med. Clin. N. Am. 104, 663–679 (2020).
Yousif, A., Jamal, M. A. & Raad, I. Biofilm-based central line-associated bloodstream infections. Adv. Exp. Med. Biol. 830, 157–179 (2015).
O’Grady, N. P. et al. Guidelines for the prevention of intravascular catheter-related infections. Centers for Disease Control and Prevention. MMWR Recomm. Rep. 51, 1–29 (2002).
Stewart, P. S. & Costerton, J. W. Antibiotic resistance of bacteria in biofilms. Lancet 358, 135–138 (2001).
Wi, Y. M. & Patel, R. Understanding biofilms and novel approaches to the diagnosis, prevention, and treatment of medical device-associated infections. Infect. Dis. Clin. N. Am. 32, 915–929 (2018).
Arciola, C. R., Campoccia, D. & Montanaro, L. Implant infections: adhesion, biofilm formation and immune evasion. Nat. Rev. Microbiol. 16, 397–409 (2018).
Mah, T. F. & O’Toole, G. A. Mechanisms of biofilm resistance to antimicrobial agents. Trends Microbiol. 9, 34–39 (2001).
Dickey, S. W., Cheung, G. Y. C. & Otto, M. Different drugs for bad bugs: antivirulence strategies in the age of antibiotic resistance. Nat. Rev. Drug Discov. 16, 457–471 (2017).
Zheng, Y., He, L., Asiamah, T. K. & Otto, M. Colonization of medical devices by staphylococci. Environ. Microbiol. 20, 3141–3153 (2018).
Otto, M. Staphylococcus aureus toxins. Curr. Opin. Microbiol. 17, 32–37 (2014).
Darouiche, R. O. Treatment of infections associated with surgical implants. N. Engl. J. Med. 350, 1422–1429 (2004).
Chambers, H. F. & Deleo, F. R. Waves of resistance: Staphylococcus aureus in the antibiotic era. Nat. Rev. Microbiol. 7, 629–641 (2009).
Klein, E., Smith, D. L. & Laxminarayan, R. Hospitalizations and deaths caused by methicillin-resistant Staphylococcus aureus, United States, 1999-2005. Emerg. Infect. Dis. 13, 1840–1846 (2007).
Abdelhady, W. et al. Reduced vancomycin susceptibility in an in vitro catheter-related biofilm model correlates with poor therapeutic outcomes in experimental endocarditis due to methicillin-resistant Staphylococcus aureus. Antimicrob. Agents Chemother. 57, 1447–1454 (2013).
Jones, S. M., Morgan, M., Humphrey, T. J. & Lappin-Scott, H. Effect of vancomycin and rifampicin on meticillin-resistant Staphylococcus aureus biofilms. Lancet 357, 40–41 (2001).
Marques, C. et al. Effects of antibiotics on biofilm and unattached cells of a clinical Staphylococcus aureus isolate from bone and joint infection. J. Med. Microbiol. 64, 1021–1026 (2015).
El-Azizi, M., Rao, S., Kanchanapoom, T. & Khardori, N. In vitro activity of vancomycin, quinupristin/dalfopristin, and linezolid against intact and disrupted biofilms of staphylococci. Ann. Clin. Microbiol. Antimicrob. 4, 2 (2005).
Schilcher, K. & Horswill, A. R. Staphylococcal biofilm development: structure, regulation, and treatment strategies. Microbiol. Mol. Biol. Rev. https://doi.org/10.1128/MMBR.00026-19 (2020).
Otto, M. Staphylococcal biofilms. Microbiol. Spectr. https://doi.org/10.1128/microbiolspec.GPP3-0023-2018 (2018).
Joo, H. S. & Otto, M. Molecular basis of in vivo biofilm formation by bacterial pathogens. Chem. Biol. 19, 1503–1513 (2012).
Parsek, M. R. & Greenberg, E. P. Sociomicrobiology: the connections between quorum sensing and biofilms. Trends Microbiol. 13, 27–33 (2005).
Le, K. Y. & Otto, M. Quorum-sensing regulation in staphylococci—an overview. Front. Microbiol. 6, 1174 (2015).
Novick, R. P. & Geisinger, E. Quorum sensing in staphylococci. Annu. Rev. Genet. 42, 541–564 (2008).
Cheung, G. Y., Joo, H. S., Chatterjee, S. S. & Otto, M. Phenol-soluble modulins-critical determinants of staphylococcal virulence. FEMS Microbiol. Rev. 38, 698–719 (2014).
Otto, M. Staphylococcal infections: mechanisms of biofilm maturation and detachment as critical determinants of pathogenicity. Annu. Rev. Med. 64, 175–188 (2013).
Periasamy, S. et al. How Staphylococcus aureus biofilms develop their characteristic structure. Proc. Natl Acad. Sci. USA 109, 1281–1286 (2012).
He, L. et al. Resistance to leukocytes ties benefits of quorum sensing dysfunctionality to biofilm infection. Nat. Microbiol. 4, 1114–1119 (2019).
Le, K. Y. et al. Role of phenol-soluble modulins in Staphylococcus epidermidis biofilm formation and infection of indwelling medical devices. J. Mol. Biol. 431, 3015–3027 (2019).
Vuong, C., Kocianova, S., Yao, Y., Carmody, A. B. & Otto, M. Increased colonization of indwelling medical devices by quorum-sensing mutants of Staphylococcus epidermidis in vivo. J. Infect. Dis. 190, 1498–1505 (2004).
Sandoz, K. M., Mitzimberg, S. M. & Schuster, M. Social cheating in Pseudomonas aeruginosa quorum sensing. Proc. Natl Acad. Sci. USA 104, 15876–15881 (2007).
Dandekar, A. A., Chugani, S. & Greenberg, E. P. Bacterial quorum sensing and metabolic incentives to cooperate. Science 338, 264–266 (2012).
Pollitt, E. J., West, S. A., Crusz, S. A., Burton-Chellew, M. N. & Diggle, S. P. Cooperation, quorum sensing, and evolution of virulence in Staphylococcus aureus. Infect. Immun. 82, 1045–1051 (2014).
Rumbaugh, K. P. et al. Kin selection, quorum sensing and virulence in pathogenic bacteria. Proc. Biol. Sci. 279, 3584–3588 (2012).
Fowler, V. G. Jr. et al. Persistent bacteremia due to methicillin-resistant Staphylococcus aureus infection is associated with agr dysfunction and low-level in vitro resistance to thrombin-induced platelet microbicidal protein. J. Infect. Dis. 190, 1140–1149 (2004).
He, L. et al. Key role of quorum-sensing mutations in the development of Staphylococcus aureus clinical device-associated infection. Clin. Transl. Med. 12, e801 (2022).
Traber, K. E. et al. agr function in clinical Staphylococcus aureus isolates. Microbiology (Reading) 154, 2265–2274 (2008).
Kang, C. K. et al. Agr functionality affects clinical outcomes in patients with persistent methicillin-resistant Staphylococcus aureus bacteraemia. Eur. J. Clin. Microbiol. Infect. Dis. 36, 2187–2191 (2017).
Suligoy, C. M. et al. Mutation of Agr is associated with the adaptation of Staphylococcus aureus to the host during chronic osteomyelitis. Front. Cell Infect. Microbiol. 8, 18 (2018).
Ramond, E. et al. Lung-adapted Staphylococcus aureus isolates with dysfunctional agr system trigger a proinflammatory response. J. Infect. Dis. 226, 1276–1285 (2022).
Shopsin, B. et al. Mutations in agr do not persist in natural populations of methicillin-resistant Staphylococcus aureus. J. Infect. Dis. 202, 1593–1599 (2010).
Carrel, M., Perencevich, E. N. & David, M. Z. USA300 methicillin-resistant Staphylococcus aureus, United States, 2000-2013. Emerg. Infect. Dis. 21, 1973–1980 (2015).
Liu, C. et al. Clinical practice guidelines by the infectious diseases society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children: executive summary. Clin. Infect. Dis. 52, 285–292 (2011).
Wang, R. et al. Identification of novel cytolytic peptides as key virulence determinants for community-associated MRSA. Nat. Med. 13, 1510–1514 (2007).
Kobayashi, S. D. et al. Comparative analysis of USA300 virulence determinants in a rabbit model of skin and soft tissue infection. J. Infect. Dis. 204, 937–941 (2011).
Donlan, R. M. & Costerton, J. W. Biofilms: survival mechanisms of clinically relevant microorganisms. Clin. Microbiol. Rev. 15, 167–193 (2002).
Hall-Stoodley, L., Costerton, J. W. & Stoodley, P. Bacterial biofilms: from the natural environment to infectious diseases. Nat. Rev. Microbiol. 2, 95–108 (2004).
Fluckiger, U. et al. Biofilm formation, icaADBC transcription, and polysaccharide intercellular adhesin synthesis by staphylococci in a device-related infection model. Infect. Immun. 73, 1811–1819 (2005).
Vuong, C., Gerke, C., Somerville, G. A., Fischer, E. R. & Otto, M. Quorum-sensing control of biofilm factors in Staphylococcus epidermidis. J. Infect. Dis. 188, 706–718 (2003).
Vuong, C., Saenz, H. L., Gotz, F. & Otto, M. Impact of the agr quorum-sensing system on adherence to polystyrene in Staphylococcus aureus. J. Infect. Dis. 182, 1688–1693 (2000).
Siegmund, A. et al. Intracellular persistence of Staphylococcus aureus in endothelial cells is promoted by the absence of phenol-soluble modulins. Virulence 12, 1186–1198 (2021).
Fraunholz, M. & Sinha, B. Intracellular Staphylococcus aureus: live-in and let die. Front. Cell Infect. Microbiol. 2, 43 (2012).
Das, S. et al. Natural mutations in a Staphylococcus aureus virulence regulator attenuate cytotoxicity but permit bacteremia and abscess formation. Proc. Natl Acad. Sci. USA 113, E3101–E3110 (2016).
Kornblum, J., Kreiswirth, B. N., Projan, S. J., Ross, H. & Novick, R. P. in Molecular biology of the Staphylococci (ed R. P. Novick) 373–402 (VCH Publishers, Inc.).
Yang, X. et al. Intermittent parathyroid hormone enhances cancellous osseointegration of a novel murine tibial implant. J. Bone Joint Surg. Am. 97, 1074–1083 (2015).
Acknowledgements
Funding: This study was supported by the National Natural Science Foundation of China [Grant nos. 82272395 and 81974311 (to L.H.), 81873957 and 82172325 (to M.L.), 81772364 (to H.S.)], the Shanghai Pujiang Program [grant number 2019PJD026 (to L.H.)], the Medical Guidance Scientific Research Support Project of the Shanghai Science and Technology Commission [grant number 19411962600 (to H.S.)], and the Intramural Research Program of the National Institute of Allergy and Infectious Diseases (NIAID), U.S. National Institutes of Health (NIH) [project number ZIA AI001080 (to M.O.)]. The funders had no role in the study design, collection, analysis, and interpretation of data, writing of the report, or in the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
Conceptualization: M.O. Methodology: L.H., M.O., and M.L. Investigation: L.H., H.L., Y.W., F.J., Q.L., F.Z., and H.W. Visualization: L.H. and M.O. Funding acquisition: L.H., H.S., M.L., and M.O. Supervision: L.H., H.S., and M.L. Writing—original draft: L.H. and M.O. Writing—review & editing: L.H., M.L., and M.O.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
He, L., Lv, H., Wang, Y. et al. Antibiotic treatment can exacerbate biofilm-associated infection by promoting quorum cheater development. npj Biofilms Microbiomes 9, 26 (2023). https://doi.org/10.1038/s41522-023-00394-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41522-023-00394-4
This article is cited by
-
The role of Staphylococcus aureus quorum sensing in cutaneous and systemic infections
Inflammation and Regeneration (2024)
-
Recent advances in single-cell engineered live biotherapeutic products research for skin repair and disease treatment
npj Biofilms and Microbiomes (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.