Abstract
Bacterial vaginosis (BV) is a condition in which the vaginal microbiome presents an overgrowth of obligate and facultative anaerobes, which disturbs the vaginal microbiome balance. BV is a common and recurring vaginal infection among women of reproductive age and is associated with adverse health outcomes and a decreased quality of life. The current recommended first-line treatment for BV is antibiotics, despite the high recurrence rate. Live biopharmaceutical products/probiotics and vaginal microbiome transplantation (VMT) have also been tested in clinical trials for BV. In this review, we discuss the advantages and challenges of current BV treatments and interventions. Furthermore, we provide our understanding of why current clinical trials with probiotics have had mixed results, which is mainly due to not administering the correct bacteria to the correct body site. Here, we propose a great opportunity for large clinical trials with probiotic strains isolated from the vaginal tract (e.g., Lactobacillus crispatus) and administered directly into the vagina after pretreatment.
Similar content being viewed by others
Introduction
The vaginal microbiome is commonly dominated by one species of Lactobacillus (e.g., L. crispatus, L. gasseri, L. iners, or L. jensenii)1,2,3. Some women have a vaginal microbiome that is dominated by non-Lactobacillus species, especially Black and Hispanic women4. Bacterial vaginosis (BV) is a condition in which the vaginal microbiome has a deficiency of lactic acid-producing bacteria with increased numbers of anaerobic bacteria such as Gardnerella, Atopobium, Megasphera, Prevotella, and Sneathia1,2,3. Common BV symptoms include vaginal discharge, increased vaginal pH, itching, fish-like odor, and burning when urinating5. Given the high percentage of women with low vaginal Lactobacillus spp. abundance but lacking BV symptoms, whether these women are healthy or have asymptomatic BV has remained a subject of debate1.
BV prevalence varies geographically and ethnically, and can affect >50% of women in some countries6. BV is diagnosed using Amsel’s criteria or Nugent score, with Amsel’s criteria more commonly used in the clinic5. Amsel’s criteria combines inspection of vaginal secretions, pH measurement, visual inspection under microscopy, and the Whiff test, whereas the Nugent score focuses exclusively on scoring Gram-stained microscopy images. The BV definition based on DNA sequencing of vaginal secretions is referred to as molecular BV7,8.
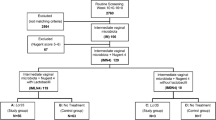
Recent studies have provided insights into the relationship between the vaginal microbiome environment and BV symptoms. In the Lactobacillus-dominated vaginal microbiome, various antimicrobial substances are produced, including lactic acid, bacteriocins, and hydrogen peroxide (H2O2), which play essential roles in protecting against potential pathogens9,10,11. Vaginal fluids are rich in glycogen, which is broken down into simpler carbohydrates by human alpha-amylase12,13. Lactobacillus species metabolize these carbohydrates, producing lactic acid and maintaining an acidic environment9,14. Bacteriocins, such as bacteriocins IIa, IIc, J46, acidocin lF221A, gassericin T, and type-A lantibiotic, produced by Lactobacillus species exhibit bactericidal activity10. Although H2O2 level has been linked to a healthy vaginal environment, its role in vaginal microbiome protection is still under investigation15,16. Furthermore, cervicovaginal secretions from women with L. crispatus-dominated vaginal microbiome show lower levels of genital inflammatory scores17,18 (Fig. 1). By contrast, vaginal fluids in BV are characterized by higher concentrations of short chain fatty acids (SCFAs), such as acetate, propionate, butyrate, and succinate, with vaginal pH elevated over 4.519,20. Also, catabolism of amino acids results in amines that are responsible for the fishy odor, and catabolism of mucosal proteins results in a thinner mucosal layer and the production of a thin homogenous discharge21. Elevated cytokine and chemokine levels in the vaginal tract have also been observed in women with BV22 (Fig. 1).
a Lactobacillus-dominated vaginal microbiome environment. Vaginal Lactobacillus species, such as Lactobacillus crispatus, produce lactic acid, bacteriocins, and hydrogen peroxide (H2O2), which may provide protection against bacterial vaginosis (BV) related bacteria and other infections. b BV microbiome environment. BV-related bacteria (mainly Gardnerella) induce inflammation in the vaginal tract and form a biofilm on vaginal epithelial cells. The latter probably increases antibiotic resistance and refractoriness to probiotic treatment. Short chain fatty acids (SCFAs) produced by BV-related bacteria, increase vaginal pH. In addition, catabolism of amino acids and mucosal proteins results in amines and a thinner mucosal layer in the vaginal tract. c Treatment of BV with probiotics. Pretreatment such as antibiotic, bacteriophage, anti-biofilm, or antimicrobial agents, in combination with vaginal probiotic species and vaginal administration, increase the probability of successful colonization. Note: figure was created with BioRender.com.
The standard of care treatment for BV is antibiotics. Live biopharmaceutical products, defined by the United States Food and Drug Administration (FDA) and the European Pharmacopeia as “a biological product that contains live organisms; is applicable to the prevention, treatment, or cure of a disease or condition of human beings; and is not a vaccine”, or generally called “probiotics,” defined as “live microorganisms that, when administered in adequate amounts, confer a health benefit on the host” by the Food and Agriculture Organization of the United Nations and the World Health Organization and revised by the International Scientific Association for Probiotics and Prebiotics, have been evaluated as BV treatments in clinical trials for decades with mixed results. Recently, vaginal microbiome transplantation (VMT), the process of transferring the microbiome of a healthy donor to an individual as a therapeutic alternative, has been tested to restore the vaginal microbiome. In this review, we discuss the advantages and disadvantages of these interventions and provide our considerations of what needs to be contemplated for future clinical trials with probiotics.
Advantages and limitations of current methods used for treating BV
Antibiotics
Antibiotics are widely used for BV treatment and have an effective initial cure rate varying between 80% and 90% 1 month after treatment1,23,24. The recommended antibiotics for BV and recurrent BV are metronidazole and clindamycin in the clinic1,25, which can be administered orally or intravaginally1,24. These recommended regimens have similar efficacy for BV treatment, with minor differences in recurrence rates26,27. Other tested antibiotics include tinidazole and secnidazole, which have similar activity in vitro against a range of microorganisms associated with BV28.
Recurrent BV is a common problem associated with the treatment of BV and presents as repeated cases of BV after the initial cessation of symptoms. Available research suggests that recurrent BV may be caused by a relapse of infection due to an inability to reestablish a Lactobacillus-dominated vaginal microbiome or the ineffective suppression of BV-related bacteria1. Recurrence of BV can also indicate persistent BV, where a positive BV diagnosis remains unchanged after treatment29,30. A high rate of BV recurrence after 1 year has been observed, ranging from 50% to 100% depending on the antibiotic used and geographic locations, underscoring the need for additional treatments1,23,30. Other factors that could affect the vaginal microbiome and potentially the efficiency of BV treatment include age (before puberty or after menopause), pregnancy, sexual intercourse, and other diseases or medical conditions31,32.
The advantages of treatment with antibiotics are their availability and convenience for clinical use. Patients can easily administer antibiotics at home with instruction. Also, since BV is characterized by the overgrowth of anaerobic bacteria, reduced vaginal bacterial load following antibiotic treatment may provide the chance for Lactobacillus species to compete for nutrients and biological niches again. Overall, a large proportion of women with BV have been cured after one-time treatment in a short period of time27,33,34.
However, the main issue with using antibiotic treatment for BV is the high rate of recurrence within months of treatment23. Relapse may occur when vaginosis-related bacteria re-colonize and take over the vaginal microbiome. Furthermore, vaginosis-related bacteria that recur after antibiotic treatment, such as Gardnerella vaginalis and Atopobium vaginae, may have higher resistance and become less sensitive to another round of antibiotic treatment29,30,35. Also, orally administered metronidazole and clindamycin disturb the healthy gut microbiome36,37, whereas even local usage of antibiotics is a risk factor for vulvovaginal candidiasis38,39.
Thus, it is important to follow the dynamics of the vaginal microbiome for at least 6 months following treatment to assess complete clinical cure endpoints23. Moreover, restoring the vaginal microbiome after antibiotic treatment (e.g., with probiotics or VMT) will assist the recovery of the vaginal environment and complete the whole treatment procedure (Fig. 1). Therefore, evaluation of additional methods for BV treatment and prevention, especially recurrent BV, will be of great value in the clinic.
Probiotics
With sequencing information obtained by the human microbiome project and many other vaginal microbiome investigations, we have learned that a large proportion of women without gynecological symptoms have a vaginal microbiome dominated by either L. crispatus or L. iners2,3,4. While an L. crispatus-dominated vaginal microbiome is related to a healthy vaginal condition, L. iners-dominated and specially non-Lactobacillus-dominated vaginal microbiomes are linked to a higher risk for infections, such as human papillomavirus and Chlamydia trachomatis1,2.
Using a single strain or mixtures of Lactobacillus strains, especially vaginal L. crispatus, could have many benefits. It avoids the risk of introducing other vaginal bacteria related to vaginosis or infections, such as G. vaginalis and Prevotella species. Once the Lactobacillus strains colonize, the produced lactic acid and bacteriocins could lower vaginal pH, inhibit BV-related pathogens, and potentially prevent BV recurrence in the long term9,10,11,14. It is easier to culture single bacterial strains in large batches under controlled standard conditions. It is also cheaper for clinical use and prevents the possibility of transferring cells and untested organisms from donor women, as in VMT.
On the other hand, probiotics only contain bacterial strains without other potential beneficial factors, such as bacteriophages or molecules that assist in the growth and colonization of Lactobacillus species. The colonization by Lactobacillus strains could be influenced by many factors including resident vaginal bacteria, glycogen, and lactic acid concentration, sexual intercourse, hormonal changes, and bleeding40,41,42. Moreover, the main concern for a single Lactobacillus strain is whether one strain would fit all genetic and immunological backgrounds, given a large variation of L. crispatus genomes in the vaginal microbiome43,44. If a mixture of strains should apply, it is still unclear which strains should be selected, and whether all mixtures will fit and colonize in women regardless of the geographic and ethnic background. If different Lactobacillus strains compete in the vaginal tract and further hinder their colonization or function, more strains would not necessarily have a stronger effect than a single strain. Finally, when mixed strains are used, each Lactobacillus strain needs to pass the standard of federal agency, which is a larger challenge than a single strain. Like VMT, the use of probiotics also lacks uniform and effective policy supervision. The lack of a standardized manufacturing process focused on the effectiveness and safety of probiotics, including the proper species, dose, administration method, presence of contaminating microorganisms, and auxiliary ingredients of probiotics, adds to uncertainty around the results for probiotics45.
Potential factors that influence the effect of Lactobacillus as a probiotic treatment
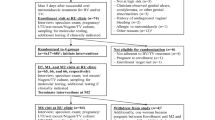
Many attempts to treat BV with probiotics have been made, but with mixed results. Considering that Lactobacillus is the main genus identified in the vagina and is also the most commonly used probiotic in BV treatment, we reviewed the literature and clinical trial registrations and proposed the following three main considerations.
Consideration 1: species variation
The first and most important issue is the Lactobacillus species that have been used in clinical trials. While probiotic attempts have focused on the genus Lactobacillus, species within a genus are not interchangeable43. Notably, vaginal Lactobacillus species are different from gut Lactobacillus, and their functional repertoire and ideal growing conditions markedly differ43,44. Species-specific characteristics may affect bacterial colonization or the microenvironment for bacteria–bacteria and bacteria–host interactions. Among the common Lactobacillus species that dominate the vaginal microbiome, L. crispatus-dominated vaginal microbiome demonstrate high stability, whereas L. gasseri and/or L. iners are more conducive to the incidence of abnormal vaginal microbiome in longitudinal analysis46. Moreover, even within the same species, different L. crispatus strains from a vaginal tract or intestinal tract demonstrate phenotypic variations that allow the bacteria to adapt to the different environments47,48. Furthermore, several recent studies have also indicated that different strains of vaginal L. crispatus demonstrate significant differences in genes for glycosylation and glycogen degradation, as well as antimicrobial and inflammatory properties, which may affect the colonization efficiency of L. crispatus and also the treatment effect on BV49,50.
Surprisingly, through extensive literature search, we found only a few BV probiotic trials regarding L. crispatus. Almost all of the clinical trials for BV treatment used Lactobacillus species from the gastrointestinal tract, probably due to how recently sequencing studies revealed that the Lactobacillus species dominating the vaginal microbiome are different from gut Lactobacillus (Tables 1–4). One L. crispatus clinical trial showed promising results for BV, with an 80% remission rate compared with a 59% remission rate in the placebo group51. This result is comparable to VMT treatment (80% vs. 80% cure rate based on clinical diagnosis), which suggests that one strain of L. crispatus may be as effective as VMT. Furthermore, two well-designed, double-blinded clinical trials with L. crispatus CTV-05 (LACTIN-V), administered to the vaginal tract directly after metronidazole treatment, showed a significantly decreased recurrence of bacterial vaginosis and increased L. crispatus colonization52,53. In the limited clinical studies described above, L. crispatus treatment resulted in a cure rate of 100% when considered short term and cure rates of 70% and 79.5% based on clinical Amsel’s criteria when considering long-term effects51,53,54.
Other Lactobacillus clinical trials mainly chose Lactobacillus species found in the gastrointestinal tract, most commonly L. rhamnosus GR-1 and L. reuteri RC-14, which yielded a cure rate of between 51% and 88% when considered short term (<4 months)55,56,57,58 (Tables 1 and 3) and between 20% and 42% when considered long term (≥4 months)59,60 (Tables 2 and 4). Improper Lactobacillus species may partly explain why the cure rate varies from study to study and why the bacteria do not colonize the vaginal tract. Notably, L. crispatus is strongly associated with a reduced risk of BV compared with other Lactobacillus species (Tables 3 and 4). Interestingly, even the placebo branch of the clinical trials showed a large range of cure rates (0–73%; Table 1), suggesting the complicated dynamics of BV and its treatment. Another possible reason might be the subjectivity of the diagnostic methods, which used wet mounts and Gram staining. A more accurate evaluation of treatment effects, such as sequencing, should be considered in future clinical trials7,8. In addition to L. crispatus CTV-05 (LACTIN-V), several other L. crispatus clinical trials aimed at preventing recurrent urinary tract infection also demonstrated safe and efficient use in the vaginal tract61,62,63.
To summarize, most of the current BV clinical trials did not use Lactobacillus species from the vaginal tract. These data collectively indicate that L. crispatus could be of potential use for BV treatment and that a rigorous pre-clinical screening strategy needs to be applied to identify the best strains that can maximize adaptiveness and colonization in the vaginal environment. The proper Lactobacillus species from a vaginal microbiome should also be tested in large, randomized, placebo-controlled cohorts.
Consideration 2: administration method
The second important factor that we believe contributes to the inefficient cure rate in clinical trials is the mode of probiotic administration. Although there is evidence that the gut microbiome might influence the vaginal environment, oral intake of bacteria for vaginosis treatment is probably based on the immune response or circulating metabolites that lack direct bacteria–bacteria inhibition64. Oral administration of probiotics follows the regulation of food supplements instead of drug development, which is less strict and provides a faster track to the market. The ability of probiotic strains to survive passage through the gastrointestinal tract becomes an important selection criterion when oral administration is intended54,59,65,66. Hypothetically, vaginal administration allows for the direct replacement of BV-related microbes by probiotic strains. Once these strains have colonized, the replacement consequently results in the maintenance of a low pH and the production of lactic acid and antimicrobial substances, which could further support a healthy vaginal microbiome environment on site16. Direct vaginal application also showed a slightly higher cure rate compared to the same L. rhamnosus GR-1 and L. reuteri RC-14 strains administered orally (88% vs. 51%; Table 1)55,56.
Consideration 3: pretreatment
Finally, the vaginal microenvironment is altered by BV-related bacteria, which could increase the difficulty for probiotic strains to compete with BV-related bacteria and hinder the colonization of probiotic strains52. Thus, it may be necessary to open a niche for probiotic strains to minimize colonization resistance from resident bacteria, especially overgrown biofilm-forming bacteria. Combinations of antibiotics and probiotic treatments have been previously attempted. A study indicated that the combination of probiotics and metronidazole is more effective than antibiotics alone in maintaining a healthy vaginal ecosystem67. There is also an overall higher remission rate with clinical trials with combined probiotic and antibiotic treatment (42–83%) compared to those using probiotics alone (20–48%) in long-term studies (≥4 months) (Table 4 vs. Table 2). For instance, short-term studies (<4 months) on L. rhamnosus GR-1 and L. reuteri RC-14 showed an 88% cure rate with antibiotic pretreatment compared to 51–88% in L. rhamnosus GR-1 and L. reuteri RC-14 only without antibiotic pretreatment (Tables 1 and 3)55,56,58. Moreover, long-term studies (≥4 months) on L. rhamnosus GR-1 and L. reuteri RC-14 showed a 42% cure rate with antibiotic pretreatment compared to 20% on L. rhamnosus GR-1 and L. reuteri RC-14 only without antibiotic pretreatment59,60 (Tables 2 and 4). Given that orally administered antibiotics influence the whole gut microbiome36,37, we propose larger randomized cohort studies with L. crispatus delivered directly to the vagina after pretreatment with antibiotics administered vaginally that reduce the influence of BV-related bacteria (Fig. 1).
VMT
VMT uses a similar approach as fecal microbiome transplant (FMT) which has greatly developed in the past decade in the field of gastroenterology, most prominently to treat recurring Clostridioides difficile infections12. VMT is the process of obtaining vaginal fluid from a donor and administer it into the vagina of a recipient, after thorough testing and minimal processing with the goal of maintaining the viability of the bacteria68. The mixture of fluid not only includes the microbes from the donor but also potentially cells, bacteriophages, proteins such as cytokines, and metabolites such as lipids and antimicrobial peptides. Recently, a study recruited five patients suffering from recurrent BV and introduced treatment with VMT after an antibiotic regimen69,70. Four of five patients had long-term remission after VMT, making it a promising alternative treatment for recurrent BV. Further studies including large, randomized, placebo controlled clinical trials are needed to follow up on VMT. Notably, of the five women included in the VMT study, four became colonized by L. crispatus with a full cure and were symptom-free up to 11 months, although three of the women required three rounds of VMT before achieving sustained remission. A fifth woman was colonized by L. gasseri and had only a partial cure based on clinical criteria. The feasibility of transplanting the vaginal microbiome between women and its protection against BV development is further supported by increasing evidence from women who have sex with women. The interchange of the vaginal microbiome during sex leads to a high level of concordance for a stable vaginal microbiome and a low risk of BV69,71.
Overall, VMT presents a promising way to combine antibiotic treatment and restoration of the vaginal microbiome to combat vaginosis-related bacteria. It also provides a whole environment, including the mixture of vaginal microbes and molecules produced by both hosts and microbes (e.g., lactic acid, cytokines, bacteriocins, and antimicrobial peptides), which assists in the colonization of essential bacteria while working against BV-associated bacteria9,11,14. These molecules might be essential for the successful re-establishment of a healthy vaginal microbiome.
However, the main functional compounds of VMT have yet to be identified. Further, similar to FMT, attention has been drawn to potential risks including heterogeneity across donors and the transmission of infectious agents and metabolites outside the standard set of tests72,73. Also, due to the lack of a standardized manufacturing process in terms of the definition of microorganisms, dose, functional properties, antibiotic resistance profiling, and potential presence of pathogens or contaminating microorganisms, it is still challenging to overcome these obstacles and pass the standard from federal agencies such as FDA. Other ethical issues, including the ethnicity and socioeconomic status of women, also need to be considered before VMT. The FDA issued a special guidance for FMT and recently drafted a guidance for developing drugs for BV treatment74. However, since BV recurrence is not as deadly as C. difficile infections, whether VMT benefits outweigh risks remains an open question. Moreover, VMT is still in its infancy, lacking large clinical trial data, and whether VMT provides a better clinical cure rate than defined probiotics and/or prebiotics needs further investigation. Further medical and regulatory needs for the clinical and regulatory viability of VMT include standardized procedures for donor screening, laboratory tests to exclude potential risk of infection, standardized sample preparation and administration procedures, standardized protocols for follow-up of donors and recipients, and maintenance of records in a biobank as currently proposed for FMT69,75,76.
Other possibilities
Other possibilities that could replace antibiotics as vaginosis treatment or pretreatment should also be evaluated. Isolating bacteriophages is a well-established technology, and bacteriophages targeting BV-related bacteria can be used alone or in combination with probiotics77. Previous studies have identified that Lactobacillus bacteriophages are related to BV, and a higher load of Lactobacillus bacteriophages was found in vaginal microbiome samples among women with BV compared to healthy women78,79. However, although there have been bacteriophages against Gardnerella and Clostridium reported by sequencing, no lytic bacteriophage has been isolated by culturing80. Furthermore, bacteriophages targeting Prevotella have been reported in the gut, but whether bacteriophages targeting vaginal Prevotella and other BV-related bacteria exist should be further studied80.
One aspect of the high rate of BV recurrence after therapy could be due to biofilm persistence81. Biofilm formation enhances the endurance of BV-related bacteria against antibacterial regimens from beneficial vaginal microbes or antibiotic treatment82. G. vaginalis is considered to be the key player in biofilm formation by adhering to the surface of vaginal epithelial cells and allowing the attachment of other species, thus leading to the formation of “clue cells,” which have been used in the clinical diagnosis of BV83,84. Bioproducts, such as anti-biofilm or antimicrobial peptides that inhibit BV-associated bacterial growth and biofilm formation, could be a future replacement for antibiotic treatment to achieve higher precision and fewer side effects31,85,86. Biofilm-disrupting agents, such as intravaginal boric acid enhanced with ethylenediaminetetraacetic acid (TOL-463) and amphoteric tenside (WO3191), are being investigated to determine their role in BV treatment (NCT03930745, NCT02687789)87,88. Another biofilm-disrupting agent example is a pHyph, a vaginal pessary containing glucono-delta-lactone and sodium gluconate. In a recent study, it was shown that pHyph has the potential to restore a normal pH and resolve clinical BV symptoms89.
Lactobacillus monoisolate or mixtures of healthy vaginal bacterial strains, with combinations of beneficial molecules, could be additional options for treatment72. Another promising approach currently in clinical trial is the Flourish Vaginal Care System (ClinicalTrials.gov, Identifier: NCT03734523)90, which includes bio-matched vaginal secretions of women with L. crispatus-dominated microbiome, a probiotic combination of L. crispatus and other strains, and a gentle, pH-balancing cleanser. All of these methods including a probiotic mix, prebiotic combinations, and/or bacteriophages provide more controlled conditions, convenience for clinical application, and ease of commercialization compared to VMT.
Challenges/opportunity of treating BV using novel interventions including probiotics and VMT
The golden age for restoring the vaginal microbiome to decrease BV and its recurrence has begun. However, except for the disadvantages discussed above, several other challenges need to be considered. Foremost, unlike regular drugs, VMT and probiotics lack a standardized manufacturing process, which could affect microbial survival, growth, and viability45,91,92. A standardized procedure for producing VMT and probiotics should be established and tested. Manufacturing the whole vaginal microbiome consistently and stably in vitro will contribute to the development and approval processes for the clinical use of VMT. Also, the effects of probiotics are strain-specific and dose-dependent; hence, medical-grade probiotics require certified laboratories universally shared validated and standardized methodologies for production and quality-control45.
Second, suitable regulatory aspects related to the production and marketing of VMT and vaginal probiotics should be in place. Vaginal administration leads to products not classified as dietary supplements. Being classified into personal care products or being prescribed to patients as drugs needs more restrictive regulation and report adverse events91,93. In this regard, professional medical associations should issue recommendations concerning the role of VMT and probiotics in obstetrics and gynecology, as their uncontrolled implementation might also lead to a potential decrease in effectiveness. Detailed discussions on medical and regulatory considerations, including finding the right FDA regulatory path for VMT, are of crucial importance for future clinical trials of VMT and have been reviewed in other papers69,94.
Finally, further high-quality data are needed to define the microbiome/strains and their effective dose in different obstetrical and gynecological conditions. Furthermore, more research needs to be focused on the interactions between vaginal microbes95, including pathogens and potential probiotics96, as well as between host and microbes84. In this manner, suitable probiotics can be selected for patients with different disease conditions or other background characteristics. Finally, vaginal microbe biobanks, such as biobanks of different L. crispatus strains, should be built, sequenced, and well documented so that more probiotics or probiotic cocktails can be selected and tested50,92.
Conclusion
In summary, we provide an overview of current treatments and interventions for BV, and discuss their advantages and limitations. We propose possible reasons why some recent clinical trials using probiotics did not work as efficiently as expected. We believe the current high recurrence rate of BV is mainly due to the application of microbial species that do not originate from the vagina, an oral instead of vaginal administration method, and a lack of probiotic replacement after antibiotic treatment. We believe there is a great opportunity to use vaginal Lactobacillus species such as L. crispatus, instead of gut Lactobacillus species as in earlier clinical trials, administered directly into the genital tract in combination with pretreatments such as vaginal antibiotic treatment, anti-biofilm, or antimicrobial agents for BV treatment (Fig. 1). There is a great need for large, placebo controlled, double blind clinical trials and mechanism-based research to determine the safety and efficacy of these novel interventions. The dynamic and complex vaginal microbiome creates obstacles for clinical trials, and the considerations discussed here should help accelerate the successful development of clinical trials against BV.
Data availability
All data generated in this study are included in this published article.
References
Coudray, M. S. & Madhivanan, P. Bacterial vaginosis—a brief synopsis of the literature. Eur. J. Obstet. Gynecol. Reprod. Biol. 245, 143–148 (2020).
Cheng, L. et al. Vaginal microbiota and human papillomavirus infection among young Swedish women. npj Biofilms Microbiomes 6, 39 (2020).
Serrano, M. G. et al. Racioethnic diversity in the dynamics of the vaginal microbiome during pregnancy. Nat. Med. 25, 1001–1011 (2019).
Ravel, J. et al. Vaginal microbiome of reproductive-age women. Proc. Natl. Acad. Sci. USA 108, 4680–4687 (2011).
Donders, G. Diagnosis and management of bacterial vaginosis and other types of abnormal vaginal bacterial flora: a review. Obstet. Gynecol. Surv. 65, 462–473 (2010).
Kenyon, C., Colebunders, R. & Crucitti, T. The global epidemiology of bacterial vaginosis: a systematic review. Am. J. Obstet. Gynecol. 209, 505–523 (2013).
Fredricks, D. N., Fiedler, T. L. & Marrazzo, J. M. Molecular identification of bacteria associated with bacterial vaginosis. N. Engl. J. Med. 353, 1899–1911 (2005).
Coleman, J. S. & Gaydos, C. A. Molecular diagnosis of bacterial vaginosis: an update. J. Clin. Microbiol. 56, e00342–18 (2018).
O’Hanlon, D. E., Moench, T. R. & Cone, R. A. Vaginal pH and microbicidal lactic acid when lactobacilli dominate the microbiota. PLoS One 8, e80074 (2013).
Stoyancheva, G., Marzotto, M., Dellaglio, F. & Torriani, S. Bacteriocin production and gene sequencing analysis from vaginal lactobacillus strains. Arch. Microbiol. 196, 645–653 (2014).
Vallor, A. C., Antonio, M. A., Hawes, S. E. & Hillier, S. L. Factors associated with acquisition of, or persistent colonization by, vaginal lactobacilli: role of hydrogen peroxide production. J. Infect. Dis. 184, 1431–1436 (2001).
Drekonja, D. et al. Fecal microbiota transplantation for clostridium difficile infection: a systematic review. Ann. Intern. Med. 162, 630 (2015).
Spear, G. T. et al. Human α-amylase present in lower-genital-tract mucosal fluid processes glycogen to support vaginal colonization by lactobacillus. J. Infect. Dis. 210, 1019–1028 (2014).
Kalia, N., Singh, J. & Kaur, M. Microbiota in vaginal health and pathogenesis of recurrent vulvovaginal infections: a critical review. Ann. Clin. Microbiol. Antimicrob. 19, 5 (2020).
Tachedjian, G., O’Hanlon, D. E. & Ravel, J. The implausible ‘in vivo’ role of hydrogen peroxide as an antimicrobial factor produced by vaginal microbiota. Microbiome 6, 29 (2018).
O’Hanlon, D. E., Moench, T. R. & Cone, R. A. In vaginal fluid, bacteria associated with bacterial vaginosis can be suppressed with lactic acid but not hydrogen peroxide. BMC Infect. Dis. 11, 200 (2011).
Masson, L. et al. Inflammatory cytokine biomarkers of asymptomatic sexually transmitted infections and vaginal dysbiosis: a multicentre validation study. Sex. Transm. Infect. 95, 5–12 (2019).
Łaniewski, P. et al. Features of the cervicovaginal microenvironment drive cancer biomarker signatures in patients across cervical carcinogenesis. Sci. Rep. 9, 7333 (2019).
Delgado-Diaz, D. J. et al. Distinct immune responses elicited from cervicovaginal epithelial cells by lactic acid and short chain fatty acids associated with optimal and non-optimal vaginal microbiota. Front. Cell Infect. Microbiol. 9, 446 (2019).
Aldunate, M. et al. Antimicrobial and immune modulatory effects of lactic acid and short chain fatty acids produced by vaginal microbiota associated with eubiosis and bacterial vaginosis. Front. Physiol. 6, 164 (2015).
Srinivasan, S. et al. Metabolic signatures of bacterial vaginosis. mBio 6, e00204–e00215 (2015).
Hedges, S. R., Barrientes, F., Desmond, R. A. & Schwebke, J. R. Local and systemic cytokine levels in relation to changes in vaginal flora. J. Infect. Dis. 193, 556–562 (2006).
Bradshaw, C. S. et al. High recurrence rates of bacterial vaginosis over the course of 12 months after oral metronidazole therapy and factors associated with recurrence. J. Infect. Dis. 193, 1478–1486 (2006).
Joesoef, M. R., Schmid, G. P. & Hillier, S. L. Bacterial vaginosis: review of treatment options and potential clinical indications for therapy. Clin. Infect. Dis. 28, S57–S65 (1999).
Bradshaw, C. S. & Sobel, J. D. Current treatment of bacterial vaginosis—limitations and need for innovation. J. Infect. Dis. 214, S14–S20 (2016).
Austin, M. N., Beigi, R. H., Meyn, L. A. & Hillier, S. L. Microbiologic response to treatment of bacterial vaginosis with topical clindamycin or metronidazole. J. Clin. Microbiol 43, 4492–4497 (2005).
Ferris, D. G., Litaker, M. S., Woodward, L., Mathis, D. & Hendrich, J. Treatment of bacterial vaginosis: a comparison of oral metronidazole, metronidazole vaginal gel, and clindamycin vaginal cream. J. Fam. Pract. 41, 443–450 (1995).
Petrina, M. A. B., Cosentino, L. A., Rabe, L. K. & Hillier, S. L. Susceptibility of bacterial vaginosis (BV)-associated bacteria to secnidazole compared to metronidazole, tinidazole and clindamycin. Anaerobe 47, 115–119 (2017).
Schuyler, J. A. et al. Identification of intrinsically metronidazole-resistant clades of Gardnerella vaginalis. Diagn. Microbiol. Infect. Dis. 84, 1–3 (2016).
Faught, B. M. & Reyes, S. Characterization and treatment of recurrent bacterial vaginosis. J. Women’s Health 28, 1218–1226 (2019).
Cs, B. & Rm, B. Making inroads into improving treatment of bacterial vaginosis—striving for long-term cure. BMC Infect. Dis. 15, 292 (2015).
Auriemma, R. S. et al. The vaginal microbiome: a long urogenital colonization throughout woman life. Front. Cell Infect. Microbiol. 11, 686167 (2021).
Oyinlola, O. O., Rose, I. A. & Folasade, T. O. The effects of antimicrobial therapy on bacterial vaginosis in non-pregnant women. Cochrane Database Syst. Rev. 8, CD006055 (2009).
Hans, V. & Rita, V. Bacterial vaginosis: an update on diagnosis and treatment. Expert Rev. Anti Infect. Ther. 7, 1109–1124 (2009).
Ferris, M. J. et al. Association of Atopobium vaginae, a recently described metronidazole resistant anaerobe, with bacterial vaginosis. BMC Infect. Dis. 4, 5 (2004).
Zimmermann, P. & Curtis, N. The effect of antibiotics on the composition of the intestinal microbiota—a systematic review. J. Infect. 79, 471–489 (2019).
Pilla, R. et al. Effects of metronidazole on the fecal microbiome and metabolome in healthy dogs. J. Vet. Intern. Med. 34, 1853–1866 (2020).
Shukla, A. & Sobel, J. D. Vulvovaginitis caused by candida species following antibiotic exposure. Curr. Infect. Dis. Rep. 21, 44 (2019).
Jacob, L., John, M., Kalder, M. & Kostev, K. Prevalence of vulvovaginal candidiasis in gynecological practices in Germany: a retrospective study of 954,186 patients. Curr. Med. Mycol. 4, 6–11 (2018).
Antonio, M. A. D., Meyn, L. A., Murray, P. J., Busse, B. & Hillier, S. L. Vaginal colonization by probiotic Lactobacillus crispatus CTV-05 is decreased by sexual activity and endogenous Lactobacilli. J. Infect. Dis. 199, 1506–1513 (2009).
Mirmonsef, P. et al. Free glycogen in vaginal fluids is associated with Lactobacillus colonization and low vaginal pH. PLoS One 9, e102467 (2014).
Farage, M. A., Miller, K. W. & Sobel, J. D. Dynamics of the vaginal ecosystem—hormonal influences. Infect. Dis. (Auckl.) 3, IDRT.S3903 (2010).
Zhang, Q. et al. Comparative genomics of Lactobacillus crispatus from the gut and vagina reveals genetic diversity and lifestyle adaptation. Genes 11, 360 (2020).
Duar, R. M. et al. Lifestyles in transition: evolution and natural history of the genus Lactobacillus. FEMS Microbiol. Rev. 41, S27–S48 (2017).
Kolaček, S. et al. Commercial probiotic products: a call for improved quality control. A position paper by the ESPGHAN working group for probiotics and prebiotics. J. Pediatr. Gastroenterol. Nutr. 65, 117–124 (2017).
Verstraelen, H. et al. Longitudinal analysis of the vaginal microflora in pregnancy suggests that L. crispatus promotes the stability of the normal vaginal microflora and that L. gasseri and/or L. iners are more conducive to the occurrence of abnormal vaginal microflora. BMC Microbiol. 9, 116 (2009).
Pan, M., Hidalgo-Cantabrana, C., Goh, Y. J., Sanozky-Dawes, R. & Barrangou, R. Comparative analysis of Lactobacillus gasseri and Lactobacillus crispatus isolated from human urogenital and gastrointestinal tracts. Front. Microbiol. 10, 3146 (2020).
Mancabelli, L. et al. Comparative genome analyses of Lactobacillus crispatus isolates from different ecological niches reveal an adaptation of this species to the human vaginal environment. Appl. Environ. Microbiol. 87, e02899–20 (2021).
Chetwin, E. et al. Antimicrobial and inflammatory properties of South African clinical Lactobacillus isolates and vaginal probiotics. Sci. Rep. 9, 1917 (2019).
van der Veer, C. et al. Comparative genomics of human Lactobacillus crispatus isolates reveals genes for glycosylation and glycogen degradation: implications for in vivo dominance of the vaginal microbiota. Microbiome 7, 49 (2019).
Bohbot, J. M. et al. Efficacy and safety of vaginally administered lyophilized Lactobacillus crispatus IP 174178 in the prevention of bacterial vaginosis recurrence. J. Gynecol. Obstet. Hum. Reprod. 47, 81–86 (2018).
Ngugi, B. M. et al. Effects of BV-associated bacteria and sexual Intercourse on vaginal colonization with the probiotic Lactobacillus crispatus CTV-05. Sex. Transm. Dis. 38, 1020–1027 (2011).
Cohen, C. R. et al. Randomized trial of lactin-V to prevent recurrence of bacterial vaginosis. N. Engl. J. Med. 382, 1906–1915 (2020).
Laue, C. et al. Effect of a yoghurt drink containing Lactobacillus strains on bacterial vaginosis in women—a double-blind, randomised, controlled clinical pilot trial. Benef. Microbes 9, 35–50 (2018).
Vujic, G., Jajac Knez, A., Despot Stefanovic, V. & Kuzmic Vrbanovic, V. Efficacy of orally applied probiotic capsules for bacterial vaginosis and other vaginal infections: a double-blind, randomized, placebo-controlled study. Eur. J. Obstet. Gynecol. Reprod. Biol. 168, 75–79 (2013).
Anukam, K. C. et al. Clinical study comparing probiotic Lactobacillus GR-1 and RC-14 with metronidazole vaginal gel to treat symptomatic bacterial vaginosis. Microbes Infect. 8, 2772–2776 (2006).
Anukam, K. et al. Augmentation of antimicrobial metronidazole therapy of bacterial vaginosis with oral probiotic Lactobacillus rhamnosus GR-1 and Lactobacillus reuteri RC-14: randomized, double-blind, placebo controlled trial. Microbes Infect. 8, 1450–1454 (2006).
Martinez, R. C. R. et al. Improved cure of bacterial vaginosis with single dose of tinidazole (2 g), Lactobacillus rhamnosus GR-1, and Lactobacillus reuteri RC-14: a randomized, double-blind, placebo-controlled trial. Can. J. Microbiol. 55, 133–138 (2009).
Hummelen, R. et al. Lactobacillus rhamnosus GR-1 and L. reuteri RC-14 to prevent or cure bacterial vaginosis among women with HIV. Int J. Gynaecol. Obstet. 111, 245–248 (2010).
Bisanz, J. E. et al. A systems biology approach investigating the effect of probiotics on the vaginal microbiome and host responses in a double blind, placebo-controlled clinical trial of post-menopausal women. PLoS One 9, e104511 (2014).
Uehara, S. et al. A pilot study evaluating the safety and effectiveness of Lactobacillus vaginal suppositories in patients with recurrent urinary tract infection. Int J. Antimicrob. Agents 28, 30–34 (2006).
Stapleton, A. E. et al. Randomized, placebo-controlled phase 2 trial of a Lactobacillus crispatus probiotic given intravaginally for prevention of recurrent urinary tract infection. Clin. Infect. Dis. 52, 1212–1217 (2011).
Czaja, C. A., Stapleton, A. E., Yarova-Yarovaya, Y. & Stamm, W. E. Phase I trial of a Lactobacillus crispatus vaginal suppository for prevention of recurrent urinary tract infection in women. Infect. Dis. Obstet. Gynecol. 2007, e35387 (2007).
Reid, G. et al. Oral use of Lactobacillus rhamnosus GR-1 and L. fermentum RC-14 significantly alters vaginal flora: randomized, placebo-controlled trial in 64 healthy women. FEMS Immunol. Med. Microbiol. 35, 131–134 (2003).
Heczko, P. B. et al. Supplementation of standard antibiotic therapy with oral probiotics for bacterial vaginosis and aerobic vaginitis: a randomised, double-blind, placebo-controlled trial. BMC Women’s Health 15, 115 (2015).
Russo, R. & Karadja, E. & De Seta, F. Evidence-based mixture containing Lactobacillus strains and lactoferrin to prevent recurrent bacterial vaginosis: a double blind, placebo controlled, randomised clinical trial. Benef. Microbes 10, 19–26 (2019).
Özmen, Ş., Turhan, N. Ö. & Seçki̇n, N. C. Garnerella-associated vaginitis: comparison of three treatment modalities. Turk. J. Med. Sci. 28, 171–174 (1998).
Ma, D., Chen, Y. & Chen, T. Vaginal microbiota transplantation for the treatment of bacterial vaginosis: a conceptual analysis. FEMS Microbiol Lett. 366, fnz025 (2019).
DeLong, K., Zulfiqar, F., Hoffmann, D. E., Tarzian, A. J. & Ensign, L. M. Vaginal microbiota transplantation: the next frontier. J. Law Med. Ethics 47, 555–567 (2019).
Lev-Sagie, A. et al. Vaginal microbiome transplantation in women with intractable bacterial vaginosis. Nat. Med. 25, 1500–1504 (2019).
Vodstrcil, L. A. et al. Incident bacterial vaginosis (BV) in women who have sex with women is associated with behaviors that suggest sexual transmission of BV. Clin. Infect. Dis. 60, 1042–1053 (2015).
Blaser, M. J. Fecal microbiota transplantation for dysbiosis—predictable risks. N. Engl. J. Med. 381, 2064–2066 (2019).
United States Food and Drug Administration. Fecal microbiota for transplantation: safety alert—risk of serious adverse events likely due to transmission of pathogenic organisms. FDA. https://www.fda.gov/safety/medical-product-safety-information/fecal-microbiota-transplantation-safety-alert-risk-serious-adverse-events-likely-due-transmission (2020).
United States Food and Drug Administration. Bacterial vaginosis: developing drugs for treatment; draft guidance for industry; availability. FDA. https://www.regulations.gov/docket/FDA-2016-D-1659/document (2016).
Cammarota, G. et al. International consensus conference on stool banking for faecal microbiota transplantation in clinical practice. Gut 68, 2111–2121 (2019).
Kim, K. O. & Gluck, M. Fecal microbiota transplantation: an update on clinical practice. Clin. Endosc. 52, 137–143 (2019).
Gordillo Altamirano, F. L. & Barr, J. J. Phage therapy in the postantibiotic Era. Clin Microbiol Rev.s 32, e00066–18 (2019).
Damelin, L. H. et al. Identification of predominant culturable vaginal Lactobacillus species and associated bacteriophages from women with and without vaginal discharge syndrome in South Africa. J. Med Microbiol 60, 180–183 (2011).
Jakobsen, R. R. et al. Characterization of the vaginal DNA virome in health and dysbiosis. Viruses 12, 1143 (2020).
Devoto, A. E. et al. Megaphages infect Prevotella and variants are widespread in gut microbiomes. Nat. Microbiol 4, 693–700 (2019).
Muzny, C. A. & Schwebke, J. R. Biofilms: an underappreciated mechanism of treatment failure and recurrence in vaginal infections. Clin. Infect. Dis. 61, 601–606 (2015).
Van Acker, H., Van Dijck, P. & Coenye, T. Molecular mechanisms of antimicrobial tolerance and resistance in bacterial and fungal biofilms. Trends Microbiol 22, 326–333 (2014).
Muzny, C. A. et al. An updated conceptual model on the pathogenesis of bacterial vaginosis. J. Infect. Dis. 220, 1399–1405 (2019).
Muzny, C. A., Łaniewski, P., Schwebke, J. R. & Herbst-Kralovetz, M. M. Host-vaginal microbiota interactions in the pathogenesis of bacterial vaginosis. Curr. Opin. Infect. Dis. 33, 59–65 (2020).
Dover, S. E., Aroutcheva, A. A., Faro, S. & Chikindas, M. L. Natural antimicrobials and their role in vaginal health: a short review. Int J. Probiotics Prebiotics 3, 219–230 (2008).
Mishra, R. et al. Natural anti-biofilm agents: strategies to control biofilm-forming pathogens. Front. Microbiol. 11, 566325 (2020).
Marrazzo, J. M. et al. Safety and efficacy of a novel vaginal anti-infective, TOL-463, in the treatment of bacterial vaginosis and vulvovaginal candidiasis: a randomized, Single-blind, Phase 2, controlled trial. Clin. Infect. Dis. 68, 803–809 (2019).
Gottschick, C. et al. Treatment of biofilms in bacterial vaginosis by an amphoteric tenside pessary-clinical study and microbiota analysis. Microbiome 5, 119 (2017).
Latham-Cork, H. C. et al. A novel non-antimicrobial treatment of bacterial vaginosis: An open label two-private centre study. Eur. J. Obstet. Gynecol. Reprod. Biol. 256, 419–424 (2021).
Sexual Health and Wellness Institute. Clinical Trial to Survey Results of Flourish Vaginal Care System for Recurrent Bacterial Vaginosis. https://clinicaltrials.gov/ct2/show/NCT03734523 (2021).
Puebla-Barragan, S. & Reid, G. Probiotics in cosmetic and personal care products: trends and challenges. Molecules 26, 1249 (2021).
Ma, Y., Chen, H., Lan, C. & Ren, J. Help, hope and hype: ethical considerations of human microbiome research and applications. Protein Cell 9, 404–415 (2018).
Buggio, L., Somigliana, E., Borghi, A. & Vercellini, P. Probiotics and vaginal microecology: fact or fancy? BMC Women’s Health 19, 25 (2019).
Hoffmann, D. E., Palumbo, F. B., Ravel, J., Rowthorn, V. & von Rosenvinge, E. A proposed definition of microbiota transplantation for regulatory purposes. Gut Microbes 8, 208–213 (2017).
Herbst-Kralovetz, M. M., Pyles, R. B., Ratner, A. J., Sycuro, L. K. & Mitchell, C. New systems for studying intercellular interactions in bacterial vaginosis. J. Infect. Dis. 214, S6–S13 (2016).
Castro, J., Machado, D. & Cerca, N. Unveiling the role of Gardnerella vaginalis in polymicrobial bacterial vaginosis biofilms: the impact of other vaginal pathogens living as neighbors. ISME J. 13, 1306–1317 (2019).
Hantoushzadeh, S. et al. Comparative efficacy of probiotic yoghurt and clindamycin in treatment of bacterial vaginosis in pregnant women: a randomized clinical trial. J. Matern Fetal. Neonatal. Med. 25, 1021–1024 (2012).
Hallén, A., Jarstrand, C. & Påhlson, C. Treatment of bacterial vaginosis with lactobacilli. Sex. Transm. Dis. 19, 146–148 (1992).
Neri, A., Sabah, G. & Samra, Z. Bacterial vaginosis in pregnancy treated with yoghurt. Acta Obstet. Gynecol. Scand. 72, 17–19 (1993).
Parent, D. et al. Therapy of bacterial vaginosis using exogenously-applied Lactobacilli acidophili and a low dose of estriol: a placebo-controlled multicentric clinical trial. Arzneimittelforschung 46, 68–73 (1996).
Mastromarino, P. et al. Effectiveness of Lactobacillus-containing vaginal tablets in the treatment of symptomatic bacterial vaginosis. Clin. Microbiol Infect. 15, 67–74 (2009).
Ya, W., Reifer, C. & Miller, L. E. Efficacy of vaginal probiotic capsules for recurrent bacterial vaginosis: a double-blind, randomized, placebo-controlled study. Am. J. Obstet. Gynecol. 203, 120.e1–6 (2010).
Ling, Z. et al. The restoration of the vaginal microbiota after treatment for bacterial vaginosis with metronidazole or probiotics. Micro. Ecol. 65, 773–780 (2013).
Vicariotto, F., Mogna, L. & Del Piano, M. Effectiveness of the two microorganisms Lactobacillus fermentum LF15 and Lactobacillus plantarum LP01, formulated in slow-release vaginal tablets, in women affected by bacterial vaginosis: a pilot study. J. Clin. Gastroenterol. 48, S106 (2014).
Ehrström, S. et al. Lactic acid bacteria colonization and clinical outcome after probiotic supplementation in conventionally treated bacterial vaginosis and vulvovaginal candidiasis. Microbes Infect. 12, 691–699 (2010).
Eriksson, K., Carlsson, B., Forsum, U. & Larsson, P.-G. A double-blind treatment study of bacterial vaginosis with normal vaginal lactobacilli after an open treatment with vaginal clindamycin ovules. Acta Derm. Venereol. 85, 42–46 (2005).
Marcone, V., Calzolari, E. & Bertini, M. Effectiveness of vaginal administration of Lactobacillus rhamnosus following conventional metronidazole therapy: how to lower the rate of bacterial vaginosis recurrences. N. Microbiol 31, 429–433 (2008).
Petricevic, L. & Witt, A. The role of Lactobacillus casei rhamnosus Lcr35 in restoring the normal vaginal flora after antibiotic treatment of bacterial vaginosis. BJOG 115, 1369–1374 (2008).
Larsson, P.-G., Stray-Pedersen, B., Ryttig, K. R. & Larsen, S. Human lactobacilli as supplementation of clindamycin to patients with bacterial vaginosis reduce the recurrence rate; a 6-month, double-blind, randomized, placebo-controlled study. BMC Women’s Health 8, 3 (2008).
Marcone, V., Rocca, G., Lichtner, M. & Calzolari, E. Long-term vaginal administration of Lactobacillus rhamnosus as a complementary approach to management of bacterial vaginosis. Int J. Gynaecol. Obstet. 110, 223–226 (2010).
Bradshaw, C. S. et al. Efficacy of oral metronidazole with vaginal clindamycin or vaginal probiotic for bacterial vaginosis: randomised placebo-controlled double-blind trial. PLoS One 7, e34540 (2012).
Recine, N. et al. Restoring vaginal microbiota: biological control of bacterial vaginosis. A prospective case–control study using Lactobacillus rhamnosus BMX 54 as adjuvant treatment against bacterial vaginosis. Arch. Gynecol. Obstet. 293, 101–107 (2016).
Acknowledgements
We thank the Centre for Translational Microbiome Research (CTMR) and Karolinska Institutet for their support. CTMR is partly funded by Ferring Pharmaceuticals. J.D. and S.W. were supported by the Swedish Research Council (VR) (2021-01683), the Swedish Foundation for Strategic Research (ICA16-0050), Jeanssons Foundation (JS2017-0141, JS2018-0034), Clas Groschinskys Minnesfond (M18213, M19351), Svenska Läkaresällskapet (SLS-784981, SLS-960584), and the Karolinska Institute Foundation.
Funding
Open access funding provided by Karolinska Institute.
Author information
Authors and Affiliations
Contributions
Conception and design: J.D. Acquisition of data: S.W. Writing, review, and/or revision of the manuscript: S.W., L.W.H., I.S.-K., and J.D.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wu, S., Hugerth, L.W., Schuppe-Koistinen, I. et al. The right bug in the right place: opportunities for bacterial vaginosis treatment. npj Biofilms Microbiomes 8, 34 (2022). https://doi.org/10.1038/s41522-022-00295-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41522-022-00295-y
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.