Abstract
Despite the proven virological advantages, there remains some controversy regarding whether first-line integrase strand transfer inhibitors (INSTIs)-based antiretroviral therapy (ART) contributes to reducing mortality of people living with HIV (PLHIV) in clinical practice. Here we report a retrospective study comparing all-cause mortality among PLHIV in China who were on different initial ART regimens (nevirapine, efavirenz, dolutegravir, lopinavir, and others [including darunavir, raltegravie, elvitegravir and rilpivirine]) between 2017 and 2019. A total of 41,018 individuals were included across China, representing 21.3% of newly reported HIV/AIDS cases collectively in the country during this period. Only the differences in all-cause mortality of PLHIV between the efavirenz group and the nevirapine group, the dolutegravir group and the nevirapine group, and the lopinavir group and the nevirapine group, were observed in China. After stratifying the cause of mortality, we found that the differences in mortality between initial ART regimens were mainly observed in AIDS-related mortality.
Similar content being viewed by others
Introduction
Integrase strand transfer inhibitor (INSTI) has been introduced and widely recommended as the third drug in modern first-line treatment for people living with HIV (PLHIV) since its first approved in 20071,2. Previous studies have demonstrated its exceptional efficacy and safety3,4,5. However, not all countries are capable of timely promoting the use of INSTIs due to varying levels of development, economic status, and healthcare.
In China, the National Free Antiretroviral Treatment Program (NFATP) was launched in 2002 and has resulted in a significantly reduction in mortality rates for PLHIV6,7,8,9,10. In June 2016, China implemented a treat-all policy, which grants access for all PLHIV to antiretroviral therapy (ART) regardless of CD4+ T-cell count11. Before 2009, the ART regimens recommended were zidovudine (AZT) or stavudine + lamivudine (3TC) + nevirapine (NVP) or efavirenz (EFV)12. The Chinese Guidelines for Diagnosis and Treatment of HIV/AIDS 2011 incorporated the tenofovir-based ART regimens recommended by the WHO for resource-limited settings, consisting of a combination of tenofovir disproxil fumarate (TDF) + 3TC + EFV, which was also made available through the NFATP12,13. Over the past years, the NFATP-sponsored ART regimens have undergone continuous evaluation and improvement14. INSTIs, new generations of protease inhibitors (PIs), among others were introduced and promoted nationally, which substantially expanding access to ART initiation and switching for PLHIV in China14. Since 2015, raltegravir (RAL) and dolutegravir (DTG) have been used in PLHIV in China15,16,17,18. In 2018, single-regimen pills containing emtricitabine (FTC)/tenofovir alafenamide fumarate (TAF) and INSTI gained widespread useage15,16,17,18.
However, a recent real-world study from high-income countries found little evidence of differences in mortality rates between most modern first-line regimens19. In routine clinical care, decisions could be influenced by more factors than in a randomized trial, including side effects, adherence, and regimen tolerability, among others. For example, several studies have reported side effects of INSTI, including weight gain20,21, obesity22,23 and cardiovascular disease24 of PLHIV.
Evidence from low- and middle-income countries (LMICs) in routine clinical care would provide a clearer picture, as regimens commonly used in high-income countries are difficult to access or afford in resource-limited settings. Nonnucleoside reverse-transcriptase (NNRTI)- and PI-based ART regimens were used the most commonly in LMICs25,26. It has been reported in some LMICs that the majority of PLHIV on ART receive an NNRTI-based ART regimen, while those who meet a failure with NNRTI-based regimens are mostly switched to a PI-based regimen25,26. Moreover, long-term INSTI-based prescriptions are expensive in China. In 2015, two INSTIs received regulatory approval and began to be used in PLHIV in China15,16,17,18. However, the landscape of fully reimbursed ART in China before 2021 included two NNRTIs (EFV and NVP), and a single PI (lopinavir [LPV]); along with several nucleotide reverse transcriptase inhibitors (NRTIs). All INSTIs and most PIs were not available free of charge before 202114. Elucidating the effects on mortality of different ART regimens in practice is therefore crucial to the global ambition of achieving the UNAIDS 95-95-95 targets by 2030. In this study, we conducted a retrospective multicentre cohort study to provide evidence for decision-making in routine clinical care in resource-limited settings.
Results
A total of 41,018 individuals who started ART between January 2017 and September 2019 were included in the analyses. Overall, males accounted for 84.6% of the total sample, and the median age was 37 years (interquartile range [IQR] 28–52). 36,838 (89.8%) patients initiated NNRTI-based regimen, 1574 (3.8%) initiated INSTI-based regimen, and 2606 (6.4%) initiated PI-based regimen. 2777 (6.8%) switched regimen, 1132 (2.8%) loss to follow-up (LTFU), 14,366 (39.5%) achieved a CD4 > 500 from the 36,396 patients with initial CD4 < 500, and 656 (1.6%; 393 AIDS-related death and 263 non-AIDS-related death) died during 65,578 person-years of follow-up (median 1.6 years [IQR 1.0–2.2]). In the analysis of cumulative incidence for CD4 improvement, only 36,396 individuals with initial CD4 < 500 were included. Detailed characteristics of individuals included were presented in Table 1.
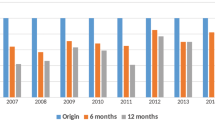
The proportion of PLHIV who started ART with EFV-based ART regimen decreased from 2017 to 2019, whereas the proportion with DTG increased in the same period (Fig. 1A). Specifically, 15,196 (87.4%) patients initiated EFV and 212 (1.2%) initial DTG as the third drugs in their regimen in 2017, but this changed to 6211 (81.2%) and 498 (6.5%) in 2019. In addition, the proportion of PLHIV who initiated ART with others uncommon drugs (including darunavir [DRV], RAL, elvitegravir [EVG] and rilpivirine [RPV]) as the third drugs increased from 132 (0.8%) in 2017 to 300 (3.9%) in 2019. The proportion of PLHIV deaths by initial ART regimen from 2017 to 2019 were shown in Fig. 1B.
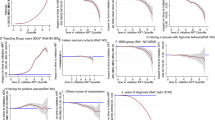
There were different risks of incidence for ART switch, LTFU, CD4 improvement, and death (Fig. 2). In the univariate Poisson regression model, compared to patients who initiated NVP based ART regimen, patients who initiated EFV (incidence rate ratio [IRR] 0.45, 0.32–0.62; Table S1) and LPV (0.57, 0.41-0.79) based ART regimens had significantly lower rates of incidence of ART switch, while patients who initiated DTG (2.07, 1.56–2.75) and others (2.62, 1.91–3.59) based ART regimens had significantly higher rates of incidence of ART switch. There was no significant difference in the incidence rate of LTFU between initial ART regimens. Compared to patients who initiated NVP based ART regimen, patients who initiated EFV (1.46, 1.21–1.76), DTG (1.96, 1.58–2.42), LPV (1.72, 1.42–2.08) and others (1.77, 1.39–2.26) based ART regimens had significantly higher rates of incidence of CD4 improvement; patients who initiated EFV (0.44, 0.22–0.85), DTG (0.23, 0.07–0.74), and LPV (0.23, 0.09–0.55) based ART regimens had significantly lower rates of incidence of all-cause mortality. Results for different causes of death were shown in Table S1.
Kaplan-Meier estimates of the cumulative incidence of ART switch, LTFU, CD4 improvement, all-cause mortality, AIDS-related mortality, and non-AIDS related mortality. ART antiretroviral therapy, LTFU loss to follow-up, CD4 improvement= transition of people living with HIV from CD4 < 500 cells/μL to CD4 > 500 cells/μL, NVP nevirapine, EFV efavirenz, DTG dolutegravir, LPV lopinavir, Others= darunavir, raltegravie, elvitegravir and rilpivirine. Log-rank test, 2-sided no adjustment for multiple comparisons.
In the multivariate Poisson regression model, age at 35–49 years (adjusted incidence rate ratio [aIRR] 3.04, 2.37–3.90; Reference: 18–24 years; Table 2 and Fig. 2), 50+ years (7.37, 5.77–9.42), location in the Southwestern (2.86, 2.08–3.93; Reference: Northern China) and Eastern China (2.34, 1.68–3.26), and >30 days to ART initiation (2.00, 1.50–2.67; Reference: same-day initiation) were risk factors for increased incidence of all-cause mortality; whereas female (0.54, 0.49–0.60; Reference: male), homosexual transmission (0.50, 0.44–0.58; Reference: heterosexual), location in the Southern China (0.22, 0.11–0.45; Reference: Northern China), and initial ART in 2018 (0.86, 0.80–0.93; Reference: 2017) were protective factors. Compared to patients who initiated NVP based ART regimen, patients who initiated EFV (0.62, 0.51–0.76), DTG (0.43, 0.18–0.98), and LPV (0.54, 0.36–0.80) based ART regimens had significantly lower rates of incidence of all-cause mortality. After stratified by cause of death, compared to patients who initiated NVP based ART regimen, patients who initiated EFV (0.48, 0.39–0.60), DTG (0.28, 0.11–0.72), and LPV (0.22, 0.13–0.37) based ART regimens had significantly lower rates of incidence of AIDS-related mortality; patients who initiated other uncommon drugs (6.53, 2.05–20.80) based ART regimens had significantly higher rates of incidence of non-AIDS-related mortality. Results for ART switch, LTFU, and CD4 improvement were shown in Table S2.
For each third drug comparison, differences of all-cause mortality between the EFV group and the NVP group (aIRR 0.64, 0.53–0.79; Table 3), the DTG group and the NVP group (0.27, 0.11–0.67), and the LPV group and the NVP group (0.49, 0.33–0.75), were significant. After stratified by cause of death, differences of AIDS-related mortality between the EFV group and the NVP group (aIRR 0.49, 0.40–0.62), the DTG group and the NVP group (0.17, 0.08–0.40), the LPV group and the NVP group (0.20, 0.12–0.33), and the LPV group and the EFV group (0.46, 0.29–0.74), were significant; differences of non-AIDS-related mortality between the others group and the NVP group (aIRR 7.74, 1.03–58.17), and the others group and the EFV group (5.78, 1.54–21.71), were significant.
Sensitivity analysis using Cox models showed that the results were about consistent with the primary analysis (Table S3 and S4).
Discussion
In this study, we did not observe significant differences in all-cause mortality of PLHIV between the majority of initial ART regimens during the clinical care in China. After adjusting for potential confounders, only the differences between the EFV group and the NVP group, the DTG group and the NVP group, and the LPV group and the NVP group were found. After stratifying cause of mortality, we found that the differences in mortality between initial ART regimens were mainly observed in AIDS-related mortality.
In the multivariate Poisson regression analysis, we observed a higher rate of ART switch among patients who initiated NVP, DTG, or regimens based on other regimens compared to those who initiated EFV or LPV based, which contrasts with previous studies in high-income countries. A retrospective, observational study from a large-scale medical claims database in Japan27 found that the switch rate constantly increased over four years for NNRTIs (17.8–45.2%) and PIs (16.2–47.6%) from 2011 to 2016, while INSTI maintained a low switch rate (2.3–7.6%). Similarly, a multicentre cohort study in the United States28 found that compared to EFV/TDF/FTC users, atazanavir (ATV)/r + TDF/FTC users switched more (rate ratio [RR] = 1.80, 95% CI, 1.17–2.76), while those on DTG/ABC/3TC (RR [95% CI] = 0.16 [0.08–0.31]) or EVG/c/TAF/FTC (RR [95% CI] = 0.12 [0.06–0.27]) switched less. One possible reason for these findings is that long-term INSTI-based prescriptions are expensive in China. The cost of a bottle of DTG in China was CNY 1880, or approximately USD 274, which was a significant burden for patients (communication with infectious disease physicians). Therefore, once the condition of patients who started INSTI-based regimens was under control, more may tend to switch to the NFATP-sponsored regimens. Furthermore, the increased incidence of severe adverse events and risk of virological failure with those who initiated NVP-based ART, which has been extensively studied, may have contributed to the higher ART switch rate29,30,31,32,33,34,35. However, we acknowledge that alternative factors beyond those mentioned may contribute to the differences in ART switch rates. Additional research is needed to further explore and elucidate the underlying reasons for these discrepancies.
Consistent with previous studies, we found that patients who initiated EFV based ART regimen had lower LTFU rates. A large-scale cohort study in 62,500 adults with HIV in Europe and North America19 found that LTFU was the lowest in those on EFV-based regimens, but otherwise broadly similar across the regimens. Another study, which analyzed data from 18 cohorts in Europe and North America from 2002–200936, found that compared to EFV, NVP and LPV were associated with higher rates of ART interruption for more than 1 month (subdistribution hazard ratios 1.5, 95% CI 1.3–1.7; and 1.4, 1.2–1.5, respectively). Following the WHO recommendations, EFV based ART regimen have been commonly used as first-line therapy for PLHIV in China since 2011 and were available through the NFATP12,13. The favorable efficacy and superior tolerability of this ART regimen in PLHIV in China were demonstrated in a cohort study carried by the China HIV/AIDS Clinical Trial Network (Clinicaltrials.gov ID: NCT01844297). It was reported that the high accessibility and efficacy were contributing factors to a low rate of LTFU29,30,31,32,33,34,35.
We found that patients who initiated DTG, LPV and others-based ART regimens had significantly higher CD4 improvement rates compared to NVP based, which was similar to existing studies. A retrospective analysis in Thailand37 found that compared with the EFV group (patient who initiated EFV ART regimen), the DTG group showed greater increments of CD4 + (P < 0.001) T-cell counts at week 96. Another retrospective study of patients registering with the NFATP in Beijing, China from July 2012 to January 201738 found that patients in the LPV/ritonavir group were more likely to display improvements in CD4 + T-cell count over time than those in the EFV group (P < 0.001). The CD4 + T-cell count reflects the immune status and risk of opportunistic infections at the time of treatment for PLHIV. In addition, the favorable efficacy and safety profile of INSTIs compared with other drug classes were widely studied in randomised trials3,4,5,39,40,41,42,43,44,45.
We found no significant differences in mortality between patients who initiated most of the ART regimens. A recent study in 62,500 adults with HIV in Europe and North America19 found that there was little evidence that mortality rates differed between regimens with DTG, EVG, RPV, DRV, or EFV as the third drug. However, mortality was higher for RAL compared with DTG (aHR 1.49, 95% CI 1.15–1.94), EVG (1.86, 1.43–2.42), RPV (1.99, 1.49–2.66), DRV (1.62, 1.33–1.98), and EFV (2.12, 1.60–2.81) regimens19. Similar results were obtained in two other long-term observational studies46,47. Our finding was consistent with the previous literature in high-income countries, but as the data were from LMICs, this provided more evidence of the clinical outcomes of the initiation of INSTI-based ART. Notably, the differences in mortality were mainly observed in people who started NVP-based regimen in our study. As an ART drug recommended in 2009, NVP is currently predominantly used in LMICs46,48. Similar to EFV, another drug recommended in the same year, patients initiating ART with NVP tend to have a higher median age in our data due to the introduction of other new drugs over the past decade. Many research has reported the efficacy gap between NVP and other drugs48,49, which is consistent with our findings. It is noteworthy that, compared to the other less common third drugs, the non-AIDS-related mortality among PLHIV initiating NVP and EFV has significantly decreased. This may be related to the side effects of less common drugs, warranting further research to elucidate the underlying causes of this phenomenon. Moreover, subsequent studies on the efficacy and mortality reduction of INSTIs, represented by DTG, will be very valuable, because China adopted DTG/3TC in the NFATP-sponsored regimens in 2021, which made it available free of charge for PLHIV from then on50. The government spending on HIV has steadily increased from 139 million USD in 2006 to 1,357 million USD in 202051. However, given the heavy impact of the COVID-19 pandemic, which started in 2020 and spread globally, on the continuum of HIV care, including ART follow-up, the impact of the epidemic should be appropriately excluded in subsequent studies52.
Our study was based on a large population between 2017 and 2019 covering a variety of regions in China, which ensured the representativeness of the sample and the robustness of the findings. To the best of our knowledge, this is the first cohort study to investigate the associations of modern initial first-line ART regimens with all-cause mortality in PLHIV in China. However, there are several limitations. First, it is important to note that our study is observational and does not demonstrate a causal relationship between initial ART regimen and clinical outcomes, as the treatment was not randomly assigned. There might have been some unmeasured or underlying causes that could bias our results. For example, given that all INSTIs and most PIs were not available free of charge before 2021 in China, patients’ socioeconomic status could potentially affect our results. Due to the sensitivity of HIV data, obtaining and adjusting data on socioeconomic indicators such as income, employment status, and location of residence is challenging, which is consistent with similar studies19,47. If more data become available in the future, subsequent studies would further enhance our understanding of the topic. However, we adjusted for a range of demographic factors (particularly region) in our multivariable models using current available data, which we believe helps to mitigate the potential impact of socioeconomic status. Second, we were unable to consider the virological suppression or failure of PLHIV as a clinical outcome given that most of the viral load were missing in China. Third, the precision of our results was relatively low due to the small number of outcomes observed in certain groups (such as RPV, EVG and DRV groups). This was mainly due to the late introduction of these drugs in China, while the high price limited patients’ consideration during our study period. Finally, our study period may be relatively short to fully capture the outcomes among PLHIV. However, given the implementation of the treat-all policy in China in 2016, and the significant impact of COVID-19 pandemic on the HIV care continuum in 202052,53, we had to limit the study duration to these three years. Additional long-term research is needed to further elucidate this topic after the lifting of zero-COVID policy in December 2022 in China.
In summary, significant differences in mortality rates of PLHIV between the majority of initial ART regimens were not observed in China. Our finding provided more evidence of the clinical outcomes of the initiation of INSTI-based ART. Further efforts are needed to confirm the reasons for the lack of significant improvement in mortality rates with the use of INSTIs in clinical practice.
Methods
Ethics approval
Ethics approval was obtained from the Ethics Review Committee for Biomedical Research, School of Public Health (Shenzhen), Sun Yat-sen University (Ref: 2020022). The data used in this study do not contain any identifying information available to the researchers.
Study design and participants
A retrospective multicenter cohort study was performed using data extracted from the NFATP database. The database introduction could be found elsewhere7. Anonymised programmatic data on ART initiation and collection in PLHIV between January 1, 2017 and December 31, 2019 were collected from three provincial and municipal Centers for Disease Control and Prevention (CDCs) in Chongqing, Jiangsu and Dehong, and nine major infectious disease hospitals specialized in HIV care in Guangzhou, Shenzhen, Hohhot, Tianjin, Shenyang (2), Beijing, Shijiazhuang and Dalian in China. We included all subjects who were older than 18 years, started triple ART between January 1, 2017 and September 30, 2019, and had available baseline CD4 + T-cell count measurements (Fig. S1). The follow-up records were collected until study end (December 31, 2019).
Jiangsu is a province in Eastern China; Chongqing is a municipality and Dehong is an autonomous minority prefecture in Southwestern China. Guangzhou and Shenzhen are located in Southern China; Hohhot, Beijing, Tianjin and Shijiazhuang are cities in Northern China; Shenyang and Dalian are located in Northeastern China. These regions collectively represent 21.3% [41,018 / (57,194 + 64,170 + 71,204)] of newly reported HIV/AIDS cases in China during this period54. In China, CDCs at various levels are established to implement public health technical management and services, and are responsible for HIV surveillance. PLHIV are required to initiate ART and pick up drugs from designated infectious disease hospitals.
Outcomes
Baseline and follow-up data, including social-demographics characteristics, clinical information, and laboratory test data, were extracted from the NFATP database. Details about the data were published elsewhere10,55. Baseline characteristics measured at ART initiation include age (18–24, 25–34, 35–49, 50+), sex (male and female, identified by the NFATP database based on the China ID card system), route of transmission (heterosexual, homosexual and others [including 90.4% intravenous drug use, 7.2% blood transfusion, 2.4% mother-to-child transmission]), region (Northern China [Hohhot, Shijiazhuang, Beijing and Tianjin], Northeastern China [Dalian and Shenyang], Southern China [Guangzhou and Shenzhen], Southwestern China [Chongqing and Dehong], and Eastern China [Jiangsu]), time from diagnosis to ART initiation (time to ART initiation; same-day, 1–7 days, 8–30 days, >30 days), year of ART initiation (2017, 2018, 2019), and CD4 + T-cell counts. Follow-up data included initial ART regimen and NRTI backbone. Third ART drugs that were most commonly utilized in the study period included NVP, EFV, DTG, LPV, and others (including DRV, RAL, EVG and RPV). The NRTI backbone pairs were stratified as: 3TC and TDF, 3TC and AZT, and others.
The primary outcomes of interest were ART switch, retention, CD4 improvement, and mortality. ART switch refers to changes in third component for any reason that occurs during a patient’s follow-up visit. Retention was represented by LTFU, which was defined by patients who were >180 days (as recommended by a systematic review56) from the last clinical visit or drug pick-up during the study period. CD4 improvement was represented by changes in longitudinally-collected CD4 measurements. We defined CD4 improvement as transition of PLHIV from CD4 < 500 cells/μL to CD4 > 500 cells/μL. Mortality referred to all-cause mortality in PLHIV, including AIDS-related mortality and non-AIDS-related mortality.
Statistical analyses
We used descriptive statistics to summarize baseline characteristics of PLHIV stratified by initial ART regimen. The median and IQR were used to describe continuous variables, and frequencies and proportions were used to describe categorical variables. Kruskal-Wallis tests were used to assess the associations of continuous variables with the initial ART class, and Pearson’s chi-squared tests were used to assess the associations between categorical variables and the initial ART class.
We then used Kaplan-Meier curves to calculate stratified cumulative incidences of four outcomes, including ART switch, LTFU, CD4 improvement, and death. Individuals included in the study were censored at the time of settle in new areas, or when switched their first-line ART regimen, or when LTFU definition was met, or death, or when study end, whichever occurred first. Poisson regression model with a time offset and robust variances, adjusted for the main covariates, was used to estimate IRRs of outcomes by initial ART class57,58. To explore the association between initial ART regimen and different causes of death, we conducted the same analyses for both AIDS-related mortality and non-AIDS-related mortality. For all analyses, we fitted an unadjusted model and a model adjusted for the main variables, including baseline age, sex, route of HIV acquisition, region, time to ART initiation, year of ART initiation, CD4 + T-cell counts, and NRTI backbone.
To check the robustness of our findings, we conducted a sensitivity analysis using Cox models to reanalyse the data. All statistical tests were two-sided, and P < 0.05 was considered indicating strong evidence against the null hypothesis. All statistical analyses were conducted using R 4.2.1 (R Foundation for Statistical Computing, Vienna, Austria).
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
The raw data that support the findings of this study are not publicly available for confidentiality reasons, since these patients may be re-identified through various techniques, such as data linkage or combining datasets. The processed data are available on reasonable request to the corresponding author, H.Z., with each request subject to ethical and legislative review from the respective data sources. Source data are provided with this paper.
Code availability
The R code used in the analyses was provided in 10.5281/zenodo.8240994. However, this study did not generate new or customized code/software. The Poisson regression models were fitted using the glm function from the base R package. The robust standard errors of Poisson models were computed using the vcovHC function from the sandwich R package. The Cox Proportional models were fitted using the coxph function from the survival R package.
References
Gandhi R. T., et al. Antiretroviral drugs for treatment and prevention of hiv infection in adults: 2022 recommendations of the International Antiviral Society-USA Panel. JAMA 329, 63–84 (2022).
Ryom, L. et al. 2019 update of the European AIDS clinical society guidelines for treatment of people living with HIV version 10.0. HIV Med. 21, 617–624 (2020).
Stellbrink, H.-J. et al. Dolutegravir in antiretroviral-naive adults with HIV-1: 96-week results from a randomized dose-ranging study. AIDS 27, 1771–1778 (2013).
Walmsley, S. L. et al. Dolutegravir plus abacavir-lamivudine for the treatment of HIV-1 infection. N. Engl. J. Med. 369, 1807–1818 (2013).
Zolopa A., et al. A randomized double-blind comparison of coformulated elvitegravir/cobicistat/emtricitabine/tenofovir disoproxil fumarate versus efavirenz/emtricitabine/tenofovir disoproxil fumarate for initial treatment of HIV-1 infection: analysis of week 96 results. J. Acquir. Immune Defic. Syndr. 63, 96–100 (2013).
Zhu, H. et al. Decreasing excess mortality of HIV-infected patients initiating antiretroviral therapy: comparison with mortality in general population in China, 2003-2009. J. Acquir. Immune Defic. Syndr. 63, e150–e157 (2013).
Zhang, F. et al. Effect of earlier initiation of antiretroviral treatment and increased treatment coverage on HIV-related mortality in China: a national observational cohort study. Lancet Infect. Dis. 11, 516–524 (2011).
Zhang F., et al. Five-year outcomes of the China National Free Antiretroviral Treatment Program. Ann. Intern. Med.151, 241–251(2009)
Zhang, F. et al. The effect of highly active antiretroviral therapy on mortality among HIV-infected former plasma donors in China. Clin. Infect. Dis. 47, 825–833 (2008).
Ma, Y. et al. Cohort profile: the Chinese national free antiretroviral treatment cohort. Int. J. Epidemiol. 39, 973–979 (2010).
Chen, Q. et al. Effect of late testing and antiretroviral treatment on mortality among people living with HIV in the era of treat-all in guangdong province, China, 1992-2018: a cohort study. Front. Public Health 10, 851117 (2022).
Zhang, F. et al. HIV, hepatitis B virus, and hepatitis C virus co-infection in patients in the China National Free Antiretroviral Treatment Program, 2010-12: a retrospective observational cohort study. Lancet Infect. Dis. 14, 1065–72. (2014).
Su, S. et al. Gaps in the continuum of HIV care: long pretreatment waiting time between hiv diagnosis and antiretroviral therapy initiation leads to poor treatment adherence and outcomes. Biomed. Res. Int. 2016, 2648923 (2016).
Cao, W., Hsieh, E. & Li, T. Optimizing treatment for adults with HIV/AIDS in China: successes over two decades and remaining challenges. Curr. HIV/AIDS Rep. 17, 26–34 (2020).
AIDS and Hepatitis C Professional Group, Society of Infectious Diseases, Chinese Medical Association; Chinese Center for Disease Control and Prevention. Chinese Guidelines for Diagnosis and Treatment of HIV/AIDS (2021). Zhonghua Nei Ke Za Zhi. 60, 1106–1128 (2021).
Yang, Z. et al. Prevalence of integrase strand transfer inhibitor (INSTIs) resistance mutations in Henan Province, China (2018-2020). Infection 49, 1195–202 (2021).
Lan Y., et al. Drug resistance to integrase strand-transfer inhibitors among HIV-1-infected adults in guangdong, China. Pathogens 11, 1321(2022)
Fan, W. et al. Prevalence of resistance mutations associated with integrase inhibitors in therapy-naive HIV-positive patients in Baoding, Hebei province, China. Front. Genet. 13, 975397 (2022).
Trickey, A. et al. Associations of modern initial antiretroviral drug regimens with all-cause mortality in adults with HIV in Europe and North America: a cohort study. Lancet HIV 9, e404–e13 (2022).
Menard, A. et al. Dolutegravir and weight gain: an unexpected bothering side effect? AIDS 31, 1499–500 (2017).
Bourgi, K. et al. Weight gain among treatment-naïve persons with HIV starting integrase inhibitors compared to non-nucleoside reverse transcriptase inhibitors or protease inhibitors in a large observational cohort in the United States and Canada. J. Int. AIDS Soc. 23, e25484 (2020).
Crum-Cianflone, N. et al. Increasing rates of obesity among HIV-infected persons during the HIV epidemic. PLoS One 5, e10106 (2010).
Koethe, J. R. et al. Rising obesity prevalence and weight gain among adults starting antiretroviral therapy in the United States and Canada. AIDS Res. Hum. Retrovir. 32, 50–58 (2016).
Neesgaard, B. et al. Associations between integrase strand-transfer inhibitors and cardiovascular disease in people living with HIV: a multicentre prospective study from the RESPOND cohort consortium. Lancet HIV 9, e474–e85. (2022).
Mbhele, N., Chimukangara, B. & Gordon, M. HIV-1 integrase strand transfer inhibitors: a review of current drugs, recent advances and drug resistance. Int. J. Antimicrob. Agents 57, 106343 (2021).
Steegen K., et al. Resistance in patients failing integrase strand transfer inhibitors: a call to replace raltegravir with dolutegravir in third-line treatment in South Africa. Open Forum Infect. Dis. 6, ofz377 (2019).
Ruzicka, D. J., Kuroishi, N., Oshima, N., Sakuma, R. & Naito, T. Switch rates, time-to-switch, and switch patterns of antiretroviral therapy in people living with human immunodeficiency virus in Japan, in a hospital-claim database. BMC Infect. Dis. 19, 505 (2019).
Li, X. et al. Recent trends and effectiveness of antiretroviral regimens among men who have sex with men living with HIV in the United States: the multicenter AIDS Cohort Study (MACS) 2008-2017. Open Forum Infect. Dis. 6, ofz333 (2019).
WHO. Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: recommendations for a public health approach. (WHO, 2013).
Cain, L. E. et al. The effect of efavirenz versus nevirapine-containing regimens on immunologic, virologic and clinical outcomes in a prospective observational study. AIDS 26, 1691–1705 (2012).
van den Berg-Wolf, M. et al. Virologic, immunologic, clinical, safety, and resistance outcomes from a long-term comparison of efavirenz-based versus nevirapine-based antiretroviral regimens as initial therapy in HIV-1-infected persons. HIV Clin. Trials 9, 324–336 (2008).
Tang, M. W., Kanki, P. J. & Shafer, R. W. A review of the virological efficacy of the 4 World Health Organization-recommended tenofovir-containing regimens for initial HIV therapy. Clin. Infect. Dis. 54, 862–875 (2012).
Nachega, J. B. et al. Efavirenz versus nevirapine-based initial treatment of HIV infection: clinical and virological outcomes in Southern African adults. AIDS 22, 2117–2125 (2008).
Shearer, K. et al. The relation between efavirenz versus nevirapine and virologic failure in Johannesburg, South Africa. J. Int. AIDS Soc. 17, 19065 (2014).
Kedir, M. S., Gemeda, D. H. & Suleman, S. Treatment outcomes of nevirapine- versus efavirenz-based highly active antiretroviral therapy regimens among antiretroviral-naive adult patients in ethiopia: a cohort study. Ther. Innov. Regul. Sci. 49, 443–449 (2015).
Abgrall, S. et al. Durability of first ART regimen and risk factors for modification, interruption or death in HIV-positive patients starting ART in Europe and North America 2002-2009. AIDS 27, 803–813 (2013).
Chan, P. et al. Immunological, cognitive, and psychiatric outcomes after initiating efavirenz- and dolutegravir-based antiretroviral therapy during acute human immunodeficiency virus infection. Clin. Infect. Dis. 76, e718–e726 (2023).
Su, B. et al. Efficacy and tolerability of Lopinavir/Ritonavir- and Efavirenz-based initial antiretroviral therapy in HIV-1-infected patients in a tertiary care hospital in Beijing, China. Front. Pharm. 10, 1472 (2019).
Clotet, B. et al. Once-daily dolutegravir versus darunavir plus ritonavir in antiretroviral-naive adults with HIV-1 infection (FLAMINGO): 48 week results from the randomised open-label phase 3b study. Lancet 383, 2222–2231 (2014).
Lennox, J. L. et al. Efficacy and tolerability of 3 nonnucleoside reverse transcriptase inhibitor-sparing antiretroviral regimens for treatment-naive volunteers infected with HIV-1: a randomized, controlled equivalence trial. Ann. Intern. Med. 161, 461–471 (2014).
Orrell, C. et al. Fixed-dose combination dolutegravir, abacavir, and lamivudine versus ritonavir-boosted atazanavir plus tenofovir disoproxil fumarate and emtricitabine in previously untreated women with HIV-1 infection (ARIA): week 48 results from a randomised, open-label, non-inferiority, phase 3b study. Lancet HIV 4, e536–e546 (2017).
Squires, K. et al. Integrase inhibitor versus protease inhibitor based regimen for HIV-1 infected women (WAVES): a randomised, controlled, double-blind, phase 3 study. Lancet HIV 3, e410–e420 (2016).
Lennox, J. L. et al. Raltegravir versus Efavirenz regimens in treatment-naive HIV-1-infected patients: 96-week efficacy, durability, subgroup, safety, and metabolic analyses. J. Acquir. Immune Defic. Syndr. 55, 39–48 (2010).
Walmsley, S. et al. Brief report: Dolutegravir Plus Abacavir/Lamivudine for the Treatment of HIV-1 infection in antiretroviral therapy-naive patients: week 96 and week 144 results from the SINGLE randomized clinical trial. J. Acquir. Immune Defic. Syndr. 70, 515–519 (2015).
Venter, W. D. F. et al. Dolutegravir plus Two Different Prodrugs of Tenofovir to Treat HIV. N. Engl. J. Med. 381, 803–815 (2019).
Lu, H. et al. Clinical effectiveness of integrase strand transfer inhibitor–based antiretroviral regimens among adults with human immunodeficiency virus: a collaboration of Cohort studies in the United States and Canada. Clin. Infect. Dis. 73, e1408–e1414 (2020).
Cole, S. R. et al. Incident AIDS or death after initiation of human immunodeficiency virus treatment regimens including Raltegravir or Efavirenz among adults in the United States. Clin. Infect. Dis. 64, 1591–1596 (2017).
Amour, M. A. et al. Predictors of mortality among adolescents and young adults living with HIV on antiretroviral therapy in Dar es Salaam, Tanzania: a retrospective cohort study. J. Int. AIDS Soc. 25, e25886 (2022).
Pillay, P., Ford, N., Shubber, Z. & Ferrand, R. A. Outcomes for efavirenz versus nevirapine-containing regimens for treatment of HIV-1 infection: a systematic review and meta-analysis. PLoS One 8, e68995 (2013).
National Healthcare Security Administration. National Drug Catalogue for Basic Medical Insurance, Work-related Injury Insurance and Maternity Insurance (2021). http://www.nhsa.gov.cn/art/2021/12/3/art_37_7429.html.
Aidsdatahub.org. AIDS data, China Review. (2023). https://www.aidsdatahub.org/country-profiles/china.
Wu, X. et al. The impact of COVID-19 non-pharmaceutical interventions on HIV care continuum in China: an interrupted time series analysis. Lancet Reg. Health West. Pac. 29, 100569 (2022).
Wu, X. et al. The Impact of COVID-19 lockdown on cases of and deaths from AIDS, Gonorrhea, Syphilis, Hepatitis B, and Hepatitis C: interrupted time series analysis. JMIR Public Health Surveill. 9, e40591 (2023).
National Administration of Disease Prevention and Control. National Overview of Notifiable Infectious Diseases. http://www.nhc.gov.cn/jkj/s2907/new_list.shtml.
Li, L. et al. Sex differences in HIV treatment outcomes and adherence by exposure groups among adults in Guangdong, China: a retrospective observational cohort study. EClinicalMedicine 22, 100351 (2020).
Chi, B. H. et al. Universal definition of loss to follow-up in HIV treatment programs: a statistical analysis of 111 facilities in Africa, Asia, and Latin America. PLoS Med. 8, e1001111 (2011).
Zou, G. A modified poisson regression approach to prospective studies with binary data. Am. J. Epidemiol. 159, 702–706 (2004).
Zou, G. Y. & Donner, A. Extension of the modified Poisson regression model to prospective studies with correlated binary data. Stat. Methods Med. Res. 22, 661–670 (2013).
Acknowledgements
H.Z. is supported by the Shenzhen Science and Technology Innovation Commission Basic Research Program [JCYJ20190807155409373], the Natural Science Foundation of China Excellent Young Scientists Fund [82022064], Natural Science Foundation of China International/Regional Research Collaboration Project [72061137001], the Sanming Project of Medicine in Shenzhen [SZSM201811071], the High Level Project of Medicine in Longhua, Shenzhen [HLPM201907020105], Special Support Plan for High-Level Talents of Guangdong Province [2019TQ05Y230], the Fundamental Research Funds for the Central Universities [58000-31620005], Non-profit Central Research Institute Fund of Chinese Academy of Medical Sciences [2020-JKCS-030]. G.W. is supported by the Chongqing Talents Program for Innovative and Entrepreneurial Pioneers [cstc2021ycjh-bgzxm0097], the Chongqing Natural Science Foundation Project [cstc2021jcyj-msxmX1171], the Chinese State Key Laboratory of Infectious Disease Prevention and Control [2021SKLID303]. P.M. is supported by the Health Science and Technology Project of Tianjin Health Commission [ZC20037], the Tianjin Key Medical Discipline (Specialty) Construction Project [Infectious Diseases ZD02]. L.L. is supported by the National Key Research and Development Program of China [2022YFC2304800], the Science and Technology Project of Guangzhou [20220020285]. X.H. is supported by the Public Health Talent Grant by Beijing Municipal Health Commission [Global Health Governance-02-12], the Capital Health Development Research [2022-2-2185; 2022-1G-3011]. B.S. is supported by the High-Level Public Health Specialized Talents Project of Beijing Municipal Health Commission [2022-2-018], the National Key R&D Program of China [2021YFC2301900; 2021YFC2301905], the Beijing Key Laboratory for HIV/AIDS Research [BZ0089]. T.Z. is supported by the High-Level Public Health Specialized Talents Project of Beijing Municipal Health Commission [2022-1-007], the Climbing the Peak (Dengfeng) Talent Training Program of Beijing Hospitals Authority (DFL20191701). All funding parties did not have any role in the design of the study or in the explanation of the data. We thank the Prof. Junfeng Wang from Utrecht University, Netherlands for supporting the statistical methods and R codes in our study. We thank Yi-Fan Lin from the School of Public Health (Shenzhen), Sun Yat-sen University for supporting the statistical methods in our study.
Author information
Authors and Affiliations
Contributions
X.W. conceived and designed the study in consultation with H.Z., H.Z., G.W., P.M., R.W., L.L., J.X., Q.L., Y.Y., L.W., X.X., Y.Q., G.F., X.H., B.S., T.Z., and H.W. contributed to data collection. X.W., Y.C., and Y.L. contributed to data analysis and presentation. X.W. drafted the report with all authors critically reviewing the paper. All authors saw and approved the final report.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks the anonymous reviewers for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wu, X., Wu, G., Ma, P. et al. Associations of modern initial antiretroviral therapy regimens with all-cause mortality in people living with HIV in resource-limited settings: a retrospective multicenter cohort study in China. Nat Commun 14, 5334 (2023). https://doi.org/10.1038/s41467-023-41051-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-023-41051-w
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.