Abstract
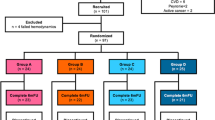
We aim to summarize the latest evidence on platelet-rich plasma (PRP) intracavernosal injections efficacy in men affected by primary organic erectile dysfunction (ED). We reviewed the literature for randomized controlled trials (RCTs) or prospective and retrospective comparative studies evaluating PRP alone or in combination for ED treatment. A comprehensive search in PubMed, Scopus, Web of Science, and ClinicalTrials.gov was performed for English language full-text articles or conference abstracts. A qualitative and quantitative data synthesis was provided. Overall, seven records were included: three RCTs evaluated PRP vs. placebo, one study separately tested PRP and low-intensity shock wave therapy (Li-SWT), three studies compared Li-SWT or low-intensity pulsed ultrasound alone with their combination with PRP. Of 641 included patients, 320 received PRP. Despite the heterogeneity among inclusion criteria, dose and protocol of PRP administration, and outcomes measured, most studies independently reported better sexual outcomes in patients who received PRP, without significant severe side effects. In meta-analysis, where only placebo-controlled studies were included, patients treated with PRP showed higher International Index of Erectile Function (erectile function domain) score compared to patients who received placebo: pooled mean difference (95% Confidence Interval) of 2.99 (1.86, 4.13) after 1 month (209 patients) vs. 2.85 (1.61, 4.09) after 3 months (204 patients) vs. 3.21 (1.82, 4.60) after 6 months (199 patients) of follow-up. In men affected by primary organic ED, PRP intracavernosal injections demonstrated an objective improvement or at least a tendency in erectile function recovery. Patient numbers, and the short-term follow-up may limit the generalizability of these observations. High quality, large-scale, and standardized controlled trials are needed before recommending its definitive use in clinical practice.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The full data set and code for statistical analyses is available upon request.
References
NIH Consensus Conference. Impotence. NIH consensus development panel on impotence. JAMA. 1993;270:83–90.
Quilter M, Hodges L, von Hurst P, Borman B, Coad J. Male sexual function in New Zealand: a population-based cross-sectional survey of the prevalence of erectile dysfunction in men aged 40–70 years. J Sex Med. 2017;14:928–36.
Çayan S, Kendirci M, Yaman Ö, Aşçı R, Orhan İ, Usta MF, et al. Prevalence of erectile dysfunction in men over 40 years of age in Turkey: results from the Turkish society of andrology male sexual health study group. Turk J Urol. 2017;43:122–9.
Corona G, Lee DM, Forti G, O’Connor DB, Maggi M, O’Neill TW, et al. Age-related changes in general and sexual health in middle-aged and older men: results from the European Male Ageing Study (EMAS). J Sex Med. 2010;7:1362–80.
Buvat J, Glasser D, Neves RCS, Duarte FG, Gingell C, Moreira ED, et al. Sexual problems and associated help-seeking behavior patterns: results of a population-based survey in France. Int J Urol. 2009;16:632–8.
Teles AG, Carreira M, Alarcão V, Sociol D, Aragüés JM, Lopes L, et al. Prevalence, severity, and risk factors for erectile dysfunction in a representative sample of 3548 portuguese men aged 40 to 69 years attending primary healthcare centers: results of the Portuguese erectile dysfunction study. J Sex Med. 2008;5:1317–24.
Laumann EO, Glasser DB, Neves RCS, Moreira ED, GSSAB Investigators’ Group. A population-based survey of sexual activity, sexual problems and associated help-seeking behavior patterns in mature adults in the United States of America. Int J Impot Res. 2009;21:171–8.
Capogrosso P, Ventimiglia E, Boeri L, Pozzi E, Chierigo F, Schifano N, et al. Should we tailor the clinical management of erectile dysfunction according to different ages? J Sex Med. 2019;16:999–1004.
Capogrosso P, Ventimiglia E, Boeri L, Cazzaniga W, Chierigo F, Pederzoli F, et al. Age at first presentation for erectile dysfunction: analysis of changes over a 12-yr period. Eur Urol Focus. 2019;5:899–905.
Elterman DS, Bhattacharyya SK, Mafilios M, Woodward E, Nitschelm K, Burnett AL. The quality of life and economic burden of erectile dysfunction. Res Rep. Urol. 2021;13:79–86.
Salonia A, Bettocchi C, Boeri L, Capogrosso P, Carvalho J, Cilesiz NC, et al. European association of urology guidelines on sexual and reproductive health-2021 update: male sexual dysfunction. Eur Urol. 2021;80:333–57.
Ventimiglia E, Cazzaniga W, Pederzoli F, Frego N, Chierigo F, Capogrosso P, et al. The role of neutrophil-to-lymphocyte ratio in men with erectile dysfunction-preliminary findings of a real-life cross-sectional study. Andrology. 2018;6:559–63.
Boeri L, Capogrosso P, Pederzoli F, Ventimiglia E, Frego N, Chierigo F, et al. Unrecognized prediabetes is highly prevalent in men with erectile dysfunction-results from a cross-sectional study. J Sex Med. 2018;15:1117–24.
Althof SE, O’leary MP, Cappelleri JC, Hvidsten K, Stecher VJ, Glina S, et al. Sildenafil citrate improves self-esteem, confidence, and relationships in men with erectile dysfunction: results from an international, multi-center, double-blind, placebo-controlled trial. J Sex Med. 2006;3:521–9.
Shabsigh R, Kim ED, Rosen RC, Shinghal R, Natanegara F, Muram D, et al. Response to treatment with tadalafil in men with erectile dysfunction who reported no successful intercourse attempts at baseline. Int J Impot Res. 2008;20:554–60. https://doi.org/10.1038/ijir.2008.38.
Porst H, Rosen R, Padma-Nathan H, Goldstein I, Giuliano F, Ulbrich E, et al. The efficacy and tolerability of vardenafil, a new, oral, selective phosphodiesterase type 5 inhibitor, in patients with erectile dysfunction: the first at-home clinical trial. Int J Impot Res. 2001;13:192–9. https://doi.org/10.1038/sj.ijir.3900713.
Hellstrom WJG, Freier MT, Serefoglu EC, Lewis RW, DiDonato K, Peterson CA. A phase II, single-blind, randomized, crossover evaluation of the safety and efficacy of avanafil using visual sexual stimulation in patients with mild to moderate erectile dysfunction. BJU Int. 2013;111:137–47.
Linet OI, Ogrinc FG. Efficacy and safety of intracavernosal alprostadil in men with erectile dysfunction. The Alprostadil Study Group. N Engl J Med. 1996;334:873–7.
Dutta TC, Eid JF. Vacuum constriction devices for erectile dysfunction: a long-term, prospective study of patients with mild, moderate, and severe dysfunction. Urology. 1999;54:891–3.
Chierigo F, Capogrosso P, Dehò F, Pozzi E, Schifano N, Belladelli F, et al. Long-term follow-up after penile prosthesis implantation-survival and quality of life outcomes. J Sex Med. 2019;16:1827–33.
Vardi Y, Appel B, Kilchevsky A, Gruenwald I. Does low intensity extracorporeal shock wave therapy have a physiological effect on erectile function? Short-term results of a randomized, double-blind, sham controlled study. J Urol. 2012;187:1769–75.
Haahr MK, Jensen CH, Toyserkani NM, Andersen DC, Damkier P, Sørensen JA, et al. Safety and potential effect of a single intracavernous injection of autologous adipose-derived regenerative cells in patients with erectile dysfunction following radical prostatectomy: an open-label phase I clinical trial. EBioMedicine. 2016;5:204–10.
Ding X-G, Li S-W, Zheng X-M, Hu L-Q, Hu W-L, Luo Y. The effect of platelet-rich plasma on cavernous nerve regeneration in a rat model. Asian J Androl. 2009;11:215–21.
Wu C-C, Wu Y-N, Ho H-O, Chen K-C, Sheu M-T, Chiang H-S. The neuroprotective effect of platelet-rich plasma on erectile function in bilateral cavernous nerve injury rat model. J Sex Med. 2012;9:2838–48.
Anastasiadis E, Ahmed R, Khoja AK, Yap T. Erectile dysfunction: is platelet-rich plasma the new frontier for treatment in patients with erectile dysfunction? A review of the existing evidence. Front Reprod health. 2022;4:944765.
Marx RE. Platelet-rich plasma (PRP): what is PRP and what is not PRP? Implant Dent. 2001;10:225–8.
Daif ET. Effect of autologous platelet-rich plasma on bone regeneration in mandibular fractures. Dent Traumatol. 2013;29:399–403.
Taschieri S, Lolato A, Ofer M, Testori T, Francetti L, Del Fabbro M. Immediate post-extraction implants with or without pure platelet-rich plasma: a 5-year follow-up study. Oral Maxillofac Surg. 2017;21:147–57.
Alkandari MH, Touma N, Carrier S. Platelet-rich plasma injections for erectile dysfunction and peyronie’s disease: a systematic review of evidence. Sex Med Rev. 2022;10:341–52.
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8:336–41.
Hartmann KE, Matchar DB, Chang S. Chapter 6: assessing applicability of medical test studies in systematic reviews. J Gen Intern Med. 2012;27:S39–46.
Cappelleri JC, Rosen RC, Smith MD, Mishra A, Osterloh IH. Diagnostic evaluation of the erectile function domain of the international index of erectile function. Urology. 1999;54:346–51.
Rosen RC, Cappelleri JC, Smith MD, Lipsky J, Peña BM. Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int J Impot Res. 1999;11:319–26. https://doi.org/10.1038/sj.ijir.3900472.
Howick J. The Oxford 2011 levels of evidence. Oxford: Oxford Centre for Evidence-Based Medicine; 2011. http://www.cebm.net/index.aspx?o=5653.
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898.
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919.
Luo D, Wan X, Liu J, Tong T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res. 2018;27:1785–805.
Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135.
Shaher H, Fathi A, Elbashir S, Abdelbaki SA, Soliman T. Is platelet rich plasma safe and effective in treatment of erectile dysfunction? Randomized controlled study. Urology. 2023;175:114–119. https://doi.org/10.1016/j.urology.2023.01.028.
Poulios E, Mykoniatis I, Pyrgidis N, Zilotis F, Kapoteli P, Kotsiris D, et al. Platelet-Rich Plasma (PRP) improves erectile function: a double-blind, randomized, placebo-controlled clinical trial. J Sex Med. 2021;18:926–35.
Masterson TA, Molina M, Ledesma B, Zucker I, Saltzman R, Ibrahim E, et al. Platelet-rich plasma for the treatment of erectile dysfunction: a prospective, randomized, double-blind, placebo-controlled clinical trial. J Urol. 2023;210:154–61.
Geyik S. Comparison of the efficacy of low-intensity shock wave therapy and its combination with platelet-rich plasma in patients with erectile dysfunction. Andrologia. 2021;53:e14197.
Sajjad K, Sohail M, Momin HA, Shafique RA, Nazir M, Ahmad S et al. Effect of low-energy shockwave therapy versus platelets rich plasma therapy in patients with erectile dysfunction. J Pharm Res Int. (2021);33:168–72.
Ruffo A, Stanojevic N, Romeo G, Riccardo F, Trama F, Iacono F. PS-5-3 Management of erectile dysfunction using a combination treatment of low-intensity shock waves (LISW) and platelet rich plasma (PRP) intracavernosal injections. J Sexual Med. (2020);17:S133–S134.
Zasieda Y. HP-3-1 platelet rich plasma and low-intensity pulsed ultrasound combination in erectile dysfunction treatment. J Sexual Med. (2020);17:S158.
Rosen RC, Allen KR, Ni X, Araujo AB. Minimal clinically important differences in the erectile function domain of the international index of erectile function scale. Eur Urol. 2011;60:1010–6.
Grover S, Shouan A. Assessment scales for sexual disorders—a review. J Psychosexual Health. 2020;2:121–38.
Althof SE, Corty EW, Levine SB, Levine F, Burnett AL, McVary K, et al. EDITS: development of questionnaires for evaluating satisfaction with treatments for erectile dysfunction. Urology. 1999;53:793–9.
Waldinger MD, Quinn P, Dilleen M, Mundayat R, Schweitzer DH, Boolell M. A multinational population survey of intravaginal ejaculation latency time. J Sex Med. 2005;2:492–7.
Epifanova MV, Gvasalia BR, Durashov MA, Artemenko SA. Platelet-rich plasma therapy for male sexual dysfunction: myth or reality? Sex Med Rev. 2020;8:106–13.
Schirmann A, Boutin E, Faix A, Yiou R. Pilot study of intra-cavernous injections of platelet-rich plasma (P-shot®) in the treatment of vascular erectile dysfunction. Prog Urol. 2022;32:1440–5.
Zaghloul AS, Mahmoud ElNashar AER, GamalEl Din SF, Zaki Said S, Saad HM, Refaat Eldebs H, et al. Smoking status and the baseline international index of erectile function score can predict satisfactory response to platelet-rich plasma in patients with erectile dysfunction: a prospective pilot study. Andrologia. 2021;53:e14162.
Taş T, Çakıroğlu B, Arda E, Onuk Ö, Nuhoğlu B. Early clinical results of the tolerability, safety, and efficacy of autologous platelet-rich plasma administration in erectile dysfunction. Sex Med. 2021;9:100313.
Wong S-M, Chiang B-J, Chen H-C, Wu Y-N, Lin Y-H, Liao C-H. A short term follow up for intracavernosal injection of platelet rich plasma for the treatment of erectile dysfunction. Urol Sci. 2021;32:171.
Burnett AL, Nehra A, Breau RH, Culkin DJ, Faraday MM, Hakim LS, et al. Erectile dysfunction: AUA guideline. J Urol. 2018;200:633–41.
Scott S, Roberts M, Chung E. Platelet-rich plasma and treatment of erectile dysfunction: critical review of literature and global trends in platelet-rich plasma clinics. Sex Med Rev. 2019;7:306–12.
Israeli JM, Lokeshwar SD, Efimenko IV, Masterson TA, Ramasamy R. The potential of platelet-rich plasma injections and stem cell therapy for penile rejuvenation. Int J Impot Res. 2022;34:375–82. https://doi.org/10.1038/s41443-021-00482-z
Liu JL, Chu KY, Gabrielson AT, Wang R, Trost L, Broderick G, et al. Restorative therapies for erectile dysfunction: position statement from the Sexual Medicine Society of North America (SMSNA). Sex Med. 2021;9:100343.
Britt D, Blankstein U, Lenardis M, Millman A, Grober E, Krakowsky Y. Availability of platelet-rich plasma for treatment of erectile dysfunction and associated costs and efficacy: a review of current publications and Canadian data. Can Urol Assoc J. 2021;15:202–6.
Dohan Ehrenfest DM, Rasmusson L, Albrektsson T. Classification of platelet concentrates: from pure platelet-rich plasma (P-PRP) to leucocyte- and platelet-rich fibrin (L-PRF). Trends Biotechnol. 2009;27:158–67.
Author information
Authors and Affiliations
Contributions
AT: conceptualization and project administration; AP: methodology and formal analysis; AP, CL, FZ, RO and FLR: data curation; AP and AT: manuscript—original draft; AP, AT and RO.: manuscript—review & editing; ABP, FM, VP and AT; supervisions. All authors have read and approved the final version of this manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Panunzio, A., Labate, C., Zacheo, F. et al. Platelet-rich plasma intracavernosal injections for the treatment of primary organic erectile dysfunction: a systematic review and meta-analysis of contemporary controlled studies. Int J Impot Res (2023). https://doi.org/10.1038/s41443-023-00798-y
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41443-023-00798-y