Abstract
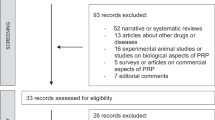
The significant discontinuation rate of available therapies and the paucity of curative options promoted the research on potential novel treatments suitable for erectile dysfunction patients. The aim of this study was to provide a summary of available evidence regarding the news and future perspectives related to the non-surgical treatment of erectile dysfunction. A narrative review of the literature was performed. A comprehensive search in the MEDLINE, Embase, and Scopus databases was done. Papers in English-language, published until April 2022, were included. No chronological restriction was applied. Retrospective and prospective clinical studies, as well as meta-analyses, were considered. Oro-dispersible formulations of phosphodiesterase type 5 inhibitors are particularly indicated in patients who have difficulty in swallowing solid dosage form; in addition, they constitute a discrete route of administration not requiring water. Low-intensity extracorporeal shock wave therapy is indicated in mild vasculogenic erectile dysfunction and in patients with vasculogenic erectile dysfunction poorly responsive to phosphodiesterase type 5 inhibitors. Stem cell therapy, platelet-rich plasma injections, and gene therapy seem promising regenerative treatments for selected patients with erectile dysfunction. Novel oral formulations of drugs commonly used in erectile dysfunction patients have recently become part of standard clinical practice. Regenerative treatments have been emerging in recent years and could become routine curative options in the near future. Further well-designed randomized controlled trials are needed to provide conclusive evidence on this topic and guide appropriate recommendations.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Change history
31 October 2022
A Correction to this paper has been published: https://doi.org/10.1038/s41443-022-00641-w
References
Salonia A, Bettocchi C, Carvalho J, Corona G, Jones TH, Kadioglu A, et al. European Association of Urology Guidelines on sexual and reproductive health. Presented at the EAU Annual Congress Amsterdam. 2022. ISBN 978-94-92671-16-5.
Atallah S, Haydar A, Jabbour T, Kfoury P, Sader G. The effectiveness of psychological interventions alone, or in combination with phosphodiesterase-5 inhibitors, for the treatment of erectile dysfunction: a systematic review. Arab J Urol. 2021;19:310–22.
Linet OI, Ogrinc FG. Efficacy and safety of intracavernosal alprostadil in men with erectile dysfunction. The Alprostadil Study Group. N Engl J Med. 1996;334:873–7.
Kim ED, McVary KT. Topical prostaglandin-E1 for the treatment of erectile dysfunction. J Urol. 1995;153:1828–30.
Arcaniolo D, Bellastella G, Manfredi C, Terribile M, Giordano DR, Quattrone C, et al. Is topical alprostadil an usable and reliable alternative to intracavernous injection for penile dynamic duplex ultrasonography? Andrologia. 2020;52:e13480.
Cookson MS, Nadig PW. Long-term results with vacuum constriction device. J Urol. 1993;149:290–4.
Howell S, Palasi S, Green T, Kannady C, Panuganti S, Slaughter K, et al. Comparison of satisfaction with penile prosthesis implantation in patients with radical prostatectomy or radical cystoprostatectomy to the general population. Sex Med. 2021;9:100300.
Manfredi C, Fortier E, Faix A, Martínez-Salamanca JI. Penile implant surgery satisfaction assessment. J Sex Med. 2021;18:868–74.
Moncada I, Martinez-Salamanca J, Ruiz-Castañe J, Romero-Otero J. Combination therapy for erectile dysfunction involving a PDE5 inhibitor and alprostadil. Int J Impot Res. 2018;30:203–8.
Mykoniatis I, Pyrgidis N, Sokolakis I, Ouranidis A, Sountoulides P. Assessment of combination therapies vs monotherapy for erectile dysfunction a systematic review and meta-analysis. JAMA Netw Open. 2021;4:1–17.
Garrido-Abad P, Senra-Bravo I, Manfredi C, Fernández-Pascual E, Linares-Espinós E, Fernández-Arjona M, et al. Combination therapy with topical alprostadil and phosphodiesterase-5 inhibitors after failure of oral therapy in patients with erectile dysfunction: a prospective, two-arm, open-label, non-randomized study. Int J Impot Res. 2022;34:164–71.
Williams P, McBain H, Amirova A, Newman S, Mulligan K. Men’s beliefs about treatment for erectile dysfunction-what influences treatment use? A systematic review. Int J Impot Res. 2021;33:16–42.
Carvalheira AA, Pereira NM, Maroco J, Forjaz V. Dropout in the treatment of erectile dysfunction with PDE5: a study on predictors and a qualitative analysis of reasons for discontinuation. J Sex Med. 2012;9:2361–9.
Kim SC, Lee YS, Seo KK, Jung GW, Kim TH. Reasons and predictive factors for discontinuation of PDE-5 inhibitors despite successful intercourse in erectile dysfunction patients. Int J Impot Res. 2014;26:87–93.
Corona G, Rastrelli G, Burri A, Serra E, Gianfrilli D, Mannucci E. First-generation phosphodiesterase type 5 inhibitors dropout: a comprehensive review and meta-analysis. Andrology. 2016;4:1002–9.
Lv Y, Luo BY, LaBadie RR, Zhu H, Feng Y, Ernst C, et al. Bioequivalence and bioavailability of an orodispersible tablet of sildenafil citrate in healthy chinese male subjects. Clin Pharm Drug Dev. 2020;9:573–81.
Ortac M, Özmez A, Cilesiz NC, Demirelli E, Kadıoğlu A. The impact of extracorporeal shock wave therapy for the treatment of young patients with vasculogenic mild erectile dysfunction: a prospective randomized single-blind, sham controlled study. Andrology. 2021;9:1571–8.
Bahk JY, Jung JH, Han H, Min SK, Lee YS. Treatment of diabetic impotence with umbilical cord blood stem cell intracavernosal transplant: preliminary report of 7 cases. Exp Clin Transpl. 2010;8:150–60.
Epifanova M, Chalyi M, Krasnov A. Investigation of mechanisms of action of growth factors of autologous platelet-rich plasma used to treat erectile dysfunction. Urologiia. 2017;4:46–8.
Corona G, Maggi M, Jannini EA. EDEUS, a real-life study on the users of phosphodiesterase type 5 inhibitors: prevalence, perceptions, and health care-seeking behavior among European men with a focus on 2nd-generation avanafil. Sex Med. 2018;6:15–23.
Rubio-Aurioles E, Porst H, Kim ED, Montorsi F, Hackett G, et al. A randomized open-label trial with a crossover comparison of sexual self-confdence and other treatment outcomes following tadalafl once a day vs. tadalafl or sildenafl on-demand in men with erectile dysfunction. J Sex Med. 2012;9:1418–29.
Taylor J, Baldo OB, Storey A, Cartledge J, Eardley I. Differences in side-efect duration and related bother levels between phosphodiesterase type 5 inhibitors. BJU Int. 2009;103:1392–5.
De Toni L, De Rocco Ponce M, Franceschinis E, Dall’Acqua S, Padrini R, Realdon N, et al. Sublingual administration of sildenafil oro-dispersible film: new profiles of drug tolerability and pharmacokinetics for PDE5 inhibitors. Front Pharm. 2018;9:59.
Radicioni M, Castiglioni C, Giori A, Cupone I, Frangione V, Rovati S. Bioequivalence study of a new sildenafil 100 mg orodispersible film compared to the conventional film-coated 100 mg tablet administered to healthy male volunteers. Drug Des Dev Ther. 2017;11:1183–92.
Loprete L, Leuratti C, Frangione V, Radicioni M. Pharmacokinetics of a novel sildenafil orodispersible film administered by the supralingual and the sublingual route to healthy men. Clin Drug Investig. 2018;38:765–72.
Pavone C, Abrate A, Agiato S, Billeci S, Tulone G, Vella M, et al. Sildenafil orodispersible film in the treatment of erectile dysfunction after radical prostatectomy: a single-centre open-label uncontrolled trial. Andrology. 2020;52:e13705.
Cocci A, Capece M, Cito G, Russo GI, Falcone M, Timpano M, et al. Effectiveness and safety of oro-dispersible sildenafil in a new film formulation for the treatment of erectile dysfunction: comparison between Sildenafil 100-mg film-coated tablet and 75-mg oro-dispersible film. J Sex Med. 2017;14:1606–11.
Wang AY, Podlasek C. Role of nanotechnology in erectile dysfunction treatment. J Sex Med. 2017;14:36–43.
Badr-eldin SM, Ahmed O. Optimized nano-transfersomal films for enhanced sildenafil citrate transdermal delivery: ex vivo and in vivo evaluation. Drug Des Dev Ther. 2016;10:1323–33.
Han G, Tar M, Kuppam D, Friedman A, Melman A, Friedman J, et al. Nanoparticles as a novel delivery vehicle for therapeutics targeting erectile dysfunction. J Sex Med. 2011;7:224–33.
Fahmy U. Nanoethosomal transdermal delivery of vardenafil for treatment of erectile dysfunction: optimization, characterization, and in vivo evaluation. Drug Des Dev Ther. 2015;9:6129–37.
Kurakula M, Ahmed OAA, Fahmy UA, Ahmed TA, Kurakula M, Ahmed OAA, et al. Solid lipid nanoparticles for transdermal delivery of avanafil: optimization, formulation, in-vitro and ex-vivo studies solid lipid nanoparticles for transdermal delivery of avanafil: optimization, formulation, in-vitro and ex-vivo studies. J Liposome Res. 2016;26:288–96.
Masuku NP, Unuofin JO, Lebelo SL. Advances in nanoparticle delivery system for erectile dysfunction: an updated review. Sex Med. 2021;9:100420.
Srivatsav A, Balasubramanian A, Pathak UI, Rivera-Mirabal J, Thirumavalavan N, Hotaling JM, et al. Efficacy and safety of common ingredients in aphrodisiacs used for erectile dysfunction: a review. Sex Med Rev. 2020;8:431–42.
Leisegang K, Finelli F. Alternative medicine and herbal remedies in the treatment of erectile dysfunction: a systematic review. Arab J Urol. 2021;19:323–39.
Mirone V, Napolitano L, D’Emmanuele di Villa Bianca R, Mitidieri E, Sorrentino R, Vanelli A, et al. A new original nutraceutical formulation ameliorates the effect of Tadalafil on clinical score and cGMP accumulation. Arch Ital Urol Androl. 2021;93:221–6.
Zenico T, Cicero AF, Valmorri L, Mercuriali M, Bercovich E. Subjective effects of Lepidium meyenii (Maca) extract on well-being and sexual performances in patients with mild erectile dysfunction: a randomised, double-blind clinical trial. Andrologia. 2009;41:95–9.
Shamsa A, Hosseinzadeh H, Molaei M, Shakeri MT, Rajabi O. Evaluation of Crocus sativus L. (saffron) on male erectile dysfunction: a pilot study. Phytomedicine. 2009;16:690–3.
Stanislavov R, Nikolova V. Treatment of erectile dysfunction with pycnogenol and L-arginine. J Sex Marital Ther. 2003;29:207–13.
Cormio L, De Siati M, Lorusso F, Selvaggio O, Mirabella L, Sanguedolce F, et al. Oral L-citrulline supplementation improves erection hardness in men with mild erectile dysfunction. Urology. 2011;77:119–22.
GamalEl Din SF, Abdel Salam MA, Mohamed MS, Ahmed AR, Motawaa AT, Saadeldin OA, et al. Tribulus terrestris versus placebo in the treatment of erectile dysfunction and lower urinary tract symptoms in patients with late-onset hypogonadism: a placebo-controlled study. Urologia. 2019;86:74–8.
Shindel AW, Xin ZC, Lin G, Fandel TM, Huang YC, Banie L, et al. Erectogenic and neurotrophic effects of icariin, a purified extract of horny goat weed (Epimedium spp.) in vitro and in vivo. J Sex Med. 2010;7:1518–28.
Ferrini MG, Garcia E, Abraham A, Artaza JN, Nguyen S, Rajfer J. Effect of ginger, Paullinia cupana, muira puama and l- citrulline, singly or in combination, on modulation of the inducible nitric oxide- NO-cGMP pathway in rat penile smooth muscle cells. Nitric Oxide. 2018;76:81–86.
Sohn M, Sikora R. Ginkgo biloba extract in the therapy of erectile dysfunction. J Sex Educ Ther. 1991;17:53–61.
Vardi Y, Appel B, Jacob G, Massarwi O, Gruenwald I. Can low-intensity extracorporeal shockwave therapy improve erectile function? A 6-month follow-up pilot study in patients with organic erectile dysfunction. Eur Urol. 2010;58:243–8.
Liu T, Shindel A, Lin G, Lue T. Cellular signaling pathways modulated by low-intensity extracorporeal shock wave therapy. Int J Impot Res. 2019;31:170–6.
Scroppo FI, Pezzoni F, Gaeta F, Pastore LA, Malfatto M, Cai T, et al. Li-Eswt improves hemodynamic parameters thus suggesting neoangiogenesis in patients with vascular erectile dysfunction. Int J Impot Res. 2022;34:237–42.
Sokolakis I, Dimitriadis F, Teo P, Hatzichristodoulou G, Hatzichristou D, Giuliano F. The basic science behind low-intensity extracorporeal shockwave therapy for erectile dysfunction: a systematic scoping review of pre-clinical studies. J Sex Med. 2019;16:168–94.
Capogrosso P, Frey A, Jensen CFS, Rastrelli G, Russo GI, Torremade J, et al. Low-intensity shock wave therapy in sexual medicine—clinical recommendations from the European Society of Sexual Medicine (ESSM). J Sex Med. 2019;16:1490–505.
Ghahhari J, De Nunzio C, Lombardo R, Ferrari R, Gatti L, Ghidini N, et al. Shockwave therapy for erectile dysfunction: which gives the best results? A retrospective national, multi-institutional comparative study of different shockwave technologies. Surg Technol Int. 2022;40:213–8.
Campbell JD, Trock BJ, Oppenheim AR, Anusionwu I, Gor RA, Burnett AL. Meta-analysis of randomized controlled trials that assess the efficacy of low-intensity shockwave therapy for the treatment of erectile dysfunction. Ther Adv Urol. 2019;11:1756287219838364.
Sokolakis I, Hatzichristodoulou G. Clinical studies on low intensity extracorporeal shockwave therapy for erectile dysfunction: a systematic review and meta-analysis of randomised controlled trials. Int J Impot Res. 2019;31:177–94.
Oliveira PS, De, Ziegelmann MJ. Low-intensity shock wave therapy for the treatment of vasculogenic erectile dysfunction: a narrative review of technical considerations and treatment outcomes. Transl Androl Urol. 2021;10:2617–28.
Rosen RC, Allen KR, Ni X, Araujo AB. Minimal clinically important differences in the erectile function domain of the international index of erectile function scale. Eur Urol. 2011;60:1010–6.
Lu Z, Lin G, Reed-Maldonado A, Wang C, Lee Y, Lue T. Low-intensity extracorporeal shock wave treatment improves erectile function: a systematic review and meta-analysis. Eur Urol. 2017;71:223–33.
Libo M, Guizhong L. Low-intensity extracorporeal shock wave therapy for erectile dysfunction: a systematic review and meta-analysis. Urology. 2018;119:97–103.
Taş T, Çakıroğlu B, Arda E, Onuk Ö, Nuhoğlu B. Early clinical results of the tolerability, safety, and efficacy of autologous platelet-rich plasma administration in erectile dysfunction. Sex Med. 2021;9:100313.
Chalyj ME, Grigorjan VA, Epifanova MV, Krasnov AO. [The effectiveness of intracavernous autologous platelet-rich plasma in the treatment of erectile dysfunction]. Urologiia. 2015;76-9.
Matz EL, Pearlman AM, Terlecki RP. Safety and feasibility of platelet rich fibrin matrix injections for treatment of common urologic conditions. Investig Clin Urol. 2018;59:61–5.
Towe M, Peta A, Saltzman RG. The use of combination regenerative therapies for erectile dysfunction: rationale and current status. Int J Impot Res. 2021:18–21.
Geyik S. Comparison of the efficacy of low-intensity shock wave therapy and its combination with platelet-rich plasma in patients with erectile dysfunction. Andrologia. 2021;00:e14197.
Poulios E, Mykoniatis I, Pyrgidis N, Zilotis F, Kapoteli P, Kotsiris D, et al. Platelet-rich plasma (PRP) improves erectile function: a double-blind, randomized, placebo-controlled clinical trial. J Sex Med. 2021;18:926–35.
Alkandari MH, Touma N, Carrier S. Platelet-rich plasma injections for erectile dysfunction and Peyronie’s disease: a systematic review of evidence. Sex Med Rev. 2022;10:341–52.
Soebadi MA, Milenkovic U, Weyne E, Castiglione F, Albersen M. Stem cells in male sexual dysfunction: are we getting somewhere? Sex Med Rev. 2017;5:222–35.
Milenkovic U, Albersen M, Castiglione F. The mechanisms and potential of stem cell therapy for penile fibrosis. Nat Rev Urol. 2019;16:79–97.
You D, Jang MJ, Kim BH, Song G, Lee C, Suh N, et al. Comparative study of autologous stromal vascular fraction and adipose-derived stem cells for erectile function recovery in a rat model of cavernous nerve injury. Stem Cells Transl Med. 2015;4:351–8.
Baghaei K, Hashemi SM, Tokhanbigli S, Asadi Rad A, Assadzadeh-Aghdaei H, Sharifian A, et al. Isolation, differentiation, and characterization of mesenchymal stem cells from human bone marrow. Gastroenterol Hepatol Bed Bench. 2017;10:208–13.
Matz EL, Terlecki RP. Stem cell and gene-based therapy for erectile dysfunction current status and future needs. Urol Clin North Am. 2022;48:611–9.
Levy J, MArchand M, Iorio L, Cassini W, Zahalsky M. Determining the feasibility of managing erectile dysfunction in humans with placental-derived stem cells. J Am Osteopath Assoc. 2016;116:1–5.
Mirzaei M, Bagherinasabsarab M, Pakmanesh H, Mohammadi R, Teimourian M, Farsinejad A, et al. The effect of intracavernosal injection of stem cell in the treatment of erectile dysfunction in diabetic patients; a randomized single-blinded clinical trial. Urol J. 2021;18:675–81.
Haahr MK, Harken C, Mohamadpour N, Caroline D, Damkier P, Ahm J, et al. Safety and potential effect of a single intracavernous injection of autologous adipose-derived regenerative cells in patients with erectile dysfunction following radical prostatectomy: an open-label phase I clinical trial. EBioMedicine. 2016;5:204–10.
Yiou R, Hamidou L, Birebent B, Bitari D, Le Corvoisier P, Contremoulins I, et al. Intracavernous injections of bone marrow mononucleated cells for postradical prostatectomy erectile dysfunction: final results of the INSTIN clinical trial. Eur Urol Focus. 2017;3:643–5.
Andersson K, Christ GJ. Gene therapy in erectile dysfunction: dead or alive? J Sex Med. 2020;17:1587–89.
Magee TR, Ferrini M, Garban HJ, Vernet D, Mitani K, Rajfer J, et al. Gene therapy of erectile dysfunction in the rat with penile neuronal nitric oxide synthase. Biol Reprod. 2002;67:1033–41.
Melman A, Bar-chama N, Cullough AMC, Davies K, Christ G. hMaxi-K gene transfer in males with erectile dysfunction: results of the first human trial. Hum Gene Ther. 2006;1176:1165–76.
Acknowledgements
Non-conditioning support of IBSA Institut Biochimique SA (Switzerland).
Author information
Authors and Affiliations
Consortia
Contributions
CM drafting the manuscript; FC choice of topics and supervision; MF, MLS, CB, and JRO scientific and grammatical correction; GC critical review and final approval of the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The original version of this article unfortunately contained a mistake. The acknowledgements note was incorrect; the correct acknowledgements note is given below. Acknowledgements Non-conditioning support of IBSA Institut Biochimique SA (Switzerland). The original article has been corrected.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Manfredi, C., Castiglione, F., Fode, M. et al. News and future perspectives of non-surgical treatments for erectile dysfunction. Int J Impot Res 35, 699–705 (2023). https://doi.org/10.1038/s41443-022-00602-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41443-022-00602-3