Abstract
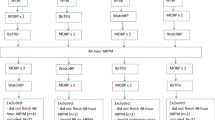
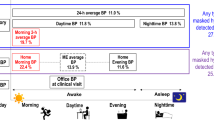
To practice standardized office blood pressure (OBP) measurement guidelines pragmatically, we developed an intelligent assisted OBP (IOBP) measurement system in the Chinese community, which can automatically obtain two or three BP values after a 5-min rest before the patients visit the doctor and transfer values to the community medical network in real time. We conducted a comparative study to investigate the agreement among IOBP, awake ambulatory BP (ABP), and conventional auscultatory OBP at different BP levels. Participants were divided into three groups according to BP, with 120/80 mmHg and 160/100 mmHg as the cut-off points. Attended IOBP, unattended IOBP, and auscultatory OBP were randomly measured before ABP monitoring. In total, 245 participants were included in the analysis. The mean systolic attended/unattended IOBP, auscultatory OBP, and awake ABP were 135.0, 136.7, 135.6, and 136.2 mmHg, respectively. Bland-Altman analysis revealed a bias of −1.1 and 0.5 mmHg for systolic attended/unattended IOBP compared with awake ABP in the overall sample. For auscultatory OBP, the bias was −0.4 (attended) and 1.2 mmHg (unattended). The discrepancy between the systolic attended/unattended IOBP and awake ABP was inconsistent at different BP levels. In Group 1 the values were −8.4 and −6.9 mmHg, whereas in Group 3, the values were 9.4 and 10.0 mmHg. BP measured using the IOBP measurement system was in accordance with awake ABP and conventional OBP, and can be a good choice in the Chinese community.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Wang Z, Chen Z, Zhang L, Wang X, Hao G, Zhang Z, et al. Status of hypertension in China: results from the China Hypertension Survey, 2012-2015. Circulation. 2018;137:2344–56.
Mancia Chairperson G, Kreutz Co-Chair R, Brunström M, Burnier M, Grassi G, Januszewicz A, et al. ESH Guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Hypertension Endorsed by the European Renal Association (ERA) and the International Society of Hypertension (ISH). J Hypertens. (2023; 20230621;https://doi.org/10.1097/hjh.0000000000003480).
Rabi DM, McBrien KA, Sapir-Pichhadze R, Nakhla M, Ahmed SB, Dumanski SM, et al. Hypertension Canada’s 2020 comprehensive guidelines for the prevention, diagnosis, risk assessment, and treatment of hypertension in adults and children. Can J Cardiol. 2020;36:596–624.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of cardiology/american heart association task force on clinical practice Guidelines. Circulation 2018;138:e426–83.
Alpert B, McCrindle B, Daniels S, Dennison B, Hayman L, Jacobson M, et al. Recommendations for blood pressure measurement in human and experimental animals; part 1: blood pressure measurement in humans. Hypertension. 2006;48:e3.
Flack JM, Adekola B. Blood pressure and the new ACC/AHA hypertension guidelines. Trends Cardiovasc Med. 2020;30:160–4.
Cheung AK, Whelton PK, Muntner P, Schutte AE, Moran AE, Williams B, et al. International consensus on standardized clinic blood pressure measurement - A Call to Action. Am J Med. 2023;136:438–445.e431.
Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, et al. 2020 international society of hypertension global hypertension practice guidelines. J Hypertens. 2020;38:982–1004.
Hwang KO, Aigbe A, Ju HH, Jackson VC, Sedlock EW. Barriers to accurate blood pressure measurement in the medical office. J Prim Care Community Health. 2018;9:2150132718816929.
Myers MG, Godwin M, Dawes M, Kiss A, Tobe SW, Kaczorowski J. Measurement of blood pressure in the office: recognizing the problem and proposing the solution. Hypertension. 2010;55:195–200.
Foti KE, Appel LJ, Matsushita K, Coresh J, Alexander GC, Selvin E. Digit preference in office blood pressure measurements, United States 2015-2019. Am J Hypertens. 2021;34:521–30.
Nietert PJ, Wessell AM, Feifer C, Ornstein SM. Effect of terminal digit preference on blood pressure measurement and treatment in primary care. Am J Hypertens. 2006;19:147–52.
Wang Y, Wang Y, Qain Y, Zhang J, Tang X, Sun J, et al. Longitudinal change in end-digit preference in blood pressure recordings of patients with hypertension in primary care clinics: Minhang study. Blood Press Monit. 2015;20:74–78.
Wang Y, Chen L, Fu C, Wang Y, An D, Zhang J, et al. Associations between various attended automated office blood pressure estimations and all-cause and cardiovascular mortality: Minhang study. J Hypertens. 2020;38:1072–9.
Devereux RBRW. Echocardiographic determination of left ventricular mass in man anatomic validation of the method. Circulation. 1977;55:613–8.
Andreadis EA, Geladari CV, Angelopoulos ET, Savva FS, Georgantoni AI, Papademetriou V. Attended and unattended automated office blood pressure measurements have better agreement with ambulatory monitoring than conventional office readings. J Am Heart Assoc. 2018;7:e008994.
Edwards C, Hiremath S, Gupta A, McCormick BB, Ruzicka M. BpTRUth: do automated blood pressure monitors outperform mercury? J Am Soc Hypertens. 2013;7:448–53.
Myers MG, Valdivieso M, Kiss A. Use of automated office blood pressure measurement to reduce the white coat response. J Hypertens. 2009;27:280–6.
Myers MG, Valdivieso M, Kiss A. Consistent relationship between automated office blood pressure recorded in different settings. Blood Press Monit. 2009;14:108–11.
Rinfret F, Cloutier L, Wistaff R, Birnbaum LM, Ng Cheong N, Laskine M, et al. Comparison of different automated office blood pressure measurement devices: evidence of nonequivalence and clinical implications. Can J Cardiol. 2017;33:1639–44.
Benavente OR, Coffey CS, Conwit R, Hart RG, McClure LA, Pearce LA, et al. Blood-pressure targets in patients with recent lacunar stroke: the SPS3 randomised trial. Lancet. 2013;382:507–15.
Cushman WC, Evans GW, Byington RP, Goff DC Jr, Grimm RH Jr, Cutler JA, et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N. Engl J Med. 2010;362:1575–85.
Wright JT Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, Rocco MV, et al. A randomized trial of intensive versus standard blood-pressure control. N. Engl J Med. 2015;373:2103–16.
Drawz PE, Pajewski NM, Bates JT, Bello NA, Cushman WC, Dwyer JP, et al. Effect of intensive versus standard clinic-based hypertension management on ambulatory blood pressure: results from the SPRINT (Systolic Blood Pressure Intervention Trial) ambulatory blood pressure study. Hypertension. 2017;69:42–50.
Andreadis EA, Geladari CV, Angelopoulos ET. Automated office blood pressure is in agreement with awake and mean 24-hour ambulatory blood pressure at the lower blood pressure range. J Clin Hypertens. 2020;22:1177–83.
Parati G, Ochoa JE, Bilo G, Zanchetti A. SPRINT blood pressure: sprinting back to Smirk’s basal blood pressure? Hypertension. 2017;69:15–19.
Mancia G, Sega R, Bravi C, De Vito G, Valagussa F, Cesana G, et al. Ambulatory blood pressure normality: results from the PAMELA study. J Hypertens. 1995;13:1377–90.
Mancia G, Facchetti R, Parati G, Zanchetti A. Effect of long-term antihypertensive treatment on white-coat hypertension. Hypertension. 2014;64:1388–98.
Mizuno H, Hoshide S, Yano Y, Nozue R, Kario K. Comparison of brachial blood pressure and central blood pressure in attended, unattended, and unattended standing situations. Hypertens Res. 2021;44:1283–90.
Roerecke M, Kaczorowski J, Myers MG. Comparing automated office blood pressure readings with other methods of blood pressure measurement for identifying patients with possible hypertension: a systematic review and meta-analysis. JAMA Intern Med. 2019;179:351–62.
Stergiou GS, Alpert B, Mieke S, Asmar R, Atkins N, Eckert S, et al. A Universal Standard for the Validation of Blood Pressure Measuring Devices: Association for the Advancement of Medical Instrumentation/European Society of Hypertension/International Organization for Standardization (AAMI/ESH/ISO) Collaboration Statement. Hypertension. 2018;71:368–74.
Bliziotis IA, Destounis A, Stergiou GS. Home versus ambulatory and office blood pressure in predicting target organ damage in hypertension: a systematic review and meta-analysis. J Hypertens. 2012;30:1289–99.
Kollias A, Lagou S, Zeniodi ME, Boubouchairopoulou N, Stergiou GS. Association of central versus brachial blood pressure with target-organ damage: systematic review and meta-analysis. Hypertension. 2016;67:183–90.
Martínez MA, Sancho T, García P, Moreno P, Rubio JM, Palau FJ, et al. Home blood pressure in poorly controlled hypertension: relationship with ambulatory blood pressure and organ damage. Blood Press Monit. 2006;11:207–13.
Acknowledgements
JM, XT, and JZ analyzed the data from this study and were responsible for writing the article. YW, MC, and DZ were responsible for the design of this study and critical revision. We also gratefully acknowledge the technical assistance of QW. All the authors critically reviewed and approved the final paper.
Funding
This project was supported by grants from National Research Center for Translational Medicine (Shanghai) grant NRCTM(SH)-2021-05, the National Natural Science Foundation of China (81370205 and 81670213), Shanghai Municipal Health Bureau Foundation (201640243). The funders had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ma, J., Tang, X., Zhao, J. et al. Intelligent Assist Office Blood Pressures (IOBP) versus awake ambulatory monitoring and conventional auscultatory office readings in Chinese primary medical institutions. Hypertens Res (2024). https://doi.org/10.1038/s41440-024-01687-7
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41440-024-01687-7