Abstract
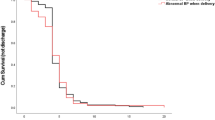
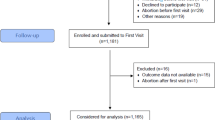
Our study aimed to investigate the clinical features of recurrent preeclampsia (rPE) and evaluate the preventive effect of low-dose aspirin (LDA) in rPE. We retrospectively analyzed the data of 109 patients who experienced preeclampsia in two consecutive pregnancies and delivered at Peking University First Hospital from January 2016 to December 2022. We analyzed the pregnancy outcomes of patients with rPE and assessed whether the use of LDA during pregnancy could improve these outcomes. Our results revealed that patients with rPE had a higher body mass index (BMI) and a higher incidence of diabetes during pregnancy compared to their first onset of preeclampsia (29.01 ± 4.70 kg/m2 vs. 27.13 ± 4.25 kg/m2, P < 0.05; 11.01% vs. 1.83%, P < 0.05). Furthermore, the incidence of severe preeclampsia was higher at recurrence in patients with rPE compared to their first onset (83.49% vs. 70.64%, P < 0.05), as well as the incidence of severe preeclampsia with chronic hypertension (34.86% vs. 8.26%, P < 0.05). Additionally, the incidence of gestational diabetes and postpartum hemorrhage was higher in patients with rPE compared to their first preeclampsia onset (25.69% vs. 5.50%, P < 0.05; 20.18% vs. 5.83%, P < 0.05). Compared to the first onset of preeclampsia, patients with rPE had an earlier gestational age at delivery (35.42 ± 3.06 weeks vs. 36.60 ± 2.74 weeks, P < 0.05), lower birth weight of neonates (2478.39 ± 828.44 g vs. 2883.71 ± 712.94 g, P < 0.05), and a higher risk of premature birth (67.00% vs. 47.19%, P < 0.05). However, in patients with rPE, the use of LDA delayed the gestational age at delivery, increased the birth weight of the neonate, reduced the premature birth rate, and increased the perinatal survival rate. In conclusion, patients with rPE are at an increased risk of adverse maternal and fetal outcomes. However, the use of LDA during pregnancy effectively improves these outcomes.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
American College of Obstetricians and Gynecologists. Practice Bulletin No 202. Gestational hypertension and preeclampsia. Obstet Gynecol. 2019;133:1.
Chen Y-Y, Wu M-L, Kao M-H, Su T-H, Chen C-P. Perinatal outcome of recurrent pre-eclampsia versus pre-eclampsia in nulliparas. J Obstet Gynaecol Res. 2009;35:1042–6.
Hnat MD, Sibai BM, Caritis S, Hauth J, Lindheimer MD, MacPherson C, et al. Perinatal outcome in women with recurrent preeclampsia compared with women who develop preeclampsia as nulliparas. Am J Obstet Gynecol. 2002;186:422–6.
Wikström A-K, Stephansson O, Cnattingius S. Previous preeclampsia and risks of adverse outcomes in subsequent nonpreeclamptic pregnancies. Am J Obstet Gynecol. 2011;204:148.e1–6.
LeFevre ML.U.S. Preventive Services Task Force Low-dose aspirin use for the prevention of morbidity and mortality from preeclampsia: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2014;161:819–26.
American College of Obstetricians and Gynecologists. Practice Bulletin No.134:Fetal Growth Restriction. Obstet Gynecol. 2013;121:1122–33.
American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2014;37:S81–90.
Stagnaro-Green A, Abalovich M, Alexander E, Azizi F, Mestman J, Negro R, et al. Guidelines of the American Thyroid Association for the diagnosis and management of thyroid disease during pregnancy and postpartum. Thyroid. 2011;21:1081–125.
He Y, Li Z, Chen S, Lv J, Zhao M, Chen Q. Pregnancy in patients with stage 3-5 CKD: Maternal and fetal outcomes. Pregnancy Hypertens. 2022;29:86–91.
Fanouriakis A, Tziolos N, Bertsias G, Boumpas DT. Update οn the diagnosis and management of systemic lupus erythematosus. Ann Rheum Dis. 2021;80:14–25.
Barbhaiya M, Zuily S, Naden R, Hendry A, Manneville F, Amigo M-C, et al. 2023 ACR/EULAR antiphospholipid syndrome classification criteria. Ann Rheum Dis. 2023;82:1258–70.
Van Rijn BB, Hoeks LB, Bots ML, Franx A, Bruinse HW. Outcomes of subsequent pregnancy after first pregnancy with early-onset preeclampsia. Am J Obstet Gynecol. 2006;195:723–8.
Melamed N, Hadar E, Peled Y, Hod M, Wiznitzer A, Yogev Y. Risk for recurrence of preeclampsia and outcome of subsequent pregnancy in women with preeclampsia in their first pregnancy. J Matern Fetal Neonatal Med. 2012;25:2248–51.
Wu P, Haththotuwa R, Kwok CS, Babu A, Kotronias RA, Rushton C, et al. Preeclampsia and future cardiovascular health: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2017;10:e003497.
Ponticelli C, Moroni G. Is preeclampsia a risk for end-stage renal disease? Kidney Int. 2019;96:547–9.
Garovic VD, White WM, Vaughan L, Saiki M, Parashuram S, Garcia-Valencia O, et al. Incidence and long-term outcomes of hypertensive disorders of pregnancy. J Am Coll Cardiol. 2020;75:2323–34.
American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins—Obstetrics. ACOG Practice Bulletin No. 203: chronic hypertension in pregnancy. Obstet Gynecol. 2019;133:e26–50.
Bramham K, Parnell B, Nelson-Piercy C, Seed PT, Poston L, Chappell LC. Chronic hypertension and pregnancy outcomes: systematic review and meta-analysis. BMJ. 2014;348:g2301.
Casagrande L, Rezende GP, Guida JP, Costa RS, Parpinelli MA, Surita FG, et al. Maternal and perinatal outcomes related to superimposed pre‐eclampsia in a Brazilian cohort of women with chronic hypertension. Int J Gynecol Obstet. 2020;149:148–53.
Boriboonhirunsarn D, Pradyachaipimol A, Viriyapak B. Incidence of superimposed preeclampsia among pregnant Asian women with chronic hypertension. Hypertens Pregnancy. 2017;36:226–31.
American College of Obstetricians and Gynecologists. Task Force on Hypertension in pregnancy. Hypertension in Pregnancy. Report of the American College of Obstetricians and Gynecologists’ Task Force on Hypertension in pregnancy. Obstet Gynecol. 2013;122:1122–31.
Brown MC, Best KE, Pearce MS, Waugh J, Robson SC, Bell R. Cardiovascular disease risk in women with pre-eclampsia: systematic review and meta-analysis. Eur J Epidemiol. 2013;28:1–19.
Dukler D, Porath A, Bashiri A, Erez O, Mazor M. Remote prognosis of primiparous women with preeclampsia. Eur J Obstet Gynecol Reprod Biol. 2001;96:69–74.
Weissgerber TL, Mudd LM. Preeclampsia and diabetes. Curr Diab Rep. 2015;15:9.
Lee J, Ouh Y-T, Ahn KH, Hong SC, Oh M-J, Kim H-J, et al. Preeclampsia: a risk factor for gestational diabetes mellitus in subsequent pregnancy. PLoS ONE. 2017;12:e0178150.
Mostello D, Jen Chang J, Allen J, Luehr L, Shyken J, Leet T. Recurrent preeclampsia: the effect of weight change between pregnancies. Obstet Gynecol. 2010;116:667–72.
Brown MA, Magee LA, Kenny LC, Karumanchi SA, McCarthy FP, Saito S. International Society for the Study of Hypertension in Pregnancy (ISSHP) et al. Hypertensive disorders of pregnancy: ISSHP classification, diagnosis, and management recommendations for international practice. Hypertension. 2018;72:24–43.
Takagi K, Makamoto O, Watanabe K, Tanaka K, Matsubara K, Kawabata I, et al. A review of the Best Practice Guide 2021 for the diagnosis and management of hypertensive disorders of pregnancy (HDP). Hypertens Res Pregnancy. 2022;10:57–73.
Rolnik DL, Wright D, Poon LC, O’Gorman N, Syngelaki A, De Paco Matallana C, et al. Aspirin versus placebo in pregnancies at high risk for preterm preeclampsia. N Engl J Med. 2017;377:613–22.
Choi YJ, Shin S. Aspirin prophylaxis during pregnancy: a systematic review and meta-analysis. Am J Prev Med. 2021;61:e31–45.
Bokuda K, Ichihara A. Preeclampsia up to date-what’s going on? Hypertens Res. 2023;46:1900–7.
Richards EMF, Giorgione V, Stevens O, Thilaganathan B. Low-dose aspirin for the prevention of superimposed preeclampsia in women with chronic hypertension: a systematic review and meta-analysis. Am J Obstet Gynecol. 2023;228:395–408.
Acknowledgements
The authors thank Dr. Yu Sun for her assistance with this study. Hui Zhang (co-first author).
Funding
This work was supported by National Key Research and Development Program of China (2022YFC2704700) and National Natural Science Foundation of China (No. 82071668).
Author information
Authors and Affiliations
Contributions
Data curation: Shujie Han, Hui Zhang; funding acquisition: Yingdong He; investigation: Shujie Han, Hui Zhang, and Yingdong He; methodology: Yingdong He; resources: Yingdong He, Qian Chen; and supervision: Yingdong He, Qian Chen. All the authors have read the manuscript and approved this submission.
Corresponding author
Ethics declarations
Ethical approval and statement of patient consent
This retrospective study was approved and monitored by the Institutional Review Board of Peking University Health Science Centre. The data were anonymous, and the requirement for informed consent was therefore waived.
Consent for publication
As this study was a retrospective analysis, formal consent was not required. All the authors of the manuscript agreed to its publication.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Han, S., Zhang, H., He, Y. et al. Clinical features of recurrent preeclampsia: a retrospective study of 109 recurrent preeclampsia patients. Hypertens Res 47, 1410–1419 (2024). https://doi.org/10.1038/s41440-024-01623-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-024-01623-9