Abstract
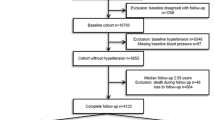
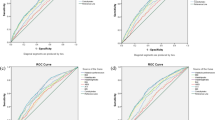
No existing reports demonstrate the association between anthropometric indices (body mass index, waist circumference, body roundness index, a body shape index) and hypertension according to sex and age in the general Japanese population. This retrospective analysis involved individuals aged 30–69 years who underwent annual medical checkups at Kagoshima Koseiren Hospital in 2005–2019, and who did not meet hypertension criteria at baseline. The outcome was hypertension incidence after 5 years, and its association with baseline anthropometric indices was evaluated using multivariable logistic regression analysis by sex and age. In 41,902 participants (age 52.3 ± 10.2 years, 47.7% men), 7622 individuals (18.2%) developed hypertension after 5 years. Body mass index, waist circumference, and body roundness index were significantly associated with the development of hypertension in both men and women across all age categories from 30 s to 60 s. In the population with a body mass index <25 kg/m2, waist circumference and body roundness index were significantly associated with hypertension after 5 years. A body shape index was significantly associated with the development of hypertension in men in their 40 s and 50 s but not in women of any age group. The area under the curve values were lower for a body shape index than for body mass index, waist circumference, and body roundness index in both men and women of all age groups. A body shape index was not a stronger indicator for 5-year hypertension incidence than body mass index, waist circumference, or body roundness index in both men and women across age groups from their 30s–60 s. The results of this study will help to more efficiently identify populations at high risk of developing hypertension and provide preventive interventions.

A total of 41,902 participants from health checkup programs were stratified by gender and age to investigate the association between baseline anthropometric indices and hypertension incidence over a 5-year period. BMI, WC, and BRI were almost equally effective and showed a better association with risk of developing hypertension in women and young adults compared to men and old adults. Conversely, ABSI showed no greater association than BMI or WC in any age group in both men and women. ABSI, a body shape index; AUC, area under the curve from receiver operating characteristic curve analysis; BMI, body mass index; BRI, body roundness index; WC, waist circumference.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The deidentified data of participants will not be shared.
References
Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2016;134:441–50.
GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1223–49.
Ikeda N, Inoue M, Iso H, Ikeda S, Satoh T, Noda M, et al. Adult mortality attributable to preventable risk factors for non-communicable diseases and injuries in Japan: a comparative risk assessment. PLOS Med. 2012;9:e1001160.
Nakamura K, Okamura T, Kanda H, Hayakawa T, Kadowaki T, Okayama A, et al. Impact of hypertension on medical economics: a 10-year follow-up study of national health insurance in Shiga, Japan. Hypertens Res. 2005;28:859–64.
Patel P, Ordunez P, DiPette D, Escobar MC, Hassell T, Wyss F, et al. Improved blood pressure control to reduce cardiovascular disease morbidity and mortality: the standardized hypertension treatment and prevention project. Rev Panam Salud Publica. 2017;41:1.
Vooradi S, Mateti UV. A systemic review on lifestyle interventions to reduce blood pressure. J Health Res Rev. 2016;3:1–5.
Krauss RM, Winston M, Fletcher BJ, Grundy SM. Obesity: impact on cardiovascular disease. Circulation. 1998;98:1472–6.
Rao G, Powell-Wiley TM, Ancheta I, Hairston K, Kirley K, Lear SA, et al. Identification of obesity and cardiovascular risk in ethnically and racially diverse populations: a scientific statement from the American Heart Association. Circulation. 2015;132:457–72.
Krakauer NY, Krakauer JC. A new body shape index predicts mortality hazard independently of body mass index. PLOS ONE. 2012;7:e39504.
Thomas DM, Bredlau C, Bosy-Westphal A, Mueller M, Shen W, Gallagher D, et al. Relationships between body roundness with body fat and visceral adipose tissue emerging from a new geometrical model. Obes (Silver Spring). 2013;21:2264–71.
Xu J, Zhang L, Wu Q, Zhou Y, Jin Z, Li Z, et al. Body roundness index is a superior indicator to associate with the cardio‐metabolic risk: evidence from a cross‐sectional study with 17,000 Eastern-China adults. BMC Cardiovasc Disord. 2021;21:97.
Kawasoe M, Kawasoe S, Kubozono T, Ojima S, Kawabata T, Ikeda Y, et al. Development of a risk prediction score for hypertension incidence using Japanese health checkup data. Hypertens Res. 2022;45:730–40.
Matsuzawa Y, Definition and the diagnostic standard for metabolic syndrome–Committee to Evaluate Diagnostic Standards for Metabolic Syndrome. Nihon Naika Gakkai Zasshi. 2005; 94: 794–809.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: the Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36:1953–2041.
Hall JE, do Carmo JM, da Silva AA, Wang Z, Hall ME. Obesity-induced hypertension: interaction of neurohumoral and renal mechanisms. Circ Res. 2015;116:991–1006.
Appel LJ, Brands MW, Daniels SR, Karanja N, Elmer PJ, Sacks FM, et al. Dietary approaches to prevent and treat hypertension: a scientific statement from the American Heart Association. Hypertension. 2006;47:296–308.
Neter JE, Stam BE, Kok FJ, Grobbee DE, Geleijnse JM. Influence of weight reduction on blood pressure: a meta-analysis of randomized controlled trials. Hypertension. 2003;42:878–84.
Channanath AM, Farran B, Behbehani K, Thanaraj TA. Association between body mass index and onset of hypertension in men and women with and without diabetes: a cross-sectional study using national health data from the State of Kuwait in the Arabian Peninsula. BMJ Open. 2015;5:e007043.
Nevill AM, Stewart AD, Olds T, Holder R. Relationship between adiposity and body size reveals limitations of BMI. Am J Phys Anthropol. 2006;129:151–6.
Li C, Ford ES, McGuire LC, Mokdad AH. Increasing trends in waist circumference and abdominal obesity among US adults. Obes (Silver Spring). 2007;15:216–24.
Bosomworth NJ. Normal-weight central obesity: unique hazard of the toxic waist. Can Fam Physician. 2019;65:399–408.
Camhi SM, Bray GA, Bouchard C, Greenway FL, Johnson WD, Newton RL, et al. The relationship of waist circumference and BMI to visceral, subcutaneous, and total body fat: sex and race differences. Obes (Silver Spring). 2011;19:402–8.
Cheng C, Sun JY, Zhou Y, Xie QY, Wang LY, Kong XQ, et al. High waist circumference is a risk factor for hypertension in normal-weight or overweight individuals with normal metabolic profiles. J Clin Hypertens (Greenwich). 2022;24:908–17.
Ashwell M, Gunn P, Gibson S. Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: systematic review and meta-analysis. Obes Rev. 2012;13:275–86.
Deng G, Yin L, Liu W, Liu X, Xiang Q, Qian Z, et al. Associations of anthropometric adiposity indexes with hypertension risk: A systematic review and meta-analysis including PURE-China. Medicine. 2018;97:e13262.
Chang Y, Guo X, Guo L, Li Z, Li Y, Sun Y. The feasibility of two new anthropometric indices to identify hypertension in rural China: a cross-sectional study. Med (Balt). 2016;95:e5301.
Ji M, Zhang S, An R. Effectiveness of a body shape index (ABSI) in predicting chronic diseases and mortality: a systematic review and meta-analysis. Obes Rev. 2018;19:737–59.
Fujita M, Sato Y, Nagashima K, Takahashi S, Hata A. Predictive power of a body shape index for development of diabetes, hypertension, and dyslipidemia in Japanese adults: a retrospective cohort study. PLOS ONE. 2015;10:e0128972.
Silva AM, Shen W, Heo M, Gallagher D, Wang Z, Sardinha LB, et al. Ethnicity-related skeletal muscle differences across the lifespan. Am J Hum Biol. 2010;22:76–82.
Lear SA, Humphries KH, Kohli S, Chockalingam A, Frohlich JJ, Birmingham CL. Visceral adipose tissue accumulation differs according to ethnic background: results of the Multicultural Community Health Assessment Trial (M-CHAT). Am J Clin Nutr. 2007;86:353–9.
Tsou MT, Chang YC, Hsu CP, Kuo YC, Yun CH, Huang WH, et al. Visceral adiposity index outperforms conventional anthropometric assessments as predictor of diabetes mellitus in elderly Chinese: a population-based study. Nutr Metab (Lond). 2021;18:87.
Cheung YB. “A Body Shape Index” in middle-age and older Indonesian population: scaling exponents and association with incident hypertension. PLoS One. 2014;9:e85421.
Wilmet G, Verlinde R, Vandevoorde J, Carnol L, Devroey D. Correlation between body mass index and abdominal circumference in Belgian adults: a cross-sectional study. Rom J Intern Med. 2017;55:28–35.
Maessen MF, Eijsvogels TM, Verheggen RJ, Hopman MT, Verbeek AL, de Vegt F. Entering a new era of body indices: the feasibility of a body shape index and body roundness index to identify cardiovascular health status. PLOS ONE. 2014;9:e107212.
Kajikawa M, Maruhashi T, Kishimoto S, Yamaji T, Harada T, Hashimoto Y, et al. A body shape index is associated with endothelial dysfunction in both men and women. Sci Rep. 2021;11:17873.
Zhang Y, Yang H, Ren M, Wang R, Zhao F, Liu T, et al. Distribution of risk factors of hypertension patients in different age groups in Tianjin. BMC Public Health. 2021;21:247.
Acknowledgements
We thank the medical staff at Kagoshima Kouseiren Hospital for their support in data collection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kawasoe, S., Kubozono, T., Salim, A.A. et al. Association between anthropometric indices and 5-year hypertension incidence in the general Japanese population. Hypertens Res 47, 867–876 (2024). https://doi.org/10.1038/s41440-023-01505-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-023-01505-6
Keywords
This article is cited by
-
Sex and age difference in associations between anthropometric indices and hypertension
Hypertension Research (2024)