Hypertensive disorders of pregnancy include chronic hypertension, gestational hypertension, preeclampsia/eclampsia, and preeclampsia superimposed on chronic hypertension [1]. Hypertension in pregnancy is defined by the most guidelines as blood pressure ≥140/90 mmHg. Nevertheless, the initiation of antihypertensive treatment during pregnancy exhibits a degree of variability. This variability stems from the prevailing uncertainty regarding the advantages of lowering maternal blood pressure and the potential fetal risks associated with the impact of antihypertensive medications on utero-placental circulation, as well as the reported alterations in fetal growth resulting from in utero exposure to such medications. This is important because hypertensive disorders affect up to 10% of pregnancies worldwide, being a major health problem for women and their infants and causing increased maternal and infant morbidity and mortality [2]. Hence, enhancements in the identification and management of risks have the potential to markedly alleviate the burden imposed by hypertensive disorders during pregnancy.
The present study by Salazar et al. [3] provides insights into the benefits of treating mild chronic hypertension during pregnancy. This debate has been fueled by recent discrepant findings that describe the beneficial effects of pharmacologically treating pregnant women with mild chronic hypertension on the reduction of preeclampsia/eclampsia risk and the risk of small-for-gestational-age infants [4, 5]. Salazar and colleagues conducted an analysis to investigate the correlation between the blood pressure levels achieved through antihypertensive treatment and the risk of developing preeclampsia/eclampsia in pregnant women with chronic hypertension. They conducted a historical cohort study on pregnant women undergoing treatment for chronic hypertension, incorporating both office blood pressure readings and ambulatory blood pressure monitoring (ABPM) after 20 weeks of gestation. This allowed them to categorize the cohort into four groups: controlled hypertension, white-coat uncontrolled hypertension, masked uncontrolled hypertension, and sustained hypertension.
Their findings revealed that sustained uncontrolled hypertension (defined as office blood pressure ≥ 140/90 mmHg and 24-h ABPM ≥ 130/80 mmHg) and masked uncontrolled hypertension (defined as office blood pressure < 140/90 mmHg and 24-hour ABPM ≥ 130/80 mmHg) were associated with a similar increase in the risk of preeclampsia/eclampsia. Controlled hypertension (office blood pressure < 140/90 mmHg and 24-h ABPM < 130/80 mmHg) or white-coat uncontrolled hypertension (office blood pressure ≥ 140/90 mmHg and 24-h ABPM < 130/80 mmHg) did not exhibit a significant risk of preeclampsia/eclampsia. Furthermore, within this cohort, nocturnal hypertension and blood pressure levels achieved during the nighttime period emerged as the most robust predictors for the development of preeclampsia/eclampsia.
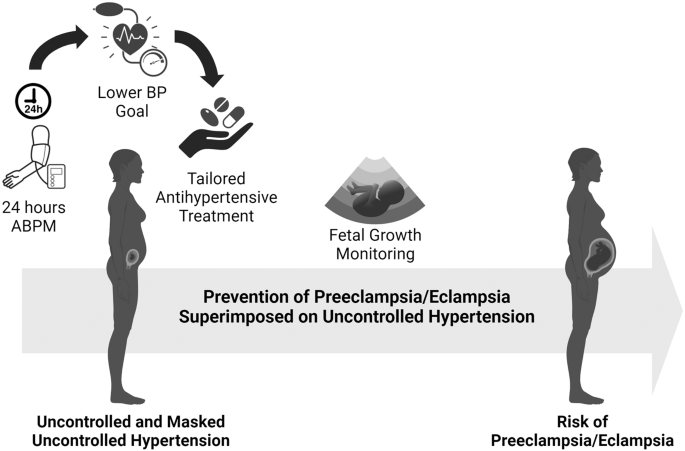
Based on the compelling findings presented by Salazar et al. [3], three pivotal considerations should be taken into account when diagnosing and managing chronic hypertension during pregnancy (as illustrated in Fig. 1). The first critical issue revolves around the methodology employed for diagnosing and monitoring uncontrolled blood pressure. This underscores the importance of employing accurate techniques for early-gestation blood pressure measurement to correctly diagnose chronic hypertension and identify individuals with uncontrolled and masked uncontrolled elevated blood pressure. Ambulatory blood pressure monitoring (ABPM) has been demonstrated to enhance both diagnosis and risk prediction in general hypertension, with additional evidence supporting its utility in managing hypertensive disorders during pregnancy. In the context of pregnancy, ABPM is recommended for identifying white-coat hypertension. However, Salazar and colleagues previously published data have underscored the indispensable role of ABPM in uncovering masked hypertension when out-of-office values are elevated but office blood pressure remains within the normal range [6]. More specifically, they have documented that nearly 60% of pregnancies initially classified as gestational hypertensive (according to current guidelines) were, in fact, cases of masked chronic hypertension. This finding holds significant importance, as masked uncontrolled hypertension, as highlighted by this study and others, has been associated with an increased risk of preeclampsia during pregnancy. Furthermore, the markedly elevated risk of preeclampsia in pregnancies with persistently elevated nighttime blood pressure values, as demonstrated by Salazar et al. [3], sheds additional light on the necessity for stringent blood pressure monitoring, including 24-h assessment, in women with uncontrolled blood pressure.
The second crucial issue under consideration pertains to the necessity of lowering the targeted blood pressure goals for managing treated chronic hypertension during pregnancy. This proposition gains substantial support from Tita et al. [4] findings, which demonstrated that aiming for a blood pressure goal lower than 140 mmHg reduced the risk of preeclampsia in pregnant women receiving treatment. Moreover, the study of Ueda et al. [7] further reinforces this argument by highlighting the positive effects of even more stringent blood pressure goals. According to their research, women with systolic blood pressure levels below 130 mmHg at 16–19 weeks of gestation exhibited a significantly reduced risk of early-onset superimposed preeclampsia compared to those with systolic blood pressure readings exceeding 140 mmHg. These findings align with the results of a meta-analysis, which indicated that blood pressure-lowering treatment during pregnancy, aiming for an achieved systolic blood pressure below 130 mmHg, reduced the risk of severe hypertension to nearly one-third when compared to maintaining systolic blood pressure levels above 140 mmHg [8]. It is worth noting, however, that this approach was associated with an increased risk of infants being born small for their gestational age. This collective body of evidence suggests that targeting a systolic blood pressure below 130 mmHg during pregnancy through blood pressure-lowering treatment may significantly decrease the risk of preeclampsia. Nonetheless, it is essential to accompany this approach with meticulous monitoring of fetal growth due to the identified increased risk of infants being small for their gestational age.
The third critical issue addressed pertains to the selection and adherence to antihypertensive treatment during pregnancy. Concerns regarding the potential association between aggressive blood pressure reduction and fetal growth restriction represent significant barriers to the consistent use of antihypertensive medications during pregnancy. The present study of Salazar et al. [3] made an important observation by noting a trend towards a higher prevalence of neonates classified as small for their gestational age among women with uncontrolled hypertension who were also taking multiple antihypertensive drugs. The mechanisms responsible for fetal growth restriction in women treated with antihypertensive drugs during pregnancy remain incompletely understood. Furthermore, whether such adverse effects are dependent on the specific type of antihypertensive agent remains an open question. The available options for antihypertensive treatment during hypertensive pregnancies are limited and include medications like methyldopa, calcium channel blockers, β-blockers, and diuretics. It’s worth noting that first-line antihypertensive drugs that block the renin-angiotensin system, such as angiotensin-converting-enzyme inhibitors and angiotensin receptor blockers, are contraindicated due to their known teratogenic effects [1]. A systematic review comparing the effects of available antihypertensive drugs for pregnancy revealed that both atenolol and labetalol, which are both β-blockers, significantly increased the risk of neonates being classified as small for their gestational age [9]. Additionally, these drugs were associated with elevated rates of caesarean delivery. It is hypothesized that β-blockers’ negative inotropic and chronotropic properties can reduce maternal cardiac output, subsequently affecting placental perfusion and fetal growth [10].
In conclusion, the choice and adherence to antihypertensive treatment during pregnancy present complex challenges, particularly in light of concerns about potential fetal growth restrictions associated with certain medications. Further research is needed to better understand the mechanisms at play and to refine treatment approaches for pregnant women with chronic hypertension.
References
Magee LA, Pels A, Helewa M, Rey E, von Dadelszen P, Committee SHG. Diagnosis, evaluation, and management of the hypertensive disorders of pregnancy: executive summary. J Obstet Gynaecol Can : JOGC = J d’obstetrique et gynecologie du Can : JOGC. 2014;36:575–6.
Abalos E, Cuesta C, Carroli G, Qureshi Z, Widmer M, Vogel JP, et al. Pre-eclampsia, eclampsia and adverse maternal and perinatal outcomes: a secondary analysis of the world health organization multicountry survey on maternal and newborn health. BJOG : Int J Obstet Gynaecol. 2014;121:14–24.
Salazar MR, Espeche WG, Minetto J, Carrera PR, Cerri G, Leiva Sisnieguez CB, et al. Uncontrolled and masked uncontrolled blood pressure in treated pregnant women with chronic hypertension and risk for preeclampsia/eclampsia. Hypertens Res. 2023. https://doi.org/10.1038/s41440-023-01443-3.
Tita AT, Szychowski JM, Boggess K, Dugoff L, Sibai B, Lawrence K, et al. Treatment for mild chronic hypertension during pregnancy. N Engl J Med. 2022;386:1781–92.
Webster LM, Conti-Ramsden F, Seed PT, Webb AJ, Nelson-Piercy C, Chappell LC. Impact of antihypertensive treatment on maternal and perinatal outcomes in pregnancy complicated by chronic hypertension: a systematic review and meta-analysis. J. Am Heart Assoc. 2017;6:e005526.
Espeche WG, Salazar MR, Minetto J, Leiva Sisnieguez CE, Cerri G, Balbin E, et al. Hypertension arising after 20 weeks of gestation: gestational hypertension or masked chronic hypertension? J Hum Hypertens. 2023;37:813–7.
Ueda A, Hasegawa M, Matsumura N, Sato H, Kosaka K, Abiko K, et al. Lower systolic blood pressure levels in early pregnancy are associated with a decreased risk of early-onset superimposed preeclampsia in women with chronic hypertension: a multicenter retrospective study. Hypertens Res : Off J Jpn Soc Hypertens. 2022;45:135–45.
Abe M, Arima H, Yoshida Y, Fukami A, Sakima A, Metoki H, et al. Optimal blood pressure target to prevent severe hypertension in pregnancy: a systematic review and meta-analysis. Hypertens Res : Off J Jpn Soc Hypertens. 2022;45:887–99.
Bellos I, Pergialiotis V, Papapanagiotou A, Loutradis D, Daskalakis G. Comparative efficacy and safety of oral antihypertensive agents in pregnant women with chronic hypertension: a network metaanalysis. Am J Obstet Gynecol. 2020;223:525–37.
Carr DB, Tran LT, Brateng DA, Kawamura C, Shofer JB, Karumanchi SA, et al. Hemodynamically-directed atenolol therapy is associated with a blunted rise in maternal sFLT-1 levels during pregnancy. Hypertens Pregnancy. 2009;28:42–55.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bertagnolli, M. Mitigating preeclampsia risk through effective uncontrolled blood pressure management. Hypertens Res 47, 545–547 (2024). https://doi.org/10.1038/s41440-023-01489-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-023-01489-3