Abstract
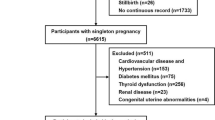
The association between maternal preconception blood pressure (BP) and preterm birth (PTB) is still unclear. The purpose of this study was to investigate the association between maternal preconception BP and PTB. This population-based cohort study included 715 984 Chinese women aged 20–49 years who participated in the National Free Preconception Health Examination Project and successfully had a singleton livebirth during 2014–2019 in Guangdong Province, China. Maternal preconception BP were measured by trained health workers. Multivariate logistic regression models and restricted cubic spline regressions were used to examine the association and dose–response relationship between maternal preconception BP and PTB, respectively. Maternal preconception hypertension was associated with the increased risk of PTB (adjusted odds ratios (aOR): 1.24; 95% CI: 1.14–1.34). Compared to women with normal preconception BP, the aORs for PTB were 1.09 (95% CI: 1.06–1.12), 1.24 (95% CI: 1.13–1.36), and 1.43 (95% CI: 1.15–1.79) for women with preconception elevated BP (120–139/ 80–89 mmHg, stage-1 hypertension (140–159/ 90–99 mmHg, and stage-2 hypertension (160–179/100–109 mmHg), respectively. According to the 2017 American College of Cardiology/American Heart Association criteria, maternal preconception elevated BP and hypertension were also significantly associated with an increased risk of PTB. Preconception systolic and diastolic BP showed a U-shaped (χ2 = 40.54; nonlinear P < 0.001) and linear (χ2 = 6.62; nonlinear P = 0.085) dose–response relationship with PTB, respectively. The association was modified by maternal age and preconception body mass index. These findings identify maternal preconception elevated BP and hypertension as a modifiable risk factor for PTB, providing evidence for future research studies, public health and clinical interventions.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Walani SR. Global burden of preterm birth. Int J Gynaecol Obstet. 2020;150:31–3.
Cao G, Liu J, Liu M. Global, regional, and national incidence and mortality of neonatal preterm birth, 1990–2019. JAMA Pediatr. 2022;176:787–96.
Deng K, Liang J, Mu Y, Liu Z, Wang Y, Li M, et al. Preterm births in China between 2012 and 2018: an observational study of more than 9 million women. Lancet Glob Health. 2021;9:e1226–e41.
Liu J, Zhang S, Liu M, Wang Q, Shen H, Zhang Y. Maternal pre-pregnancy infection with hepatitis B virus and the risk of preterm birth: a population-based cohort study. Lancet Glob Health. 2017;5:e624–e32.
Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet. 2008;371:75–84.
He C, Liu L, Chu Y, Perin J, Dai L, Li X, et al. National and subnational all-cause and cause-specific child mortality in China, 1996-2015: a systematic analysis with implications for the Sustainable Development Goals. Lancet Glob Health. 2017;5:e186–e97.
Bello NA, Zhou H, Cheetham TC, Miller E, Getahun DT, Fassett MJ, et al. Prevalence of hypertension among pregnant women when using the 2017 American College of Cardiology/American Heart Association Blood Pressure Guidelines and Association With Maternal and Fetal Outcomes. JAMA Netw Open. 2021;4:e213808.
Hypertension in Pregnancy: Executive Summary. Obstetrics & Gynecology. 2013;122:1122–31.
Gunnarsdottir J, Akhter T, Hogberg U, Cnattingius S, Wikstrom AK. Elevated diastolic blood pressure until mid-gestation is associated with preeclampsia and small-for-gestational-age birth: a population-based register study. BMC Preg Childbirth. 2019;19:186.
Wu DD, Gao L, Huang O, Ullah K, Guo MX, Liu Y, et al. Increased adverse pregnancy outcomes associated with stage 1 hypertension in a low-risk cohort: evidence from 47 874 cases. Hypertension. 2020;75:772–80.
Nobles CJ, Mendola P, Mumford SL, Silver RM, Kim K, Andriessen VC, et al. Preconception blood pressure and its change into early pregnancy: early risk factors for preeclampsia and gestational hypertension. Hypertension. 2020;76:922–9.
Magnussen EB, Vatten LJ, Myklestad K, Salvesen KA, Romundstad PR. Cardiovascular risk factors prior to conception and the length of pregnancy: population-based cohort study. Am J Obstet Gynecol. 2011;204:526 e1–8.
Jung YM, Oh GC, Noh E, Lee HY, Oh MJ, Park JS, et al. Pre-pregnancy blood pressure and pregnancy outcomes: a nationwide population-based study. BMC Preg Childbirth. 2022;22:226.
Harville EW, Myers L, Shu T, Wallace ME, Bazzano LA. Pre-pregnancy cardiovascular risk factors and racial disparities in birth outcomes: the Bogalusa Heart Study. BMC Preg Childbirth. 2018;18:339.
Harville EW, Viikari JS, Raitakari OT. Preconception cardiovascular risk factors and pregnancy outcome. Epidemiology. 2011;22:724–30.
Vladutiu CJ, Butera NM, Sotres-Alvarez D, Stuebe AM, Aviles-Santa L, Daviglus ML, et al. Preconception cardiometabolic markers and birth outcomes among women in the Hispanic community health study/study of Latinos. J Womens Health. 2022;31:1727–35.
Raghuraman N, Tuuli MG. Preconception care as an opportunity to optimize pregnancy outcomes. JAMA. 2021;326:79–80.
Yang Y, He Y, Li Q, Wang Y, Peng Z, Xu J, et al. Preconception blood pressure and risk of preterm birth: a large historical cohort study in a Chinese rural population. Fertil Steril. 2015;104:124–30.
Li N, Li Z, Ye R, Zhu Y, Li S, Yang N, et al. Preconception blood pressure and risk of preterm birth: a large cohort study in China. J Hypertens. 2016;34:2243–7.
Tang J, Zhu X, Li M, Huang D, Zhao Q. The impact of maternal prepregnancy impaired fasting glucose on preterm birth and large for gestational age: a large population-based cohort study. Am J Obstet Gynecol. 2020;222:265 e1–e19.
Xiong W, Han L, Li R, Tang X, Fan C, Liu X, et al. Preconception syphilis seroprevalence and association with duration of marriage and age among married individuals in Guangdong Province, China: a population-based cross-sectional study. PLoS Negl Trop Dis. 2022;16:e0010884.
Zhang SK, Wang QM, Shen HP. Design of the national free preconception health examination project in China (in Chinese). Natl Med J Chin. 2015;95:162–5.
Zhou Q, Zhang S, Wang Q, Shen H, Tian W, Chen J, et al. China’s community-based strategy of universal preconception care in rural areas at a population level using a novel risk classification system for stratifying couples´ preconception health status. BMC Health Serv Res. 2016;16:689.
Writing Group of 2018 Chinese Guidelines for the Management of Hypertension. 2018 Chinese guidelines for the management of hypertension. Chin J Cardiovasc Med. 2019;24:24–56.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71:e127–e248.
Wang YY, Li Q, Guo Y, Zhou H, Wang X, Wang Q, et al. Association of long-term exposure to airborne particulate matter of 1 μm or less with preterm birth in China. JAMA Pediatr. 2018;172:e174872.
Liu B, Xu G, Sun Y, Du Y, Gao R, Snetselaar LG, et al. Association between maternal pre-pregnancy obesity and preterm birth according to maternal age and race or ethnicity: a population-based study. Lancet Diabetes Endocrinol. 2019;7:707–14.
Fafard St-Germain AA, Kirby RS, Urquia ML. Reproductive health among married and unmarried mothers aged less than 18, 18-19, and 20-24 years in the United States, 2014-2019: a population-based cross-sectional study. PLoS Med. 2022;19:e1003929.
VanderWeele TJ, Ding P. Sensitivity analysis in observational research: introducing the E-value. Ann Intern Med. 2017;167:268–74.
Ardissino M, Slob EAW, Millar O, Reddy RK, Lazzari L, Patel KHK, et al. Maternal hypertension increases risk of preeclampsia and low fetal birthweight: genetic evidence from a Mendelian randomization study. Hypertension. 2022;79:588–98.
Harville EW, Juonala M, Viikari JS, Raitakari OT. Preconception metabolic indicators predict gestational diabetes and offspring birthweight. Gynecol Endocrinol. 2014;30:840–4.
Everett TR, Lees CC. Beyond the placental bed: placental and systemic determinants of the uterine artery Doppler waveform. Placenta. 2012;33:893–901.
Bushnell C, McCullough LD, Awad IA, Chireau MV, Fedder WN, Furie KL, et al. Guidelines for the prevention of stroke in women: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45:1545–88.
Tita AT, Szychowski JM, Boggess K, Dugoff L, Sibai B, Lawrence K, et al. Treatment for mild chronic hypertension during pregnancy. N Engl J Med. 2022;386:1781–92.
Cnattingius S, Villamor E, Johansson S, Edstedt Bonamy AK, Persson M, Wikström AK, et al. Maternal obesity and risk of preterm delivery. JAMA. 2013;309:2362–70.
Cappelletti M, Della Bella S, Ferrazzi E, Mavilio D, Divanovic S. Inflammation and preterm birth. J Leuk Biol. 2016;99:67–78.
ACOG Practice Bulletin No. 203: Chronic Hypertension in Pregnancy. Obstetrics & Gynecology. 2019;133:e26–e50.
Zhao J, Zhang X, Guan T, Wang X, Zhang H, Zeng X, et al. The association between glucose-6-phosphate dehydrogenase deficiency and abnormal blood pressure among prepregnant reproductive-age Chinese females. Hypertens Res. 2019;42:75–84.
Hong X, Zhao J, Huang K, Dai Q, Zhang H, Xuan Y, et al. Preconception blood pressure and time to pregnancy among couples attempting to conceive their first pregnancy. Am J Obstet Gynecol. 2019;221:470 e1–e10.
Acknowledgements
We would like to thank all the community workers, health workers and participants involved in the National Free Preconception Health Examination Project for their generous help during the data gathering process.
Funding
National Natural Science Foundation of China grants (No. 72274225), Guangdong Province Medical Research Funding (No. 2022314, No. B2023416, No. 2022326, and No. B2023135). The funders had no role in study design, data collection, data analysis, data interpretation, or writing the report.
Author information
Authors and Affiliations
Contributions
LH, XL, HN, WQ, and YH obtained access to the data from the National Free Preconception Health Examination Project in Guangdong Province, China. WX and LL developed the study and analytical strategy. WX, RL, ZZ did statistical analysis and WX drafted the manuscript. XT, QW, WC, HZ, and LL revised the manuscript and gave critical inputs into the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xiong, W., Han, L., Tang, X. et al. Association of maternal preconception blood pressure with preterm birth: a population-based cohort study. Hypertens Res 47, 467–477 (2024). https://doi.org/10.1038/s41440-023-01483-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-023-01483-9
Keywords
This article is cited by
-
Maternal preconception blood pressure and the association with preterm birth
Hypertension Research (2024)