Abstract
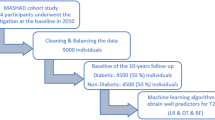
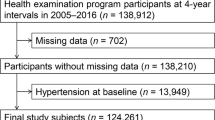
In this paper, we are going to investigate the association between Hypertension (HTN) and routine hematologic indices in a cohort of Iranian adults. The data were obtained from a total population of 9704 who were aged 35–65 years, a prospective study was designed. The association between hematologic factors and HTN was assessed using logistic regression (LR) analysis and a decision tree (DT) algorithm. A total of 9704 complete datasets were analyzed in this cohort study (N = 3070 with HTN [female 62.47% and male 37.52%], N = 6634 without HTN [female 58.90% and male 41.09%]). Several variables were significantly different between the two groups, including age, smoking status, BMI, diabetes millitus, high sensitivity C-reactive protein (hs-CRP), uric acid, FBS, total cholesterol, HGB, LYM, WBC, PDW, RDW, RBC, sex, PLT, MCV, SBP, DBP, BUN, and HCT (P < 0.05). For unit odds ratio (OR) interpretation, females are more likely to have HTN (OR = 1.837, 95% CI = (1.620, 2.081)). Among the analyzed variables, age and WBC had the most significant associations with HTN OR = 1.087, 95% CI = (1.081, 1.094) and OR = 1.096, 95% CI = (1.061, 1.133), respectively (P-value < 0.05). In the DT model, age, followed by WBC, sex, and PDW, has the most significant impact on the HTN risk. Ninety-eight percent of patients had HTN in the subgroup with older age (≥58), high PDW (≥17.3), and low RDW (<46). Finally, we found that elevated WBC and PDW are the most associated factor with the severity of HTN in the Mashhad general population as well as female gender and older age.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
GBD 2017 Risk Factor Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1923–94.
GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1736–88.
Tayefi M, Shabani N, Saberi-Karimian M, Oladi M, Mouhebati M, Farjami Z, et al. Systolic and diastolic blood pressure percentiles by age and gender in Northeastern Iran. J Am Soc Hypertens. 2018;12:e85–91.
Flack JM, Adekola B. Blood pressure and the new ACC/AHA hypertension guidelines. Trends Cardiovasc Med. 2020;30:160–4.
Aghasizadeh M, Samadi S, Sahebkar A, Miri‐Moghaddam E, Esmaily H, Souktanloo M, et al. Serum HDL cholesterol uptake capacity in subjects from the MASHAD cohort study: Its value in determining the risk of cardiovascular endpoints. J Clin Lab Anal. 2021;35:e23770.
Fakhri M, Sarokhani D, Ghiasi B, Dehkordi AH. Prevalence of hypertension in cardiovascular disease in iran: systematic review and meta-analysis. Int J Prev Med. 2020;11:56.
Shrestha PL, Shrestha PA, Vivo RP. Epidemiology of comorbidities in patients with hypertension. Curr Opin Cardiol. 2016;31:376–80.
Aghasizadeh M, Bizhaem SK, Baniasadi M, Khazdair MR, Kazemi T. Evaluation of LDL goal achievement in statin consumption, south east of Iran. Sci Rep. 2021;11:1–8.
Ishida S, Kondo S, Funakoshi S, Satoh A, Maeda T, Kawazoe M, et al. White blood cell count and incidence of hypertension in the general Japanese population: ISSA-CKD study. PLoS One. 2021;16:e0246304.
Jeong HR, Shim YS, Lee HS, Hwang JS. Hemoglobin and hematocrit levels are positively associated with blood pressure in children and adolescents 10 to 18 years old. Sci Rep. 2021;11:19052.
Kim NH, Lee JM, Kim HC, Lee JY, Yeom H, Lee JH, et al. Cross-sectional and longitudinal association between hemoglobin concentration and hypertension: a population-based cohort study. Medicine. 2016;95:e5041.
Lee SG, Rim JH, Kim JH. Association of hemoglobin levels with blood pressure and hypertension in a large population-based study: the Korea National Health and Nutrition Examination Surveys 2008-2011. Clin Chim Acta. 2015;438:12–8.
Atsma F, Veldhuizen I, de Kort W, van Kraaij M, Pasker-de Jong P, Deinum J. Hemoglobin level is positively associated with blood pressure in a large cohort of healthy individuals. Hypertension. 2012;60:936–41.
Liu X, Liang J, Qiu Q, Zhu Y, Sun Y, Ying P, et al. Association of hematocrit and pre-hypertension among Chinese adults: the CRC study. Cell Biochem Biophys. 2015;71:1123–8.
Paul L, Jeemon P, Hewitt J, McCallum L, Higgins P, Walters M, et al. Hematocrit predicts long-term mortality in a nonlinear and sex-specific manner in hypertensive adults. Hypertension. 2012;60:631–8.
Pusuroglu H, Akgul O, Erturk M, Surgit O, Tasbulak O, Akkaya E, et al. Red cell distribution width and end-organ damage in patients with systo-diastolic hypertension. Arch Med Sci. 2016;12:319–25.
Emamian M, Hasanian SM, Tayefi M, Bijari M, Movahedian Far F, Shafiee M, et al. Association of hematocrit with blood pressure and hypertension. J Clin Lab Anal. 2017;31:e22124.
Merad-Boudia HN, Dali-Sahi M, Kachekouche Y, Dennouni-Medjati N. Hematologic disorders during essential hypertension. Diabetes Metab Syndr. 2019;13:1575–9.
Gang L, Yanyan Z, Zhongwei Z, Juan D. Association between mean platelet volume and hypertension incidence. Hypertens Res. 2017;40:779–84.
Pusuroglu H, Cizgici AY, Demir AR, Uygur B, Ozal E. Long-term prognostic value of mean platelet volume in patients with hypertension. Acta Cardiol Sin. 2021;37:504–11.
Akın H, Bilge Ö, Yavuz B, Özkan S, Işık F. The relationship between mean platelet volume and resistant hypertension. Clin Exp Hypertens. 2022;44:228–32.
Zhan YL, Zou B, Kang T, Xiong LB, Zou J, Wei YF. Multiplicative interaction between mean corpuscular volume and red cell distribution width with target organ damage in hypertensive patients. J Clin Lab Anal. 2017;31:e22082.
Lin S, Zhang L, Shen S, Wei D, Lu J, Chen X, et al. Platelet parameters and risk of hypertension disorders of pregnancy: a propensity score adjusted analysis. Platelets. 2022;33:543–50.
Li T, Jin J, Meng Z, Zhang W, Li Y, Yu X, et al. The different associations between platelet distribution width and hypertension subtypes in males and females. Biosci Rep. 2020;40:BSR20201747.
Anderson GH. Effect of age on hypertension: analysis of over 4,800 referred hypertensive patients. Saudi J Kidney Dis Transplant. 1999;10:286.
McEniery CM, Wilkinson IB, Avolio AP. Age, hypertension and arterial function. Clin Exp Pharmacol Physiol. 2007;34:665–71.
Gillis EE, Sullivan JC. Sex differences in hypertension: recent advances. Hypertension. 2016;68:1322–7.
Connelly PJ, Currie G, Delles C. Sex differences in the prevalence, outcomes and management of hypertension. Curr Hypertens Rep. 2022;24:185–92.
Gilstrap LG, Wang TJ. Biomarkers and cardiovascular risk assessment for primary prevention: an update. Clin Chem. 2012;58:72–82.
den Engelsen C, Koekkoek PS, Gorter KJ, van den Donk M, Salomé PL, Rutten GE. High-sensitivity C-reactive protein to detect metabolic syndrome in a centrally obese population: a cross-sectional analysis. Cardiovasc Diabetol. 2012;11:1–7.
Shah T, Newcombe P, Smeeth L, Addo J, Casas JP, Whittaker J, et al. Ancestry as a determinant of mean population C-reactive protein values: implications for cardiovascular risk prediction. Circulation. 2010;3:436–44.
Deo RC. Machine learning in medicine. Circulation. 2015;132:1920–30.
Saberi‐Karimian M, Safarian‐Bana H, Mohammadzadeh E, Kazemi T, Mansoori A, Ghazizadeh H, et al. A pilot study of the effects of crocin on high‐density lipoprotein cholesterol uptake capacity in patients with metabolic syndrome: a randomized clinical trial. BioFactors. 2021;47:1032–41.
Mahesh B. Machine learning algorithms -a review. International Journal of Science and Research. 2020;9:381–6.
Ghayour-Mobarhan M, Moohebati M, Esmaily H, Ebrahimi M, Parizadeh SMR, Heidari-Bakavoli AR, et al. Mashhad stroke and heart atherosclerotic disorder (MASHAD) study: design, baseline characteristics and 10-year cardiovascular risk estimation. Int J Public Health. 2015;60:561–72.
Hosmer Jr DW, Lemeshow S, Sturdivant RX. Applied logistic regression. 3rd ed. Hoboken, NJ: John Wiley & Sons; 2013.
Hooley JM, Teasdale JD. Predictors of relapse in unipolar depressives: expressed emotion, marital distress, and perceived criticism. J Abnorm Psychol. 1989;98:229.
Mohammadi F, Pourzamani H, Karimi H, Mohammadi M, Mohammadi M, Ardalan N, et al. Artificial neural network and logistic regression modelling to characterize COVID-19 infected patients in local areas of Iran. Biomed J. 2021;44:304–16.
Saberi-Karimian M, Khorasanchi Z, Ghazizadeh H, Tayefi M, Saffar S, Ferns GA, et al. Potential value and impact of data mining and machine learning in clinical diagnostics. Crit Rev Clin Lab Sci. 2021;58:275–96.
Mohammadi M, Mansoori A. A projection neural network for identifying copy number variants. IEEE J Biomed health Inform. 2018;23:2182–8.
The analysis of cases based on decision tree. In Zhong Y, editor. 7th IEEE international conference on software engineering and service science (ICSESS). Beijing: IEEE; 2016.
Mansoori A, Sahranavard T, Hosseini ZS, Soflaei SS, Emrani N, Nazar E, et al. Prediction of type 2 diabetes mellitus using hematological factors based on machine learning approaches: a cohort study analysis. Sci Rep. 2023;13:1–11.
Saberi‐Karimian M, Mansoori A, Bajgiran MM, Hosseini ZS, Kiyoumarsioskouei A, Rad ES, et al. Data mining approaches for type 2 diabetes mellitus prediction using anthropometric measurements. J Clin Lab Anal. 2023;37:e24798.
Mansoori A, Hosseini ZS, Ahari RK, Poudineh M, Rad ES, Zo MM, et al. Development of data mining algorithms for identifying the best anthropometric predictors for cardiovascular disease: MASHAD cohort study. High Blood Press Cardiovasc Prev. 2023;30:243–53.
Ghazizadeh H, Shakour N, Ghoflchi S, Mansoori A, Saberi-Karimiam M, Rashidmayvan M, et al. Use of data mining approaches to explore the association between type 2 diabetes mellitus with SARS-CoV-2. BMC Pulm Med. 2023;23:1–14.
Wu S, Jin C, Li S, Zheng X, Zhang X, Cui L, et al. Aging, arterial stiffness, and blood pressure association in chinese adults. Hypertension. 2019;73:893–9.
Zheng M, Xu X, Wang X, Huo Y, Xu X, Qin X, et al. Age, arterial stiffness, and components of blood pressure in Chinese adults. Medicine. 2014;93:e262.
Rockwood MR, Howlett SE. Blood pressure in relation to age and frailty. Can Geriatrics J. 2011;14:2.
Franklin SS. Ageing and hypertension: the assessment of blood pressure indices in predicting coronary heart disease. J Hypertens Suppl. 1999;17:S29–36.
Gu Q, Burt VL, Paulose-Ram R, Dillon CF. Gender differences in hypertension treatment, drug utilization patterns, and blood pressure control among US adults with hypertension: data from the National Health and Nutrition Examination Survey 1999–2004. Am J Hypertens. 2008;21:789–98.
Wang Z, Chen Z, Zhang L, Wang X, Hao G, Zhang Z, et al. Status of hypertension in china: results from the China Hypertension Survey, 2012-2015. Circulation 2018;137:2344–56.
Ramirez LA, Sullivan JC. Sex differences in hypertension: where we have been and where we are going. Am J Hypertens. 2018;31:1247–54.
Lloyd-Jones DM, Evans JC, Levy D. Hypertension in adults across the age spectrum: current outcomes and control in the community. JAMA. 2005;294:466–72.
Zhang Y, Moran AE. Trends in the prevalence, awareness, treatment, and control of hypertension among young adults in the United States, 1999 to 2014. Hypertension. 2017;70:736–42.
Guo X, Zou L, Zhang X, Li J, Zheng L, Sun Z, et al. Prehypertension: a meta-analysis of the epidemiology, risk factors, and predictors of progression. Tex Heart Inst J. 2011;38:643–52.
Ndzie Noah ML, Adzika GK, Mprah R, Adekunle AO, Adu-Amankwaah J, Sun H. Sex-gender disparities in cardiovascular diseases: the effects of estrogen on eNOS, lipid profile, and NFATs during catecholamine stress. Front Cardiovasc Med. 2021;8:639946.
Shankar A, Klein BE, Klein R. Relationship between white blood cell count and incident hypertension. Am J Hypertens. 2004;17:233–9.
Friedman GD, Selby JV, Quesenberry CP Jr. The leukocyte count: a predictor of hypertension. J Clin Epidemiol. 1990;43:907–11.
Idler EL, Angel RJ. Self-rated health and mortality in the NHANES-I Epidemiologic Follow-up Study. Am J Public Health. 1990;80:446–52.
Orakzai R, Orakzai S, Nasir K, Santos R, Rana J, Pimentel I, et al. Association of white blood cell count with systolic blood pressure within the normotensive range. J Hum Hypertens. 2006;20:341–7.
Karthikeyan V, Lip G. White blood cell count and hypertension. J Hum Hypertens. 2006;20:310–2.
Curiati MNC, Silvestre OM, Pires LJT, Mangini S, Pires PV, Gaiotto FA, et al. Agreement of BNP and NT-proBNP and the influence of clinical and laboratory variables. Einstein. 2013;11:273–7.
Cheema AN, Khan DA, Tuyyab F. Early detection of cardiac dysfunction by BNP in beta-thalassaemia major patients. Acta Cardiologica. 2012;67:331–5.
Palazzuoli A, Quatrini I, Calabrò A, Antonelli G, Caputo M, Campagna MS, et al. Anemia correction by erythropoietin reduces BNP levels, hospitalization rate, and NYHA class in patients with cardio-renal anemia syndrome. Clin Exp Med. 2011;11:43–8.
Takeda T, Kohno M. Brain natriuretic peptide in hypertension. Hypertens Res. 1995;18:259–66.
Casserly B, Klinger JR. Brain natriuretic peptide in pulmonary arterial hypertension: biomarker and potential therapeutic agent. Drug Des Dev Ther. 2009;3:269.
Jae SY, Kurl S, Laukkanen JA, Heffernan KS, Choo J, Choi Y-H, et al. Higher blood hematocrit predicts hypertension in men. J Hypertens. 2014;32:245–50.
Tripolino C, Gnasso A, Carallo C, Scavelli FB, Irace C. Hemorheological profiles of subjects with prehypertension. Hypertens Res. 2016;39:519–23.
Divya R, Ashok V. A study of hematological parameters and anthropometric indicators in hypertensive and normotensive males. Int J Curr Res Rev. 2016;8:6.
Babu KR, Solepure A, Shaikh R. Comparison of hematological parameters in primary hypertensives and normotensives of sangareddy. Int J Biomed Res. 2015;6:309–15.
Karabulut A, Karadag A. Clinical implication of hematological indices in the essential hypertension. World J Hypertens. 2015;5:93–7.
Cirillo M, Laurenzi M, Trevisan M, Stamler J. Hematocrit, blood pressure, and hypertension. The Gubbio Population Study. Hypertension. 1992;20:319–26.
Al-Muhana F, Larbi E, Al-Ali A, Al-Sultan A, Al-Ateeeq S, Soweilem L, et al. Haematological, lipid profile and other biochemical parameters in normal and hypertensive subjects among the population of the eastern province of Saudi Arabia. East Afr Med J. 2006;83:44–8.
Ighoroje A, Dapper D. Sex variations in the haemorheological parameters of some hypertensive Nigerians as compared to hypertensive. Niger J Physiological Sci. 2005;20:33–8.
Bruschi G, Minari M, Bruschi ME, Tacinelli L, Milani B, Cavatorta A, et al. Similarities of essential and spontaneous hypertension. Volume and number of blood cells. Hypertension. 1986;8:983–9.
Postnov YV, Kravtsov GM, Orlov S, Pokudin N, Postnov IY, Kotelevtsev YV. Effect of protein kinase C activation on cytoskeleton and cation transport in human erythrocytes. Reproduction of some membrane abnormalities revealed in essential hypertension. Hypertension. 1988;12:267–73.
Sharp DS, Curb JD, Schatz IJ, Meiselman HJ, Fisher TC, Burchfiel CM, et al. Mean red cell volume as a correlate of blood pressure. Circulation. 1996;93:1677–84.
Enawgaw B, Adane N, Terefe B, Asrie F, Melku M. A comparative cross-sectional study of some hematological parameters of hypertensive and normotensive individuals at the university of Gondar hospital, Northwest Ethiopia. BMC Hematol. 2017;17:1–7.
Gunebakmaz O, Kaya MG, Duran M, Akpek M, Elcik D, Eryol NK. Red blood cell distribution width in ‘non-dippers’ versus ‘dippers’. Cardiology. 2012;123:154–9.
Enawgaw B, Adane N, Terefe B, Asrie F, Melku M. A comparative cross-sectional study of some hematological parameters of hypertensive and normotensive individuals at the university of Gondar hospital, Northwest Ethiopia. BMC Hematol. 2017;17:21.
Sileshi B, Urgessa F, Wordofa M. A comparative study of hematological parameters between hypertensive and normotensive individuals in Harar, eastern Ethiopia. PLoS One. 2021;16:e0260751.
Li N, Zhou H, Tang Q. Red blood cell distribution width: a novel predictive indicator for cardiovascular and cerebrovascular diseases. Dis Markers. 2017;2017:7089493.
Fornal M, Wizner B, Cwynar M, Królczyk J, Kwater A, Korbut RA, et al. Association of red blood cell distribution width, inflammation markers and morphological as well as rheological erythrocyte parameters with target organ damage in hypertension. Clin Hemorheol Microcirc. 2014;56:325–35.
Farhangi MA, Keshavarz S-A, Eshraghian M, Ostadrahimi A, Saboor-Yaraghi A-A. White blood cell count in women: relation to inflammatory biomarkers, haematological profiles, visceral adiposity, and other cardiovascular risk factors. J Health Popul Nutr. 2013;31:58.
Ozcan F, Turak O, Durak A, Işleyen A, Uçar F, Giniş Z, et al. Red cell distribution width and inflammation in patients with non-dipper hypertension. Blood Press. 2013;22:80–5.
Abul Y, Ozsu S, Korkmaz A, Bulbul Y, Orem A, Ozlu T. Red cell distribution width: a new predictor for chronic thromboembolic pulmonary hypertension after pulmonary embolism. Chron Respir Dis. 2014;11:73–81.
Tonelli M, Sacks F, Arnold M, Moye L, Davis B, Pfeffer M. Relation between red blood cell distribution width and cardiovascular event rate in people with coronary disease. Circulation. 2008;117:163–8.
Ates I, Bulut M, Ozkayar N, Dede F. Association between high platelet indices and proteinuria in patients with hypertension. Ann Lab Med. 2015;35:630–4.
Lande K, Os I, Kjeldsen SE, Westheim A, Hjermann I, Eide I, et al. Increased platelet size and release reaction in essential hypertension. J Hypertens. 1987;5:401–6.
Yaghoubi A, Golmohamadi Z, Alizadehasl A, Azarfarin R. Role of platelet parameters and haematological indices in myocardial infarction and unstable angina. J Pak Med Assoc. 2013;63:1133–7.
Lee KW, Blann AD, Lip GY. High pulse pressure and nondipping circadian blood pressure in patients with coronary artery disease: relationship to thrombogenesis and endothelial damage/dysfunction. Am J Hypertens. 2005;18:104–15.
Boos CJ, Beevers GD, Lip GY. Assessment of platelet activation indices using the ADVIATM 120 amongst ‘high‐risk’patients with hypertension. Ann Med. 2007;39:72–8.
Bae MH, Lee JH, Yang DH, Park HS, Cho Y, Chae SC. White blood cell, hemoglobin and platelet distribution width as short-term prognostic markers in patients with acute myocardial infarction. J Korean Med Sci. 2014;29:519–26.
Bekler A, Ozkan MTA, Tenekecioglu E, Gazi E, Yener AU, Temiz A, et al. Increased platelet distribution width is associated with severity of coronary artery disease in patients with acute coronary syndrome. Angiology. 2015;66:638–43.
Varol E, Akcay S, Icli A, Yucel H, Ozkan E, Erdogan D, et al. Mean platelet volume in patients with prehypertension and hypertension. Clin Hemorheol Microcirc. 2010;45:67–72.
Leow MK-S. Environmental origins of hypertension: phylogeny, ontogeny and epigenetics. Hypertens Res. 2015;38:299–307.
Siebers R, Maling T. Mean platelet volume in human essential hypertension. J Hum Hypertens. 1995;9:207.
Ahmadzadeh J, Mansorian B, Attari MM-A, Mohebbi I, Naz-Avar R, Moghadam K, et al. The association between hematological parameters and metabolic syndrome in Iranian men: a single center large-scale study. Diabetes Metab Syndrome Clin Res Rev. 2018;12:17–21.
Chul Sung K, Suh JY, Kim BS, Kang JH, Kim H, Lee MH, et al. High sensitivity C-reactive protein as an independent risk factor for essential hypertension. Am J Hypertens. 2003;16:429–33.
Fujii M, Ohnishi H, Saitoh S, Akasaka H, Miura T, Mori M. The combination of abdominal obesity and high-sensitivity C-reactive protein predicts new-onset hypertension in the general Japanese population: the Tanno–Sobetsu study. Hypertens Res. 2015;38:426–32.
Sesso HD, Buring JE, Rifai N, Blake GJ, Gaziano JM, Ridker PM. C-reactive protein and the risk of developing hypertension. JAMA. 2003;290:2945–51.
Tangvarasittichai S, Pingmuanglaew P, Tangvarasittichai O. Association of Elevated Serum Lipoprotein (a), inflammation, oxidative stress and chronic kidney disease with hypertension in non-diabetes hypertensive patients. Indian J Clin Biochem. 2016;31:446–51.
Niskanen L, Laaksonen DE, Nyyssönen K, Punnonen K, Valkonen V-P, Fuentes R, et al. Inflammation, abdominal obesity, and smoking as predictors of hypertension. Hypertension. 2004;44:859–65.
Verma S, Wang C-H, Li S-H, Dumont AS, Fedak PW, Badiwala MV, et al. A self-fulfilling prophecy: C-reactive protein attenuates nitric oxide production and inhibits angiogenesis. Circulation. 2002;106:913–9.
Venugopal SK, Devaraj S, Yuhanna I, Shaul P, Jialal I. Demonstration that C-reactive protein decreases eNOS expression and bioactivity in human aortic endothelial cells. Circulation. 2002;106:1439–41.
Devaraj S, Xu DY, Jialal I. C-reactive protein increases plasminogen activator inhibitor-1 expression and activity in human aortic endothelial cells: implications for the metabolic syndrome and atherothrombosis. Circulation. 2003;107:398–404.
Acknowledgements
We gratefully acknowledge the contributions of the data collection team and the individuals who participated in this study.
Author information
Authors and Affiliations
Contributions
AM: conception, data analyzing. NSFG: conception, drafting the article. LE: revising the article. MP: drafting the article. RKA: drafting the article. FM: drafting the article. MA: revising the article. ESR: drafting the article. GF: revising the article. HE: corresponding author. MG-M: corresponding author.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study protocol was reviewed and all methods are approved by the Ethics Committee of MUMS with approval number IR.MUMS.REC.1386.250. All methods were carried out in accordance with relevant guidelines and regulations. All the participants consented to take part in the study by signing written informed consent. Informed consent was obtained from all subjects using protocols approved by the Ethics Committee of the Mashhad University of Medical Science (MUMS), approval number IR.MUMS.REC.1386.250. All experiments were performed in accordance with relevant guidelines and regulations.
Consent to publication
It is not applicable to the Consent of Image Publication for this manuscript. The figures were designed only in this manuscript for presenting the results of the current paper.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mansoori, A., Farizani Gohari, N.S., Etemad, L. et al. White blood cell and platelet distribution widths are associated with hypertension: data mining approaches. Hypertens Res 47, 515–528 (2024). https://doi.org/10.1038/s41440-023-01472-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-023-01472-y
Keywords
This article is cited by
-
A link between white blood cell count and blood pressure levels
Hypertension Research (2024)
-
Uric acid is associated with type 2 diabetes: data mining approaches
Diabetology International (2024)
-
The relationship between anthropometric indices and the presence of hypertension in an Iranian population sample using data mining algorithms
Journal of Human Hypertension (2023)