Abstract
Smoking is associated with vascular endothelial dysfunction. It is thought that smoking impairs vascular endothelial function through a decrease in nitric oxide bioavailability induced by activation of oxidative stress and inflammation. Endothelial dysfunction can be improved or augmented by appropriate interventions including pharmacotherapy, administration of supplements and lifestyle modifications. Although there have not been many studies, the effects of smoking cessation on endothelial function have been shown. In those studies, it was shown that smoking cessation does not always have a positive effect on vascular endothelial function. In this review, I will focus on the role of smoking in endothelial function and the effects of smoking cessation on endothelial function.

Smoking impairs vascular endothelial function and leads to atherosclerosis. Smoking cessation is expected to improve vascular endothelial function. Effects of smoking cessation on endothelial function are not always consistent. Further studies are needed to determine whether smoking cessation directly improves endothelial function. NO indicates nitric oxide.
Similar content being viewed by others
Introduction
Smoking is deeply involved in the development, maintenance, and progression of atherosclerosis, and smoking itself is an independent risk factor for the development of cardiovascular events and death [1,2,3,4]. The clinical significance of vascular endothelial function has become clear in many aspects such as understanding the etiology, pathogenesis, involvement in the development of atherosclerosis, therapeutic targets, and prognostic factors. Vascular endothelial dysfunction is the first step in atherosclerosis and plays an important role in the development, maintenance, and progression of atherosclerosis, resulting in cardiovascular events [5, 6]. Smoking as well as hypertension, dyslipidemia, diabetes, obesity, aging, lack of exercise, excessive salt intake, and menopause are known to induce endothelial dysfunction [7]. Endothelial dysfunction can be improved by appropriate pharmacotherapy [8,9,10,11], replacement therapy [12, 13], and lifestyle modifications including aerobic exercise [14, 15], body weight reduction [16], decrease in salt intake [17] and smoking cessation [18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35]. The mechanisms by which smoking induces vascular endothelial dysfunction and the effects of smoking cessation on vascular endothelial function will be reviewed.
Smoking and atherosclerosis
Epidemiological studies have shown a strong correlation between cardiovascular disease and the amount and duration of smoking [1]. Epidemiological studies and large clinical trials have indicated that smoking is a major risk factor for atherosclerosis [1,2,3,4]. Smoking is associated with elevated low-density lipoprotein cholesterol, decreased high-density lipoprotein cholesterol, increased blood catecholamine levels, increased fibrinogen levels, and impaired vascular endothelial function [36,37,38,39,40,41,42,43,44,45,46,47,48]. Although it is not clear whether smoking cessation can improve advanced atherosclerosis, it is expected to reverse the promotion of atherosclerosis caused by smoking. Indeed, among female smokers, two years of smoking cessation reduced cardiovascular mortality by 24% [49], and smoking cessation after myocardial infarction has been reported to reduce mortality by 20–50% compared with that in continuing smokers [50]. Regardless of smoking quantity, duration, or age at the start of smoking cessation, smoking cessation for about five years reduces the risk of developing cardiovascular events to that of never-smokers [2].
Vascular endothelium structure and physiological function
The vascular endothelium is the innermost layer of the heart lumen, arteries, veins, and lymphatics and is composed of a single layer of vascular endothelial cells. Vascular endothelial cells produce and secrete many physiologically active substances including vasodilators, such as nitric oxide (NO), prostaglandin I2, C-type natriuretic peptide, and endothelium-derived vascular hyperpolarizing factor, and vasoconstrictors, such as endothelin, angiotensin II, prostaglandin H2 and thromboxane A2 [51, 52]. NO plays a very important role in atherosclerosis. The normal vascular endothelium regulates vasodilation and vasocontraction, proliferation and antiproliferation of vascular smooth muscle cells, coagulation and anticoagulation, inflammation and anti-inflammation, and oxidation and antioxidant effects, which work in balance to regulate and maintain vascular tone and structure [53]. Atherosclerosis develops as the first stage of vascular endothelial dysfunction. Further progression leads to cardiovascular events (e.g., angina pectoris, myocardial infarction, heart failure, stroke, and heart failure). If the entire body’s vascular endothelium could be collected, the total weight would be equivalent to that of the liver, and if it could be spread over an entire surface, the total area would be equivalent to six tennis courts, and it would be 100,000 km or two and a half times around the earth if it could be connected in a single row [6].
Smoking and vascular endothelial function
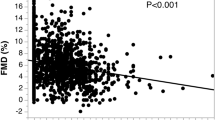
Many studies have shown that the vascular endothelium-dependent relaxation response is impaired in smokers and in experimental animal models [42,43,44,45,46,47,48, 54, 55]. In our studies also, endothelial function was impaired in smokers compared to that in nonsmokers after forearm artery administration of acetylcholine, an agonist of NO production [46]. Pre-administration of the NO synthase (NOS) inhibitor NG-monomethyl-L-arginine acetate abolished the difference in endothelium-dependent relaxation induced by acetylcholine between smokers and nonsmokers [46]. In a study in which vasodilation induced by reactive hyperemia, flow-mediated vasodilation (FMD), in forearm arteries was investigated, it was shown that FMD was decreased in smokers and that FMD decreased with increase in the amount of smoking [20, 23,24,25,26,27, 31,32,33, 42, 48]. In coronary arteries, decreased reactivity to endogenous NO and decreased production of endogenous NO itself have also been noted in smokers [56]. It has been reported that vascular endothelial function is impaired in passive smokers as well as in smokers and that there is a correlation between passive smoking duration and endothelial dysfunction [57, 58]. In addition, smoking further exacerbates endothelial dysfunction in individuals with hypertension, diabetes, dyslipidemia, and other coronary risk factors [45]. In a multivariate analysis using FMD as the index, smoking was also confirmed to be an independent risk factor for vascular endothelial dysfunction [59].
Several studies have shown that endothelial function assessed by biomarkers for endothelial function including circulating levels of nitrate/nitrite, NO, von Willebrand factor (vWF), cellular adhesion molecules, vascular cell adhesion molecule-1 (VCAM-1) and intercellular adhesion molecule-1 (ICAM-1), endothelial progenitor cells (EPCs) and endothelial microparticles (EMPs), endothelin-1 and activity of endothelial NOS (eNOS) other than physiological assessment for endothelial function was impaired in smokers. These findings suggest that smoking is associated with endothelial dysfunction [17, 18, 21, 22, 29, 60,61,62,63].
Mechanisms of smoking-induced vascular endothelial dysfunction
Figure 1 shows the putative mechanisms of smoking-induced vascular endothelial dysfunction.
Putative mechanism of vascular endothelial dysfunction induced by smoking. NADPH indicates nicotinamide adenine dinucleotide phosphate, ROCK Rho-associated kinase, SOD superoxide dismutase, ROS reactive oxygen species, eNOS endothelial nitric oxide synthase, MAPK mitogen-activated protein kinase, oxLDL oxidative low-density lipoprotein, NO nitric oxide, NF-κB nuclear factor-kappa B, AP-1 activator protein-1, VCAM-1 vascular cell adhesion molecule-1, ICAM-1 intracellular adhesion molecule-1, MCP-1 macrophage chemotactic protein 1, EPC endothelial progenitor cell
Involvement of oxidative stress
The increase in reactive oxygen species (ROS) caused by smoking is thought to play a critical role in vascular endothelial dysfunction. Inactivation of NO due to the increased NO scavenging associated with increased ROS production has attracted attention as one of the mechanisms of vascular endothelial dysfunction [64,65,66,67]. The ROS produced are converted to peroxynitrite, which has a very strong cytotoxic effect when combined with NO, resulting in direct damage to vascular wall cells and a decrease in the biological activity of NO in vascular endothelial cells and vascular smooth muscle cells [68]. Oxidative stress conditions lead to vascular endothelial dysfunction, expression of redox-sensitive genes, induction of inflammation, and development of atherosclerosis [69]. This chain of processes leading to ROS overproduction and vascular endothelial damage exists not only in experimental animal models but also in humans [70]. Cigarette smoke contains a wide variety and large amount of ROS. In smokers, there is a decrease in blood ascorbic acid levels and an increase in various oxidative stress markers in blood or urine. Even single smoking decreases blood NO metabolites and antioxidants such as ascorbic acid, cysteine, methionine and uric acid [71]. In smokers, there appears to be a disruption of antioxidant mechanisms and an increase in ROS-producing systems [72]. Although there is no consensus regarding the increased activation of nicotinamide adenine dinucleotide phosphate oxidase by smoking, xanthine oxidase, an ROS-producing system, is activated by smoking. In smokers, a single dose of the xanthine oxidase inhibitor allopurinol restores the acetylcholine-induced endothelium-dependent relaxation response in forearm arteries to nonsmoker levels but does not affect the endothelium-dependent relaxation response in nonsmokers [73]. Rapid administration of the antioxidant vitamin C may improve endothelial function in smokers [74]. Deficiency of tetrahydrobiopterin, an essential cofactor for eNOS, has been shown to promote eNOS unpairing, which attenuates NO production and tends to enhance ROS production [75]. These basic clinical findings suggest that increased oxidative stress caused by smoking may contribute to vascular endothelial function. Increased oxidative stress due to smoking contributes to atherosclerosis by inducing cell proliferation, cell hypertrophy, and apoptosis, either directly through vascular endothelial damage or through activation of various intracellular signaling pathways. Furthermore, the onset of atherosclerosis feeds back to itself and aggravates the condition, making a vicious cycle that leads to the maintenance and progression of atherosclerosis.
Involvement of Rho-associated kinase (ROCK)
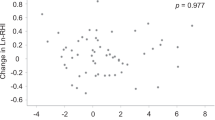
The Rho family (Pho, Cdc42, Rac, and Rnd) belongs to the Ras superfamily of low molecular weight G proteins and is a major regulator of the actin cytoskeleton [76,77,78,79,80]. It is essential for vascular smooth muscle contraction, cell adhesion, cell death, cell division, and other processes of vascular formation. Furthermore, the RhoA/ROCK pathway plays an important role in the onset, maintenance, and progression of vascular injury through vasoconstriction and remodeling [81, 82]. It has been reported that plasminogen activator inhibitor-1 gene expression in endothelial cells and vascular remodeling are normalized by ROCK inhibitor treatment in atherosclerosis models [83, 84]. We confirmed that ROCK was activated in smokers and that ROCK activity was significantly correlated with FMD in smokers [85,86,87]. Although the detailed mechanism of smoking-induced activation of ROCK is not clear, smoking is thought to be directly involved in Rho activation. ROCK activation is known to be directly associated with decreased eNOS activity through reduced eNOSmRNA stability and inhibition of Akt phosphorylation [88]. Smoking-induced ROCK activation is associated with decreased eNOS activity and making a vicious cycle that may lead to further vascular endothelial dysfunction.
Smoking cessation and vascular endothelial function
Unfortunately, there is little information on the effects of smoking cessation on endothelial function. Even taking into account publication bias, the number of published papers is very small. This may be due in part to the difficulty of smoking cessation. From 1998 to 2022, there were 23 studies in which the effects of smoking cessation on endothelial function in smokers were evaluated (Table 1) [18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35, 89,90,91,92,93]. Many studies including our studies have clearly shown that smoking is associated with endothelial dysfunction [42,43,44,45,46,47,48]. Therefore, it is strongly expected that smoking cessation will improve endothelial function. However, not all of the studies showed beneficial effects of smoking cessation on endothelial function. There were three studies using a prospective, double-blind, randomized, and placebo-control design [22, 89, 90]. Johnson et al. [22]. Showed that smoking cessation for one year improved FMD in the brachial artery in 1504 cigarette smokers. Mah et al. [89, 90]. Showed in two studies that smoking cessation alone did not improve FMD in healthy young cigarette smokers during smoking cessation for 7 days (n = 135) and for 24 h (n = 12), while smoking cessation with γ-tocopherol-rich supplementation improved FMD in both studies. Although 12 of 15 studies in which the effects of smoking cessation on vascular endothelial function was assessed by physiological methods including measurements of FMD and reactive hyperemia index (RHI) showed that smoking cessation improved FMD, RHI or vascular response to vasoactive agents [18, 21, 22, 25,26,27,28,29, 32,33,34,35], three of those 15 studies showed no effects of smoking cessation on FMD or RHI [89,90,91]. In eight studies in which the effects of smoking cessation on endothelial function were assessed by biomarkers[19, 20, 23, 24, 30, 31, 92, 93], five studies showed that smoking cessation increased or improved biomarkers for endothelial function including circulating levels of nitrate/nitrite, NO, vvWF, ICAM-1, EPCs and EMPs and activity of eNOS [19, 23, 24, 30, 31]. However, three of the eight studies showed no effects of smoking cessation on biomarkers for endothelial function [20, 92, 93]. In any case, there has been no report of smoking cessation worsening endothelial function.
The reasons of the discrepant results of studies remain unclear. Depending on the degree of vascular endothelial dysfunction caused by smoking, smoking cessation is expected to improve vascular endothelial function as long as the impairment is not irreversible. Indeed, although many studies have clearly shown that several interventions including pharmacological therapy and lifestyle modifications improve endothelial function under the condition of relatively mild vascular endothelial dysfunction [8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35], we have shown that advanced endothelial dysfunction is not reversible even by appropriate pharmacological therapy [94]. Daily smoking amount, duration of smoking, duration of cessation, and background of individuals may play a critical role in the impact of smoking cessation on endothelial function. The method used for quitting smoking may also be important. The use of nicotine, bupropion, varenicline and e-cigarettes as an aid in smoking cessation may result in alteration of endothelial function. There were 15 studies on the use of nicotine replacement [19, 20, 22,23,24, 29,30,31,32,33,34,35, 90,91,92], and four of 14 studies showed that smoking cessation did not alter circulating NOx levels [92], improved the function of EPCs but not the number of EPCs [24], did not improve FMD [91], and improved FMD but not RHI [34]. In two of six studies on the use of varenicline, smoking cessation did not improve endothelial function [34, 93]. In only one study on the use of bupropion, smoking cessation decreased plasma ICAM-l levels but not vWF levels [20]. It has been shown that e-cigarettes per se has harmful effects on endothelial function [95, 96]. However, in both of the two studies on the use of e-cigarettes in combination with nicotine replacement, smoking cessation improved vascular function [33, 35]. In addition, effects of smoking cessation on endothelial function may differ by sex, age, and risk severity of the subject. Further studies are needed to confirm the effects of smoking cessation on endothelial function using an appropriate study design, several smoking cessation methods, short- to long-term follow-up periods, different grades of smoking status, and diverse subjects including subjects with advanced atherosclerosis and healthy subjects in large clinical trials.
Conclusions
It is clear that smoking impairs vascular endothelial function and leads to atherosclerosis. Smoking cessation is expected to improve vascular endothelial function. However, the effects of smoking cessation on vascular endothelial function are not always consistent. In addition, the number of studies on the relationship between smoking cessation and vascular endothelial function is overwhelmingly small. Further studies are needed to elucidate the detailed mechanisms by which smoking induces endothelial dysfunction and to determine whether smoking cessation directly improves endothelial function.
References
Doll R, Peto R, Wheatley K, Gray R, Sutherland I. Mortality in relation to smoking: 40 years’ observations on male British doctors. Br Med J. 1994;309:901–11.
Rigotti NA, Pasternak RC. Cigarette smoking and coronary heart disease: risks and management. Cardiol Clin. 1996;14:51–68.
Ambrose JA, Barua RS. The pathophysiology of cigarette smoking and cardiovascular disease: an update. J Am Coll Cardiol. 2004;43:1731–7.
Hadley MB, Henderson SB, Brauer M, Vedanthan R. Protecting cardiovascular health from wildfire smoke. Circulation. 2022;146:788–801.
Ross R. Atherosclerosis-an inflammatory disease. N Engl J Med. 1999;340:115–26.
Higashi Y, Noma K, Yoshizumi M, Kihara Y. Endothelial function and oxidative stress in cardiovascular diseases. Circ J. 2009;73:411–8.
Higashi Y, Yoshizumi M. Exercise and endothelial function: role of endothelium-derived nitric oxide and oxidative stress in healthy subjects and hypertensive patients. Exercise and endothelial function: role of endothelium-derived nitric oxide and oxidative stress in healthy subjects and hypertensive patients. Pharm Ther. 2004;102:87–96.
Schiffrin EL, Deng LY. Comparison of effects of angiotensin I-converting enzyme inhibition and ß-blockade for 2 years on function of small arteries from hypertensive patients. Hypertension. 1995;25:699–703.
Higashi Y, Sasaki S, Nakagawa K, Kurisu S, Yoshimizu A, Matsuura H, et al. A comparison of angiotensin-converting enzyme inhibitors, calcium antagonists, beta-blockers, diuretics on reactive hyperemia in patients with essential hypertension: a multicenter study. J Am Coll Cardiol. 2000;35:284–91.
Wolfrum S, Jensen KS, Liao JK. Endothelium-dependent effects of statins. Arterioscler Thromb Vasc Biol. 2003;23:729–36.
Fujimura N, Hata T, Soga J, Hidaka T, Idei N, Fujii Y, et al. Selective mineralocorticoid receptor blocker eplerenone improves endothelial function and inhibits Rho-associated kinase activity in patients with essential hypertension. Clin Pharm Ther. 2012;91:289–97.
Sanada M, Higashi Y, Sasaki S, Nakagawa K, Kodama I, Tsuda M, et al. Relationship between the angiotensin-converting enzym genotype and forearm vasodilatior response to estrogen replacement therapy in postmenopausal. J Am Coll Cardiol. 2001;37:1529–35.
Higashi Y, Sasaki S, Nakagawa K, Fukuda Y, Matsuura H, Oshima T, et al. Tetrahydrobiopterin improves impaired endothelium-dependent vasodilation in patients with essential hypertension. Am J Hypertens. 2002;15:326–32.
Goto C, Higashi Y, Kimura M, Noma K, Hara K, Nakagawa K, et al. The effect of different intensities of exercise on endothelium-dependent vasodilation in humans: role of endothelium-dependent nitric oxide and oxidative stress. Circulation. 2003;108:530–5.
Hambrecht R, Wolf A, Gielen S, Linke A, Hofer J, Erbs S, et al. Effect of exercise on coronary endothelial function in patients with coronary artery disease. N Engl J Med. 2000;342:454–60.
Sasaki S, Higashi Y, Nakagawa K, Kimura M, Noma K, Sasaki S, et al. A low-calorie diet improves endothelium-dependent vasodilation in obese patients with essential hypertension. Am J Hypertens. 2002;15:302–9.
Bragulat E, de la Sierra A, Antonio MT, Coca A. Endothelial dysfunction in salt-sensitive essential hypertension. Hypertension. 2001;37:444–8.
Moreno H Jr, Chalon S, Urae A, Tangphao O, Abiose AK, Hoffman BB, et al. Endothelial dysfunction in human hand veins is rapidly reversible after smoking cessation. Am J Physiol. 1998;275:H1040–5.
Kondo T, Hayashi M, Takeshita K, Numaguchi Y, Kobayashi K, Iino S, et al. Smoking cessation rapidly increases circulating progenitor cells in peripheral blood in chronic smokers. Arterioscler Thromb Vasc Biol. 2004;24:1442–7.
Halvorsen B, Lund Sagen E, Ueland T, Aukrust P, Tonstad S. Effect of smoking cessation on markers of inflammation and endothelial cell activation among individuals with high risk for cardiovascular disease. Scand J Clin Lab Invest. 2007;67:604–11.
Hosokawa S, Hiasa Y, Miyazaki S, Ogura R, Miyajima H, Ohara Y, et al. Effects of smoking cessation on coronary endothelial function in patients with recent myocardial infarction. Int J Cardiol. 2008;128:48–52.
Johnson HM, Gossett LK, Piper ME, Aeschlimann SE, Korcarz CE, Baker TB, et al. Effects of smoking and smoking cessation on endothelial function: 1-year outcomes from a randomized clinical trial. J Am Coll Cardiol. 2010;55:1988–95.
Caponnetto P, Russo C, Di Maria A, Morjaria JB, Barton S, Guarino F, et al. Circulating endothelial-coagulative activation markers after smoking cessation: a 12-month observational study. Eur J Clin Invest. 2011;41:616–26.
Puls M, Schroeter MR, Steier J, Stijohann L, Hasenfuss G, Konstantinides S, et al. Effect of smoking cessation on the number and adhesive properties of early outgrowth endothelial progenitor cells. Int J Cardiol. 2011;152:61–9.
Umeda A, Kato T, Yamane T, Yano H, Ieiri T, Miyagawa K, et al. Does smoking cessation with varenicline worsen vascular endothelial function? BMJ Open. 2013;3:e003052.
Sugiura T, Dohi Y, Hirowatari Y, Yamashita S, Ohte N, Kimura G, et al. Cigarette smoking induces vascular damage and persistent elevation of plasma serotonin unresponsive to 8 weeks of smoking cessation. Int J Cardiol. 2013;166:748–9.
Kato T, Umeda A, Miyagawa K, Takeda H, Adachi T, Toyoda S, et al. Varenicline-assisted smoking cessation decreases oxidative stress and restores endothelial function. Hypertens Res. 2014;37:655–8.
Kobayashi M, Takemoto Y, Norioka N, Iguchi T, Shimada K, Maeda M, et al. Vascular functional and morphological alterations in smokers during varenicline therapy. Osaka City Med J. 2015;61:19–30.
Taylor BA, Zaleski AL, Dornelas EA, Thompson PD. The impact of tetrahydrobiopterin administration on endothelial function before and after smoking cessation in chronic smokers. Hypertens Res. 2016;39:144–50.
Wang J, Zhao L, Wei J, Zhang S, Chen N, Ding D, et al. Comparison of various strategies for the prognosis and outcomes of ischaemic dilated cardiomyopathy in smokers: complete revascularisation and smoking cessation produces a superior outcome. Heart Lung Circ. 2017;26:463–76.
Ikonomidis I, Marinou M, Vlastos D, Kourea K, Andreadou I, Liarakos N, et al. Effects of varenicline and nicotine replacement therapy on arterial elasticity, endothelial glycocalyx and oxidative stress during a 3-month smoking cessation program. Atherosclerosis. 2017;262:123–30.
Xue C, Chen QZ, Bian L, Yin ZF, Yin ZF, Xu ZJ, et al. Effects of smoking cessation with nicotine replacement therapy on vascular endothelial function, arterial stiffness, and inflammation response in healthy smokers. Angiology. 2019;70:719–25.
Klonizakis M, Gumber A, McIntosh E, Brose LS. Short-term cardiovascular effects of E-cigarettes in adults making a stop-smoking attempt: a randomized controlled trial. Biology (Basel). 2021;10:1208.
Fukumoto K, Takemoto Y, Norioka N, Takahashi K, Namikawa H, Tochino Y, et al. Predictors of the effects of smoking cessation on the endothelial function of conduit and digital vessels. Hypertens Res. 2021;44:63–70.
Klonizakis M, Gumber A, McIntosh E, Brose LS. Medium- and longer-term cardiovascular effects of e-cigarettes in adults making a stop-smoking attempt: a randomized controlled trial. BMC Med. 2022;20:276.
Eagles CJ, Martin U. Non-pharmacological modification of cardiac risk factors: part 3. Smoking cessation and alcohol consumption. J Clin Pharm Ther. 1998;23:1–9.
Saladini F, Benetti E, Fania C, Mos L, Casiglia E, Palatini P. Effects of smoking on central blood pressure and pressure amplification in hypertension of the young. Vasc Med. 2016;21:422–8.
Sambola A, Osende J, Hathcock J, Degen M, Nemerson Y, Fuster V, et al. Role of risk factors in the modulation for tissue factor activity and blood thrombogenicity. Circulation. 2003;107:973–7.
Craig WY, Palomaki GE, Haddow JE. Cigarette smoking and serum lipid and lipoprotein concentrations: an analysis of published data. BMJ. 1989;298:784–8.
Nakamura K, Barzi F, Huxley R, Lam TH, Suh I, Woo J.Asia Pacific Cohort Studies Collaboration. Pacific Cohort Studies Collaboration. et al. Does cigarette smoking exacerbate the effect of total cholesterol and high-density lipoprotein cholesterol on the risk of cardiovascular diseases?. Heart. 2009;95:909–16.
Barua RS, Ambrose JA, Saha DC, Eales-Reynolds LJ. Smoking is associated with altered endothelial-derived fibrinolytic and antithrombotic factors: an in vitro demonstration. Circulation. 2002;106:905–8.
Celermajer DS, Sorensen KE, Georgakopoulos D, Bull C, Thomas O, Robinson J, et al. Cigarette smoking is associated with dose-related and potentially reversible impairment of endothelium-dependent dilation in healthy young adults. Circulation. 1993;88:2149–55.
Kiowski W, Linder L, Stoschitzky K, Pfisterer M, Burckhardt D, Burkart F, et al. Diminished vascular response to inhibition of endothelium-derived nitric oxide and enhanced vasoconstriction to exogenously administered endothelin-1 in clinically healthy smokers. Circulation. 1994;90:27–34.
Zeiher AM, Schachinger V, Minners J. Long-term cigarette smoking impairs endothelium-dependent coronary arterial vasodilator function. Circulation. 1995;92:1094–110.
Heitzer T, Yla-Herttuala S, Luoma J, Kurz S, Münzel T, Just H, et al. Cigarette smoking potentiates endothelial dysfunction of forearm resistance vessels in patients with hypercholesterolemia. Role of oxidized LDL. Circulation. 1996;93:1346–53.
Kimura M, Higashi Y, Hara K, Noma K, Sasaki S, Nakagawa K, et al. PDE5 inhibitor sildenafil citrate augments endothelium-dependent vasodilation in smokers. Hypertension. 2003;41:1106–10.
Nakamura S, Kimura M, Goto C, Noma K, Yoshizumi M, Chayama K, et al. Cigarette smoking abolished ischemic preconditioning-induced augmentation of endothelium-dependent vasodilation. Hypertension. 2009;53:674–81.
Hashimoto H, Maruhashi T, Yamaji T, Harada T, Han Y, Takaeko Y, et al. Smoking status and endothelial function in Japanese men. Sci Rep. 2021;11:95.
Kawachi I, Colditz GA, Stampfer MJ, Willett WC, Manson JE, Rosner B, et al. Smoking cessation in relation to total mortality rates in women. A prospective cohort study. Ann Inter Med. 1993;119:992–1000.
Daly LE, Mulcahy R, Graham M, Hickey N. Long term effect on mortality of stopping smoking after unstable angina and myocardial infarction. Br Med J. 1983;287:324–6.
Lüscher TF. Imbalance of endothelium-derived relaxing and contracting factors. Am J Hypertens. 1990;3:317–30.
Vane JR, Anggard EE, Botting RM. Regulatory functions of the vascular endothelium. N Engl J Med. 1990;323:27–36.
Vanhoutte PM. Endothelium and control of vascular function: state of the art lecture. Hypertension. 1989;13:658–67.
Ota Y, Kugiyama K, Sugiyama S, Ohgushi M, Matusmura T, Doi H, et al. Impairment of endothelium-dependent relaxation of rabbit aortas by cigarette smoke extract: role of free radicals and attenuation by captopril. Atherosclerosis. 1997;131:195–202.
Nene S, Gelabert HA, Moore W, Quinones-Baldrich W, Santibanez-Gallerani A, Ignarro L. Cigarette smoking increases endothelium-derived vasorelaxation in the rat carotid artery in a dose-dependent manner. J Surg Res. 1997;71:101–6.
Kugiyama K, Yasue H, Ohgushi M, Motoyama T, Kawano H, Inobe Y, et al. Deficiency in nitric oxide bioactivity in epicardial coronary arteries of cigarette smokers. Am Coll Cardiol. 1996;28:1161–7.
Celermajer DS, Adams MR, Clarkson P, Robinson J, McCredie R, Donald A, et al. Passive smoking and impaired endothelium-dependent arterial dilatation in healthy young adults. N Engl J Med. 1996;334:150–4.
Sumida H, Watanabe H, Kugiyama K, Ohgushi M, Matsumura T, Yasue H. Does passive smoking impair endothelium-dependent coronary artery dilation in women? J Am Coll Cardiol. 1998;31:811–5.
Maruhashi T, Soga J, Idei N, Fujimura N, Mikami S, Iwamoto Y, et al. Relationship between flow-mediated vasodilatation and cardiovascular risk factors in a large community-based study. Heart. 2013;99:1837–42.
Delgado GE, Kramer BK, Siekmeier R, Yazdani B, März W, Leipe J, et al. Influence of smoking and smoking cessation on biomarkers of endothelial function and their association with mortality. Atherosclerosis. 2020;292:52–59.
Münzel T, Hahad O, Kuntic M, Keaney JF, Deanfield JE, Daiber A. Effects of tobacco cigarettes, e-cigarettes, and waterpipe smoking on endothelial function and clinical outcomes. Eur Heart J. 2020;41:4057–70.
Serban KA, Rezania S, Petrusca DN, Poirier C, Cao D, Justice MJ, et al. Structural and functional characterization of endothelial microparticles released by cigarette smoke. Sci Rep. 2016;6:31596.
Rodella LF, Favero G, Rossini C, Foglio E, Reiter RJ, Rezzani R. Endothelin-1 as a potential marker of melatonin’s therapeutic effects in smoking-induced vasculopathy. Life Sci. 2010;87:558–64.
Rajagopalan S, Kurz S, Münzel T, Tarpey M, Freeman BA, Griendling KK, et al. Angiotensin II-mediated hypertension in the rat increases vascular superoxide production via membrane NADH/NADPH oxidase activation. J Clin Invest. 1996;97:1916–23.
Irani k. Oxidant signaling in vascular cell growth, death and survival: a review of the roles of reactive oxygen species in smooth muscle and endothelial cell mitogenic and apoptotic signaling. Cir Res. 2000;87:179–83.
Cai H, Harrison DG. Endothelial dysfunction in cardiovascular diseases: the role of oxidant stress. Circ Res. 2000;87:840–4.
Burke A, Fitzgerald GA. Oxidative stress and smoking-induced vascular injury. Prog Cardiovasc Dis. 2003;46:79–90.
Kuzkaya N, Weissmann N, Harrison DG, Dikalov S. Interactions of peroxynitrite, tetrahydrobiopterin, ascorbic acid, and thiols: implications for uncoupling endothelial nitric-oxide synthase. J Biol Chem. 2003;278:22546–54.
Ushio-Fukai M, Zafari AM, Fukui T, Nishizaka N, Griendling KK. p22phox is a critical component of the superoxide-generating NADH/NADPH oxidase system and regulates angiotensin II-induced hypertrophy in vascular smooth muscle cells. J Biol Chem. 1996;271:23317–21.
Higashi Y, Sasaki S, Nakagawa K, Matsuura H, Oshima T, Chayama K. Endothelial function and oxidative stress in renovascular hypertension. N Engl J Med. 2002;346:1954–62.
Tsuchiya M, Asada A, Kasahara E, Sato EF, Shindo M, Inoue M. Smoking a single cigarette rapidly reduces combined concentrations of nitrate and nitrite and concentrations of antioxidants in plasma. Circulation. 2002;105:1155–7.
Barua RS, Ambrose JA, Srivastava S, DeVoe MC, Eales-Reynolds LJ. Reactive oxygen species are involved in smoking-induced dysfunction of nitric oxide biosynthesis and upregulation of endothelial nitric oxide synthase: an in vitro demonstration in human coronary artery endothelial cells. Circulation. 2003;107:2342–7.
Guthikonda S, Sinkey C, Barenz T, Haynes WG. Xanthine oxidase inhibition reverses endothelial dysfunction in heavy smokers. Circulation. 2003;107:416–21.
Heitzer T, Just H, Munzel T. Antioxidant vitamin C improves endothelial dysfunction in chronic smokers. Circulation. 1996;94:6–9.
Higman DJ, Stracchan AMJ, Buttery L, Hicks RC, Springall DR, Greenhalgh RM, et al. Smoking impairs the activity of endothelial nitric oxide synthase in saphenous vein. Arterioscler Thromb Vasc Biol. 1996;16:546–52.
Kimura K, Ito M, Amano M, Chihara K, Fukata Y, Nakafuku M, et al. Regulation of myosin phosphatase by Rho and Rho-associated kinase (Rho-kinase). Science. 1996;273:245–8.
Uehata M, Ishizaki T, Satoh H, Ono T, Kawahara T, Morishita T, et al. Calcium sensitization of smooth muscle mediated by a Rho-associated protein kinase in hypertension. Nature. 1997;389:990–4.
Amano M, Chihara K, Kimura K, Fukata Y, Nakamura N, Matsuura Y, et al. Formation of actin stress fibers and focal adhesions enhanced by Rho-kinase. Science. 1997;275:1308–11.
Hoshijima M, Sah VP, Wang Y, Chien KR, Brown JH. The low molecular weight GTPase Rho regulates myofibril formation and organization in neonatal rat ventricular myocytes. Involvement of Rho kinase. J Biol Chem. 1998;273:7725–30.
Wei L, Imanaka-Yoshida K, Wang L, Zhan S, Schneider MD, DeMayo FJ, et al. Inhibition of Rho family GTPases by Rho GDP dissociation inhibitor disrupts cardiac morphogenesis and inhibits cardiomyocyte proliferation. Development. 2002;129:1705–14.
Brown JH, Del Re DP, Sussman MA. The Rac and Rho hall of fame: a decade of hypertrophic signaling hits. Circ Res. 2006;98:730–42.
Shimokawa H, Sunamura S, Satoh K. RhoA/Rho-kinase in the cardiovascular system. Circ Res. 2016;118:352–66.
Rikitake Y, Liao JK. Rho-kinase mediates hyperglycemia-induced plasminogen activator inhibitor-1 expression in vascular endothelial cells. Circulation. 2005;111:3261–8.
Zhou Q, Gensch C, Liao JK. Rho-associated coiled-coil-forming kinases (ROCKs): potential targets for the treatment of atherosclerosis and vascular disease. Trends Pharm Sci. 2011;32:167–73.
Noma K, Higashi Y, Jitsuiki D, Hara K, Kimura M, Nakagawa K, et al. Smoking activates Rho-kinase in smooth muscle cells of forearm vasculature in humans. Hypertension. 2003;41:1102–5.
Noma K, Goto C, Jitsuiki D, Ueda K, Kimura M, Nishioka K, et al. Smoking, endothelial function, and Rho-kinase in humans. Arterioscler Thromb Vasc Biol. 2005;25:2630–5263.
Hidaka T, Hata T, Soga J, Nakamura S, Fujii Y, Idei N, et al. Increased leukocyte Rho kinase (ROCK) and endothelial dysfunction in cigarette smokers. Hypertens Res. 2010;33:354–9.
Noma K, Oyama N, Liao JK. Physiological role of ROCKs in the cardiovascular system. Am J Physiol Cell Physiol. 2006;290:C661–8.
Mah E, Pei R, Guo Y, Ballard KD, Barker T, Rogers VE, et al. γ-Tocopherol-rich supplementation additively improves vascular endothelial function during smoking cessation. Free Radic Biol Med. 2013;65:1291–9.
Mah E, Pei R, Guo Y, Masterjohn C, Ballard KD, Taylor BA, et al. Greater γ-tocopherol status during acute smoking abstinence with nicotine replacement therapy improved vascular endothelial function by decreasing 8-iso-15(S)-prostaglandin F2α. Exp Biol Med (Maywood). 2015;240:527–33.
Jodoin I, Bussières LM, Tardif JC, Juneau M. Effect of a short-term primary prevention program on endothelium-dependent vasodilation in adults at risk for atherosclerosis. Can J Cardiol. 1999;15:83–88.
Miller VM, Lewis DA, Rud KS, Offord KP, Croghan IT, Hurt RD. Plasma nitric oxide before and after smoking cessation with nicotine nasal spray. J Clin Pharm. 1998;38:22–7.
Strulovici-Barel Y, Staudt MR, Krause A, Gordon C, Tilley AE, Harvey BG, et al. Persistence of circulating endothelial microparticles in COPD despite smoking cessation. Thorax. 2016;71:1137–44.
Higashi Y, Sasaki S, Nakagawa K, Kimura M, Noma K, Sasaki S, et al. The severity of hypertension affects improved resistance artery endothelial function by angiotensin converting enzyme inhibition. J Cardiovasc Pharm. 2002;39:668–76.
Carnevale R, Sciarretta S, Violi F, Nocella C, Loffredo L, Perri L, et al. Acute impact of tobacco vs electronic cigarette smoking on oxidative stress and vascular function. Chest. 2016;150:606–12.
Mohammadi L, Han DD, Xu F, Huang A, Derakhshandeh R, Rao P, et al. Chronic E-cigarette use impairs endothelial function on the physiological and cellular levels. Arterioscler Thromb Vasc Biol. 2022;42:1333–50.
Acknowledgements
I thank Megumi Wakisaka, Ki-ichiro Kawano, and Satoko Michiyama for their excellent secretarial assistance.
Funding
This work was supported by the Grant-in-Aid for Scientific Research from the Ministry of Education, Science and Culture of Japan (18590815 and 21590898) and a Grant in Aid of Japanese Arteriosclerosis Prevention Fund.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Higashi, Y. Smoking cessation and vascular endothelial function. Hypertens Res 46, 2670–2678 (2023). https://doi.org/10.1038/s41440-023-01455-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-023-01455-z