Abstract
Although social jetlag (SJL) is generally considered a chronic condition, even acute SJL may have unfavorable effects on the cardiovascular system. We focused on the acute effects of SJL on morning blood pressure (BP) surge. This randomized crossover trial recruited 20 healthy men. In the SJL trial, participants delayed their bedtime by three hours on Friday and Saturday nights. Participants in the control (CON) trial implemented the same sleep-wake timing as on weekdays. Pre- and post-intervention measurements were performed to evaluate resting cardiovascular variables on Friday and Monday mornings, respectively. The ambulatory BP was automatically measured during the sleep and awake periods for 2 h after the participant woke up at night before pre- and post-intervention measurements. SJL (average mid-sleep time on weekends – average mid-sleep time on weekdays) occurred only in the SJL trial (SJL: 181 ± 24 min vs. CON: 8 ± 47 min). Carotid-femoral pulse wave velocity (cfPWV) and morning BP surge on Monday in the SJL trial were significantly higher than those on Friday in the SJL trial (cfPWV: P = 0.001, morning BP surge: P < 0.001), and those on Monday in the CON trial (cfPWV: P = 0.007; morning BP surge: P < 0.001). Furthermore, a significant positive correlation was found between ΔcfPWV and Δmorning BP surge (R = 0.587, P = 0.004). These results suggest that even acute SJL augments morning BP surge. This phenomenon may correspond to increased central arterial stiffness.
State the details of Clinical Trials: Name: Effect of acute social jetlag on risk factors of lifestyle-related diseases. URL: https://center6.umin.ac.jp/cgi-open-bin/ctr_e/ctr_view.cgi?recptno=R000053204. Unique identifier: UMIN000046639. Registration date: 17/01/2022

Similar content being viewed by others
Introduction
The discrepancy in sleep–wake timing between workdays and free (non-work) days due to modern work schedules possibly causes mild circadian misalignment between endogenous circadian rhythm and the sleep schedule imposed by social obligations. This jetlag-like phenomenon is called “social jetlag (SJL),” [1] which is measured as the differences between mid-sleep time on workdays and free days [1, 2]. SJL is prevalent in the general population [3,4,5] and has been suggested to lead to cardiovascular diseases [6, 7]. Although SJL is generally considered a chronic condition [3,4,5], even acute SJL may have unfavorable effects on the cardiovascular system, given that the simulated jetlag due to air travel acutely affects the cardiovascular system in an animal study [8]. To the best of our knowledge, no evidence shows that acute SJL influences the cardiovascular system in humans.
In humans, blood pressure (BP) shows circadian variations; it decreases during sleep and increases in the morning [9, 10]. The diurnal variation in pressure stress from the nadir during sleep to the peak in the morning is called the morning BP surge. A normal morning BP surge is a physiological phenomenon, whereas an exaggerated morning BP surge is an independent predictor of cardiovascular events [11, 12]. Interestingly, the morning BP surge has a weekly variation and is most significant on Monday [13]. In modern society, many people work on weekdays (Monday to Friday) and take a day off on weekends (Saturday and Sunday); thus, the weekly variation may be influenced by acute SJL on weekends.
Thus, the purpose of the present study was to investigate the acute effects of SJL on morning BP surge. As an unhealthy lifestyle on free days, such as excess intake of energy as well as reduced physical activity levels, may confound the effects of SJL, we designed a randomized crossover trial to eliminate these potential confounding effects. We hypothesized that even acute SJL augments morning BP surge. Furthermore, the present study evaluated the effects of acute SJL on other cardiovascular variables and the autonomic nervous system, such as central arterial stiffness and sympathetic nerve activity in a vessel, to elucidate the underlying physiological mechanisms of the morning BP surge due to acute SJL.
Materials and methods
Participants
Twenty healthy men were recruited to participate in this study. All participants did not have a history of hypertension (systolic BP [SBP] ≤ 140 and diastolic BP [DBP] ≤ 90 mmHg), were nonsmokers, and were free of overt cardiovascular disease or diabetes, as assessed by medical history. All participants provided written informed consent to participate before the start of this study. The purpose, procedures, and risks involved in this study were reviewed and approved by the Human Research Committee of Waseda University (approval No. 2021-214). This study was conducted according to the guidelines of the 1975 Declaration of Helsinki.
Experimental design
The present study was an open-label, randomized crossover trial consisting of the SJL and control (CON) trials (Figure S1). The study protocol is registered in the University Hospital Medical Information Network-Clinical Trial Registry (number: UMIN000046639, registration date: 17/01/2022). The present study shows a part of the primary outcomes listed in the registered protocol. Figure S2 shows the schedule of the present study. The participants were randomly assigned to the CON or SJL trials after the screening term. One investigator was responsible for the randomization and allocation of the participants to two trials. The allocation list was created using spreadsheet software (Microsoft Excel, Microsoft, WA, USA).
After written informed consent was obtained, wearable devices (Fitbit Charge 5, Fitbit, CA, USA) were distributed to the participants to monitor sleep variables and energy balance throughout this study. The device automatically measures bedtime, awake time, sleep duration (percentage of time in rapid eye movement [REM], light and deep sleep), and daily total energy expenditure. The validity of Fitbit Charge series for measuring the sleep variables has been confirmed by comparison with polysomnography and actigraphy [14, 15]. The energy expenditure for every 5 min was extracted, and the amount of physical activity for 2 h before and after awake time was calculated from the energy expenditure. The participants were instructed about the correct usage of the device (Fitbit: Health & Fitness, Fitbit, CA, USA) and to record food intake by themselves. The participants were allotted a period to familiarize themselves with the device and the application. We required the participants to wear the device during the intervention period, except for bathing. The intervention was conducted for 4 weeks, as described below.
Week one
We started with a screening term to confirm sleep variables (bedtime, awake time, and mid-sleep time [median time between bedtime and awake time]) under free-living conditions for each participant from Wednesday in week one to Tuesday in week two. We confirmed that day-to-day intraindividual variation in mid-sleep time on weekdays was within 2 h.
Week two
Resting hemodynamics, autonomic nervous system, cardiovagal baroreflex sensitivity (cvBRS), and central arterial stiffness were measured on Friday morning as pre-intervention measurement one. The participants were required to perform the SJL or CON trial from Friday night to Sunday morning.
Week three
Post-intervention measurement one was conducted on Monday morning, as with pre-intervention measurement one. Afterward, the participants were required to live according to everyday routine until Thursday as a washout term. Pre-intervention measurement two was conducted on Friday morning. The participants were then crossed over to the opposite trial and were instructed to have the same meal and to perform physical activity as per the last weekend to avoid the confounding effect of energy expenditure and intake.
Week four
Post-intervention measurement two was performed on Monday morning. After that, the participants were required to live according to routine life until Thursday as a follow-up.
Social jetlag and control trials
In the SJL trial, the participants were required to delay their bedtime by 3 h on Friday and Saturday nights in week two or three (Figure S3). The participants in the CON trial were instructed to implement the same sleep–wake timing as on weekdays. These sleep–wake timings during the intervention were based on those during the screening term. SJL was calculated as follows: SJL (min) = average mid-sleep time on weekends in week two or three – average mid-sleep time on weekdays in the screening term.
Pre- and post-intervention measurements
Pre- and post-intervention measurements were performed on Friday and Monday mornings; the participants were tested at the same time of day throughout the study period to avoid potential diurnal variations. Before these measurements, the participants were instructed to avoid food and caffeine and alcohol intake for at least 12 and 24 h, respectively. Pre- and post-intervention measurements were conducted under comfortable laboratory conditions between 09:00 AM and 11:00 AM.
Body composition
The percentage of body fat and lean body mass was measured using bioelectrical impedance analysis (InBody 720, InBody, Tokyo, Japan) with the participants in the upright position. The validity of the device for measuring body composition has been confirmed by comparison with dual-energy x-ray absorptiometry, which is the gold standard for measuring body composition [16,17,18].
Central arterial stiffness
The participants were studied under quiet resting conditions for 10 min in the supine position. Carotid-femoral pulse wave velocity (cfPWV), which is the gold standard for measuring central arterial stiffness [19, 20], was measured using a vascular testing device (form PWV/ABI, Omron Colin, Tokyo, Japan). Carotid arterial pressure waveforms were stored for 30 s using applanation tonometry sensors attached to the right common carotid and common right femoral arteries. The value of cfPWV was calculated using the length from the heart to the common carotid (Lhc) and common femoral arteries (Lhf) and the transit time (Tcf): [21]
The coefficient of variation for the cfPWV was 4.9 ± 4.1% within the same participant.
Ambulatory blood pressure and heart rate
The ambulatory BP monitoring (ABPM) device (TM-2441, A&D Medical, Tokyo, Japan) automatically measured ambulatory BP and heart rate (HR) using the oscillometric method every 30–60 min during the sleep and awake period until measurement was completed for 2 h after wake-up. The ambulatory BP monitoring device has been confirmed to be accurate and fulfilled all ISO 81060-2:2013 standard requirements for ABPM determination in adults [22]. The measurement was automatically performed the night before pre-intervention measurement (Thursday night to Friday morning in weeks two and three) and post-intervention measurement (Sunday night in weeks two and three to Monday morning in weeks three and four).
Sleep BP was defined as the average BP readings during sleep. The lowest BP was defined as the average of three BP readings (1.5 h) during sleep. Preawakening BP was defined as the average BP readings during the 2 h just before awake time (four BP readings). Morning BP was defined as the average BP readings during the first 2 h after the awake time (four BP readings) (Figure S4) [11]. Then, the morning BP surge was calculated as follows: [11]
\({{{{{\rm{Morning}}}}}}\; {{{{{\rm{BP}}}}}}\; {{{{{\rm{surge}}}}}}={{{{{\rm{morning}}}}}}\; {{{{{\rm{systolic}}}}}}\; {{{{{\rm{BP}}}}}}({{{{{\rm{SBP}}}}}})-{{{{{\rm{lowest}}}}}}\; {{{{{\rm{nocturnal}}}}}}\; {{{{{\rm{SBP}}}}}}\)
\({{{{{\rm{Preawakening}}}}}}\; {{{{{\rm{morning}}}}}}\; {{{{{\rm{BP}}}}}}\; {{{{{\rm{surge}}}}}}={{{{{\rm{preawakening}}}}}}\; {{{{{\rm{SBP}}}}}}-{{{{{\rm{lowest}}}}}}\; {{{{{\rm{nocturnal}}}}}}\; {{{{{\rm{SBP}}}}}}\)
\({{{{{\rm{Wakening}}}}}}\; {{{{{\rm{morning}}}}}}\; {{{{{\rm{BP}}}}}}\; {{{{{\rm{surge}}}}}}={{{{{\rm{morning}}}}}}\; {{{{{\rm{SBP}}}}}}-{{{{{\rm{preawakening}}}}}}\; {{{{{\rm{SBP}}}}}}\)
The coefficients of variation for the morning SBP and the lowest nocturnal SBP were 7.1 ± 6.6% and 7.0 ± 7.3% within the same participant, respectively [23].
Cardiovagal baroreflex sensitivity
Spontaneous cardiovagal baroreflex sensitivity (cvBRS) was determined from beat-to-beat changes in R–R interval (RRI) and SBP using an analysis software (Beatscope, version 1.1, Finapres Medical Systems, Amsterdam, The Netherlands). Three or more beats of progressive SBP changes and corresponding changes of RRI were identified as baroreflex sequences. Both were recorded in the present study. The minimum criteria for accepting a sequence were set at 1 mmHg for SBP and 4 ms for RRI. The slope of the linear correlation between RRI and SBP was assessed for up–up (progressive increases of SBP followed by a lengthening of the RRI) and down–down (progressive decreases of SBP with a subsequent shortening of the RRI) cvBRSs, which was determined if the r-value was > 0.8. Both cvBRSs were averaged for each participant for the last 5 min of 10-min rest [24].
HR and BP variabilities
HR variability (HRV) was measured as a reliable quantitative marker to assess the activity of the sympathetic and parasympathetic branches of the autonomic nervous system using HRV analysis module (MLS 310, AD Instruments, New South Wales, Australia). In the time domain, the root mean square of the squared differences of successive RRI (RMSSD) estimates short-term variation of HR caused by parasympathetic activity [25]. In the frequency domain analysis, the variance of the signal is calculated through a short, fast Fourier transform, and, according to the frequency band classification, it is characterized into low-frequency (LF: 0.04–0.15 Hz) and high-frequency (HF: 0.15–0.4 Hz). The power component of the LF band includes sympathetic and parasympathetic influences. HF band is primarily influenced by the efferent activity of the vagal tone [25]. The ratio between normalized LF and HF (LF/HF) is established as an index of the sympathovagal balance [26].
BP variability was assessed as a marker of efferent sympathetic vascular modulation [27]. A previous study has reported that oscillation in the LF component of the SBP power spectral density (LF-SBP) is associated with an increase in the sympathetic drive [28]. The LF-SBP was evaluated in the frequency domain using an analysis module (MLS 370, AD Instruments, New South Wales, Australia), similar with HRV analysis.
Hemodynamics in rest
HR and beat-to-beat BP waveform were monitored using a three-lead electrocardiogram (BSM-2401, Nihon Kohden, Tokyo, Japan) and finger photoplethysmography (Finometer MIDI, Finapres Medical Systems, Amsterdam, The Netherlands), respectively. The latter instrument was attached to the middle finger of the left hand. The BP value obtained from the finger was automatically reconstructed as the brachial BP value (Beatscope, version 1.1, Finapres Medical Systems, Amsterdam, The Netherlands) [29]. The method has been validated by comparison with intra-arterial brachial BP [29]. Furthermore, stroke volume (SV) was calculated based on the obtained BP waveform using the model flow method [30], which incorporates age, height, and body mass and simulates aortic flow waveforms from an arterial pressure signal using a nonlinear three-element model of the aortic input impedance (Beatscope, version 1.1, Finapres Medical Systems, Amsterdam, The Netherlands). The method has been validated by comparison with the thermodilution method [30]. Cardiac output (CO) and total peripheral resistance (TPR) were then calculated as SV × HR and mean arterial pressure (MAP)/CO, respectively. In addition, a carotid pressure waveform was obtained in the right common carotid artery. The pressure waveforms were converted from an oscillometric device (form PWV/ABI, Omron Colin, Komaki, Japan) at a sampling rate of 1000 Hz through an analog/digital converter (PowerLab/16SP, AD Instruments, New South Wales, Australia) and recorded in a device connected to a personal computer (Macbook Pro, Apple, CA, USA). Then, the obtained data were analyzed using an analysis software (LabChart8, AD Instruments, New South Wales, Australia). The carotid arterial pressure was calibrated by equating the carotid DBP and MAP to the brachial artery value [31]. Then, these hemodynamics variables were measured for 60 s after resting in the supine position for 10 min. The coefficient of variation for the carotid SBP was 6.1 ± 4.1% within the same participant.
Statistical analyses
A priori statistical power analysis was performed to determine the sample size needed for the present study using G*Power 3.1.9.6 [32]. We determined that a sample size of 12 was needed to achieve a statistical power (1 − β) of more than 0.80, which was required to reject the null hypothesis, with a large standardized effect size (f = 0.40) and an error probability of 0.05 (α), using a repeated measure two-way analysis of variance (ANOVA) (number of trials = 2, number of measurements = 2). Although the minimum calculated sample size was 12, we recruited 20 participants considering the possibility of discontinued intervention or missing data to measurement errors.
All data are expressed as mean ± standard deviation (SD). Statistical analyses were performed using IBM SPSS Statistics for Mac version 27.0 (IBM Corp., Armonk, N.Y., USA). The effects of time and trials were examined by the two-way repeated-measures ANOVA (trial × time) for participants’ characteristics, ambulatory BP and HR, hemodynamics, baroreflex sensitivity, autonomic nervous system, central arterial stiffness, and morning BP surge. The difference in the time course of ambulatory SBP and physical activity between the trials was also analyzed by the two-way repeated-measures ANOVA. In the case of significant F values, it was analyzed using Bonferroni’s post hoc test. One-way repeated-measures ANOVA was applied to compare the differences in sleep variables, including SJL and energy balance, between weekdays (during the screening term) and weekends (during the screening term, the SJL and CON trials).
Moreover, we calculated the absolute change (Δ) from Friday to Monday in each trial in cfPWV, morning BP surge, and LF-SBP. Then, Pearson’s correlation coefficients were used to assess the relationships between the ΔcfPWV and Δmorning BP surge or ΔLF-SBP, Δmorning BP surge, and ΔLF-SBP. The level of significance for all comparisons was set at P < 0.05.
Results
Data exclusion
Six participants were excluded from this study because four showed SJL of < 2 h in the SJL trial, and the ambulatory BP monitoring device did not work for two participants. Therefore, results were based on the remaining 14 participants who completed all measurements (Figure S1). To assess whether the results were affected by excluding participants, we also analyzed the morning BP surge, cfPWV, and the time course of ambulatory SBP using the data from all participants, including those who did not adhere to the intervention in the SJL trial.
Participants’ characteristics
Table 1 shows the participants’ characteristics of the present study. The two-way ANOVA revealed no significant trial × time interactions for all participant characteristics (body mass F = 3.931, P = 0.069; body mass index [BMI]: F = 4.452, P = 0.055; body fat: F = 0.324, P = 0.579; lean body mass: F = 0.001, P = 0.974; waist circumference: F = 0.784, P = 0.392; intracellular water: F = 0.051, P = 0.825; extracellular water: F = 0.009, P = 0.927).
Sleep variables and energy balance
Sleep variables and energy balance during the screening term, the SJL trial, and the CON trial are summarized in Table 2. One-way ANOVA indicated a significant difference in bedtime, awake time, and mid-sleep time on the weekend in the SJL trial compared with weekdays in the screening term, weekend in the screening term, and CON trial (bedtime: P = 0.014; awake time: P < 0.001; mid-sleep time: P < 0.001). SJL was significantly different in the SJL trial compared with the CON trial (SJL: 181 ± 24 min vs. CON: 8 ± 47 min or weekend in screening term: 27 ± 60 min). On the other hand, there were no significant differences in bedtime, sleep duration, REM sleep, light sleep, deep sleep, energy expenditure, and intake on weekends in the SJL trial compared with weekdays in the screening term (sleep duration: P = 0.588; REM sleep: P = 0.827; light sleep: P = 0.945; deep sleep: P = 0.879; energy expenditure: P = 0.600; energy intake: P = 0.964). No significant differences in sleep variables and energy compared with weekdays in the screening term were observed on the weekend of the CON trial.
Ambulatory blood pressure, heart rate, and physical activity
Table S1 indicates ambulatory BP and HR on Friday and Monday in both trials. There was a significant trial × time interaction in morning SBP and double product (morning SBP: F = 20.066, P = 0.001; morning DBP: F = 5.019, P = 0.043; preawakening DBP: F = 6.809, P = 0.022; preawakening HR: F = 19.343, P = 0.001; morning double product: F = 4.769, P = 0.048; wakening morning BP surge: F = 5.393, P = 0.037). Both variables on Monday in the SJL trial were significantly higher than those on Friday in the SJL trial (morning SBP: P < 0.001; morning double product: P = 0.008) and those on Monday in the CON trial (morning SBP: P < 0.001; morning double product: P = 0.026). In contrast, other ambulatory hemodynamics showed no significant interaction (asleep SBP: F = 1.784, P = 0.204; asleep DBP: F = 0.156, P = 0.700; asleep HR: F = 0.618, P = 0.446; preawakening SBP: F = 3.258, P = 0.094; morning HR: F = 0.004, P = 0.950; the lowest nocturnal SBP: F = 0.001, P = 0.985; preawakening morning BP surge: F = 0.443, P = 0.517).
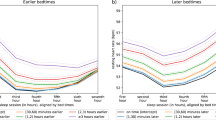
Figure 1 summarizes the difference in the time course of ambulatory SBP (line chart) and physical activity (vertical bar chart) for 2 h before and after an awake time between the trials. We also showed individual data of the time course of ambulatory SBP during CON and SJL trials from Sunday night to Monday morning in Figure S5. Significant trial × time interaction was observed for ambulatory SBP (F = 1.601, P = 0.049). There was no significant trial × time interactions in physical activity (F = 0.072, P = 0.998). Ambulatory SBP on Monday in the SJL trial was significantly higher than that on Friday in the SJL trial at all points after wake-up (0.5 h: P = 0.007; 1 h: P = 0.006; 1.5 h: P = 0.018; 2 h: P = 0.019) and Monday in the CON trial at 1 h and 2 h after wake-up (1 h: P = 0.035; 2 h: P = 0.046). In contrast, the two-way ANOVA revealed no significant trial × time interactions in the time course of ambulatory SBP (F = 1.365, P = 0.132, n = 18) when including those who did not adhere to the intervention in the SJL trial (< 2 h).
Time course of ambulatory systolic blood pressure (line chart) and physical activity (vertical bar chart) for 2 h before and after the awake time (n = 14). A vertical bar line means the awakening point as zero. Line charts show the time course of ambulatory systolic blood pressure as follows: open triangle (△): CON trial on Friday, open circle (○): CON trial on Monday, closed triangle (▲): SJL trial on Friday, closed circle (●): SJL trial on Monday. Vertical bar charts show as follows: white bar: CON trial on Friday, white bar with a black dot: CON trial on Monday, black bar: SJL trial on Friday, black bar with a white dot: SJL trial on Monday. CON, control trial; SBP, systolic blood pressure; SJL, social jetlag trial. Values are presented as mean ± standard deviation. *Significantly different from Friday in the SJL trial at the same point (P < 0.05). †Significantly different from Monday in the CON trial at the same point (P < 0.05)
Hemodynamics, baroreflex sensitivity and autonomic nervous system
Table 3 shows the hemodynamics, baroreflex sensitivity, and autonomic nervous system response to SJL. Significant trial × time interaction was observed for brachial and carotid SBP and TPR (brachial SBP: F = 5.691, P = 0.033; carotid SBP: F = 4.946, P = 0.044; TPR: F = 5.232, P = 0.040). LF-SBP showed significant trial × time interaction (F = 8.023, P = 0.014). Post hoc test revealed that the brachial SBP and LF-SBP on Monday in the SJL trial were significantly higher than those on Friday in the SJL trial (brachial SBP: P = 0.001; LF-SBP: P = 0.015) and those on Monday in the CON trial (brachial SBP: P = 0.003; LF-SBP: P = 0.018). Carotid SBP on Monday in the SJL trial was significantly higher than on Friday in the SJL trial (P = 0.002). There were no significant trial × time interactions with other hemodynamics, baroreflex sensitivity, and autonomic nervous system (brachial DBP: F = 0.641, P = 0.438; MAP: F = 4.092, P = 0.064; carotid PP: F = 3.955, P = 0.068; HR: F = 0.015, P = 0.905; SV: F = 1.145, P = 0.304; CO: F = 1.187, P = 0.296; double product: F = 1.773, P = 0.206; RMSSD: F = 0.078, P = 0.785; LF/HF: F = 1.304, P = 0.274; cvBRS up–up: F = 0.013, P = 0.912; cvBRS down–down: F = 0.225, P = 0.643).
Central arterial stiffness and morning BP
Figure 2 summarizes the data on cfPWV and morning BP surge on Friday and Monday morning in both trials. There were significant trial × time interactions in these variables (cfPWV: F = 4.874, P = 0.046, Fig. 2a; morning BP surge: F = 5.796, P = 0.032, Fig. 2b). Significant differences in both variables were also observed between Monday in the SJL trial (cfPWV: P = 0.001; morning BP surge: P < 0.001) and Monday in the CON trial (cfPWV: P = 0.007; morning BP surge: P = 0.007). However, there was no significant trial × time interaction in the cfPWV and morning BP surge (cfPWV: F = 0.718, P = 0.409, n = 20; morning BP surge: F = 3.193, P = 0.092, n = 18) when including those who did not adhere to the intervention in the SJL trial.
Central arterial stiffness (a), morning blood pressure surge (b) on Friday and Monday morning in both trials (n = 14). White bar: Friday. Black bar: Monday. BP, blood pressure; cfPWV, carotid-femoral pulse wave velocity; CON, control trial; SJL, social jetlag trial. Values are presented as mean ± standard deviation. *Significantly different from Friday in the SJL trial (P < 0.05). †Significantly different from Monday in the CON trial (P < 0.05)
Association between changes in central arterial stiffness, morning BP surge and sympathetic nerve activity in vessels
Figure 3 shows an association between ΔcfPWV and Δmorning BP surge (Fig. 3a) or ΔLF-SBP (Fig. 3b) and Δmorning BP surge and ΔLF-SBP (Fig. 3c). A significant positive correlation was found between ΔcfPWV and Δmorning BP surge (R = 0.587, P = 0.004, Fig. 3a) and ΔLF-SBP (R = 0.438, P = 0.042, Fig. 3b). However, no significant correlation was found between Δmorning BP surge and ΔLF-SBP (R = 0.150, P = 0.504, Fig. 3c). These relationships were nearly unchanged when including those who did not adhere to the intervention in the SJL trial (ΔcfPWV and Δmorning BP surge: R = 0.605, P < 0.001, n = 18; ΔcfPWV and ΔLF-SBP: R = 0.375, P = 0.046, n = 20; Δmorning BP surge and ΔLF-SBP: R = 0.219, P = 0.200, n = 18).
Association between changes in central arterial stiffness and morning blood pressure surge (a) and changes in sympathetic nerve activity and central arterial stiffness (b) or morning blood pressure surge (c) from Friday to Monday (CON trial: n = 14, SJL trial: n = 14). Δ means the change from Friday to Monday in each trial. Open circle (○): CON trial. Closed circle (●): SJL trial. The open and closed circles of each participants were connected with thin dot line. BP, blood pressure; cfPWV, carotid-femoral pulse wave velocity; CON, control trial; LF-SBP, low-frequency systolic blood pressure; SJL, social jetlag trial
Discussion
The significant finding of the present study was that acute SJL on weekends (181 ± 24 min) increased cfPWV and morning BP surge on Monday (Figs. 1, 2a, b). Furthermore, a significant positive correlation was found between ΔcfPWV and Δmorning BP surge (Fig. 3a). These results were obtained without the changes in other lifestyle variables such as sleep duration, energy expenditure, and intake. Therefore, the present study suggests that acute SJL on weekends augments morning BP surge with central arterial stiffening on Monday.
Alteration of morning BP surge by acute social jetlag
SJL trial significantly augmented morning BP surge (Fig. 2b), and the change was correlated with ΔcfPWV (Fig. 3a). Previous studies demonstrated that morning BP surge was significantly correlated with cfPWV [23, 33, 34]. Central arteries expand and recoil effectively within each cardiac cycle, providing a Windkessel effect to dampen left ventricular ejection pressure. Increased central arterial stiffness leads to less Windkessel function and augments BP [35]. Thus, the augmentation of morning BP surge in the SJL trial (Fig. 3b) might be attributed to the loss of Windkessel function caused by increased central arterial stiffness (Fig. 3a).
As baroreceptors, located in the carotid artery and aortic arch, are stretch receptors, the deformation of the barosensory arterial wall is required to initiate neural firing [36]. Knutsen et al. [37]. have suggested that the arterial diameter experiences less distension in a stiffer artery. Morning BP surge was negatively correlated with cvBRS, which modulates cardiac BP via the autonomic nervous system [38]. Moreover, it was found that a decreased cvBRS was caused by an augmentation in central arterial stiffness in the morning [39]. In the present study, the cvBRS was not significantly different between pre- and post-interventions in the SJL trial (Table 3), suggesting no influence of cvBRS on the augmentation of morning BP surge by acute SJL. Okada et al. [23]. have reported that the sympathetic baroreflex, which regulates BP via vasoconstriction, has greater contribution to the morning BP control than cvBRS. Thus, sympathetic BRS may play a more important role in the regulation of morning BP. However, we did not assess the sympathetic BRS in the present study.
Response of central arterial stiffness to acute SJL
The cfPWV was significantly elevated during the SJL trial compared with pre-intervention (Fig. 2a). Central arterial stiffness is mainly determined by central arterial structure (e.g., elastin, collagen, and smooth muscle) and function (e.g., vasoactive substance and sympathetic nerve activity). LF-SBP, an accepted marker of sympathetic vasomotor control, was increased in the SJL trial (Table 3), and the change was positively associated with the alteration of central arterial stiffening after acute SJL (Fig. 3b). A previous study has reported that elevation of sympathetic nerve activity in vessels (measured muscle sympathetic nerve activity) increases central arterial stiffness [40]. Acute stimulation, such as exercise, drastically increases sympathetic nerve activity [41, 42]. Since acute SJL is unlikely to induce structural remodeling as suggested in several studies that investigated the effects of acute stimulation on arterial structure [43, 44], the functional component would be attributed to the temporal central arterial stiffening.
The mechanisms underlying acute SJL elevation of sympathetic nerve activity remain unclear. We can speculate that the phenomenon is attributed to circadian disruption caused by acute SJL. An animal study has shown that simulated 12-h jet lag caused by air travel led to a pressor response by increasing the activity of the sympathetic nervous system via oxidative stress in the rostral ventrolateral medulla, which plays a role in cardiovascular regulatory nuclei within the brainstem [8]. However, we did not measure any index to clarify these mechanisms underlying the elevation of sympathetic nerve activity caused by acute SJL. Although alteration of the LF-SBP has been considered a marker of changes in sympathetic efferent activity to the peripheral vasculature, it is not a directly measured sympathetic nervous activity, such as muscle sympathetic nerve activity.
Response of central arterial stiffness and morning BP surge to acute SJL when including those who did not adhere to the intervention in the SJL trial
Although there were significant interactions in cfPWV, morning BP surge, and time course of ambulatory SBP, the significant interactions disappeared when including participants who did not adhere to the intervention in the SJL trial (SJL < 2 h). The results suggest that acute small SJL ( < 2 h) does not influence cardiovascular system in healthy men. As the present study could not clarify how many hours of SJL influence the cardiovascular system, further study is necessary.
Study limitations
This study has some limitations. First, although we randomly assigned participants to two trials, the intervention was not performed in a blinded manner, which might have caused bias in the results. Second, we did not evaluate whether acute SJL altered circadian variables, such as clock gene expression levels and circadian-regulated hormones. Therefore, the present study could not clarify whether the intervention caused circadian disruption. Third, self-reported energy intake might be underestimated because the energy intake was low relative to energy expenditure throughout the intervention. Fourth, because only healthy male participants were recruited for the present study, the generalizability of our findings to other populations is limited. Future studies should be performed to solve these limitations.
Perspectives
Our findings may contribute to clarifying pathophysiological mechanisms to prevent the Monday morning-specific increase in cardiovascular events. It has been reported that cardiovascular events and strokes often occur on Mondays [45,46,47]. Furthermore, these cardiovascular events are experienced mainly in the morning [48]. Although Kimura et al. [49]. have reported that increased double product affects the Monday morning-specific increase in cardiovascular events, the mechanisms remain unclear. Considering many people work on weekdays (Monday to Friday) and take a day off on weekends (Saturday and Sunday) in modern society, our findings provide new mechanistic insight that SJL is highly likely to contribute to the Monday morning-specific increase in cardiovascular events. To our knowledge, this is the first study examining the effect of acute SJL on the cardiovascular system. Future work should be performed to understand both the acute and chronic effects of SJL on the cardiovascular system and their underlying mechanisms based on the protocol of the present study.
In conclusion, acute SJL augments morning BP surge in the present study. Although this phenomenon may correspond to increase central arterial stiffness, we cannot yet identify the mechanisms that explain the central arterial stiffening with acute SJL. The underlying physiological mechanisms and clinical implications of these findings warrant further study. However, we assert this is the first study revealing the effects of acute SJL on the cardiovascular system.
References
Wittmann M, Dinich J, Merrow M, Roenneberg T. Social jetlag: Misalignment of biological and social time. Chronobiol Int. 2006;23:497–509. https://doi.org/10.1080/07420520500545979.
Roenneberg T, Allebrandt KV, Merrow M, Vetter C. Social jetlag and obesity. Curr Biol. 2012;22:939–43. https://doi.org/10.1016/j.cub.2012.03.038.
Roenneberg T, Kantermann T, Juda M, Vetter C, Allebrandt KV. Light and the human circadian clock. Handb Exp Pharmacol. 2013;217:311–31. https://doi.org/10.1007/978-3-642-25950-0_13.
Parsons MJ, Moffitt TE, Gregory AM, Goldman-Mellor S, Nolan PM, Poulton R, et al. Social jetlag, obesity and metabolic disorder: investigation in a cohort study. Int J Obes. 2015;39:842–8. https://doi.org/10.1038/ijo.2014.201.
Komada Y, Okajima I, Kitamura S, Inoue Y. A survey on social jetlag in Japan: a nationwide, cross-sectional internet survey. Sleep Biol Rhythms. 2019;17:417–22. https://doi.org/10.1007/s41105-019-00229-w.
Wong PM, Hasler BP, Kamarck TW, Muldoon MF, Manuck SB. Social jetlag, chronotype, and cardiometabolic risk. J Clin Endocrinol Metab. 2015;100:4612–20. https://doi.org/10.1210/jc.2015-2923.
Islam Z, Akter S, Kochi T, Hu H, Eguchi M, Yamaguchi M, et al. Association of social jetlag with metabolic syndrome among Japanese working population: the Furukawa Nutrition and Health Study. Sleep Med. 2018;51:53–8. https://doi.org/10.1016/j.sleep.2018.07.003.
Kishi T, Sunagawa K Experimental ‘jet lag’ causes sympathoexcitation via oxidative stress through AT1 receptor in the brainstem. Annu Int Conf IEEE Eng Med Biol Soc. 2011; 1969–72. https://doi.org/10.1109/IEMBS.2011.6090555.
Muller JE, Tofler GH, Stone PH. Circadian variation and triggers of onset of acute cardiovascular disease. Circulation. 1989;79:733–43. https://doi.org/10.1161/01.CIR.79.4.733.
Tochikubo O, Kawano Y, Miyajima E, Toshihiro N, Ishii M. Circadian variation of hemodynamics and baroreflex functions in patients with essential hypertension. Hypertens Res. 1997;20:157–66. https://doi.org/10.1291/hypres.20.157.
Kario K, Pickering TG, Umeda Y, Hoshide S, Hoshide Y, Morinari M, et al. Morning surge in blood pressure as a predictor of silent and clinical cerebrovascular disease in elderly hypertensives: a prospective study. Circulation. 2003;107:1401–6. https://doi.org/10.1161/01.CIR.0000056521.67546.AA.
Li Y, Thijs L, Hansen TW, Kikuya M, Boggia J, Richart T, et al. Prognostic value of the morning blood pressure surge in 5645 subjects from 8 populations. Hypertension. 2010;55:1040–8. https://doi.org/10.1161/HYPERTENSIONAHA.109.137273.
Murakami S, Otsuka K, Kubo Y, Shinagawa M, Yamanaka T, Ohkawa SI, et al. Repeated ambulatory monitoring reveals a Monday morning surge in blood pressure in a community-dwelling population. Am J Hypertens. 2004;17:1179–83. https://doi.org/10.1016/j.amjhyper.2004.07.016.
Benedetti D, Olcese U, Frumento P, Bazzani A, Bruno S, d’Ascanio P, et al. Heart rate detection by Fitbit ChargeHRTM: a validation study versus portable polysomnography. J Sleep Res. 2021;30:1–10. https://doi.org/10.1111/jsr.13346.
Dong X, Yang S, Guo Y, Lv P, Wang M, Li Y. Validation of Fitbit Charge 4 for assessing sleep in Chinese patients with chronic insomnia: a comparison against polysomnography and actigraphy. PLoS One. 2022;17:1–14. https://doi.org/10.1371/journal.pone.0275287.
Fürstenberg A, Davenport A. Comparison of multifrequency bioelectrical impedance analysis and dual-energy X-ray absorptiometry assessments in outpatient hemodialysis patients. Am J Kidney Dis. 2011;57:123–9. https://doi.org/10.1053/j.ajkd.2010.05.022.
Esco MR, Snarr RL, Leatherwood MD, Chamberlain NA, Redding ML, Flatt AA, et al. Comparison of total and segmental body composition using DXA and multifrequency bioimpedance in collegiate female athletes. J Strength Cond Res. 2015;29:918–25. https://doi.org/10.1519/JSC.0000000000000732.
Kim M, Shinkai S, Murayama H, Mori S. Comparison of segmental multifrequency bioelectrical impedance analysis with dual-energy X-ray absorptiometry for the assessment of body composition in a community-dwelling older population. Geriatr Gerontol Int. 2015;15:1013–22. https://doi.org/10.1111/ggi.12384.
Safar ME, London GM. Therapeutic studies and arterial stiffness in hypertension: recommendations of the European Society of Hypertension. The Clinical Committee of Arterial Structure and Function. Working Group on Vascular Structure and Function of the European Society of Hyp. J Hypertens. 2000;18:1527–35. https://doi.org/10.1097/00004872-200018110-00001.
Vlachopoulos C, Aznaouridis K, Stefanadis C. Prediction of cardiovascular events and all-cause mortality with arterial stiffness. A systematic review and meta-analysis. J Am Coll Cardiol. 2010;55:1318–27. https://doi.org/10.1016/j.jacc.2009.10.061.
Gando Y, Yamamoto K, Murakami H, Ohmori Y, Kawakami R, Sanada K, et al. Longer time spent in light physical activity is associated with reduced arterial stiffness in older adults. Hypertension. 2010;56:540–6. https://doi.org/10.1161/HYPERTENSIONAHA.110.156331.
Kario K, Hoshida S, Saito K, Sato K, Hamasaki H, Suwa H, et al. Validation of the TM-2441 ambulatory blood pressure measurement device according to the ISO 81060-2: 2013 standard. Blood Press Monit. 2019;24:38–41. https://doi.org/10.1097/MBP.0000000000000357.
Okada Y, Melyn Galbreath M, Shibata S, Jarvis SS, Bivens TB, Vongpatanasin W, et al. Morning blood pressure surge is associated with arterial stiffness and sympathetic baroreflex sensitivity in hypertensive seniors. Am J Physiol - Hear Circ Physiol. 2013;305:793–802. https://doi.org/10.1152/ajpheart.00254.2013.
Yang H, Carter JR. Baroreflex sensitivity analysis: spontaneous methodology vs. Valsalva’s maneuver. Clin Auton Res. 2013;23:133–9. https://doi.org/10.1007/s10286-013-0195-9.
Heart rate variability: standards of measurement, physiological interpretation and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Circulation. 1996;93:1043–65.
Bilchick KC, Berger RD. Heart rate variability. J Cardiovasc Electrophysiol. 2006;17:691–4. https://doi.org/10.1111/j.1540-8167.2006.00501.x.
Pagani M, Malliani A. Interpreting oscillations of muscle sympathetic nerve activity and heart rate variability. J Hypertens. 2000;18:1709–19. https://doi.org/10.1097/00004872-200018120-00002.
Pagani M, Montano N, Porta A, Malliani A, Abboud FM, Birkett C, et al. Relationship between spectral components of cardiovascular variabilities and direct measures of muscle sympathetic nerve activity in humans. Circulation. 1997;95:1441–8. https://doi.org/10.1161/01.CIR.95.6.1441.
Bos WJW, Van Goudoever J, Van Montfrans GA, Van den Meiracker AH, Wesseling KH. Reconstruction of brachial artery pressure from noninvasive finger pressure measurements. Circulation. 1996;94:1870–5. https://doi.org/10.1161/01.CIR.94.8.1870.
Wesseling KH, Jansen JRC, Settels JJ, Schreuder JJ. Computation of aortic flow from pressure in humans using a nonlinear, three-element model. J Appl Physiol. 1993;74:2566–73. https://doi.org/10.1152/jappl.1993.74.5.2566.
Armentano R, Megnien JL, Simon A, Bellenfant F, Barra J, Levenson J. Effects of hypertension on viscoelasticity of carotid and femoral arteries in humans. Hypertension. 1995;26:48–54. https://doi.org/10.1161/01.hyp.26.1.48.
Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175–91. https://doi.org/10.3758/BF03193146.
Polónia J, Amado P, Barbosa L, Nazaré J, Silva JA, Bertoquini S, et al. Morning rise, morning surge and daytime variability of blood pressure and cardiovascular target organ damage. A cross-sectional study in 743 subjects. Rev Port Cardiol. 2005;24:65–78.
Artal-Sanz M, Tavernarakis N. Prohibitin couples diapause signalling to mitochondrial metabolism during ageing in C. elegans. Nature. 2009;461:793–7. https://doi.org/10.1038/nature08466.
Boutouyrie P, Chowienczyk P, Humphrey JD, Mitchell GF. Arterial Stiffness and Cardiovascular Risk in Hypertension. Circ Res. 2021;128:864–86. https://doi.org/10.1161/CIRCRESAHA.121.318061.
Aars H. Relationship between aortic diameter and aortic baroreceptor activity in normal and hypertensive rabbits. Acta Physiol Scand. 1969;75:406–14. https://doi.org/10.1111/j.1748-1716.1969.tb04394.x.
Knutsen RH, Beeman SC, Broekelmann TJ, Liu D, Tsang KM, Kovacs A, et al. Minoxidil improves vascular compliance, restores cerebral blood flow, and alters extracellular matrix gene expression in a model of chronic vascular stiffness. Am J Physiol - Hear Circ Physiol. 2018;315:H18–32. https://doi.org/10.1152/ajpheart.00683.2017.
Eguchi K, Tomizawa H, Ishikawa J, Hoshide S, Pickering TG, Shimada K, et al. Factors associated with baroreflex sensitivity: association with morning blood pressure. Hypertens Res. 2007;30:723–8. https://doi.org/10.1291/hypres.30.723.
Taylor CE, Atkinson G, Willie CK, Jones H, Ainslie PN, Tzeng YC. Diurnal variation in the mechanical and neural components of the baroreflex. Hypertension. 2011;58:51–6. https://doi.org/10.1161/HYPERTENSIONAHA.111.171512.
Holwerda SW, Luehrs RE, Dubose L, Collins MT, Wooldridge NA, Stroud AK, et al. Elevated muscle sympathetic nerve activity contributes to central artery stiffness in young and middle-age/older adults. Hypertension. 2019;73:1025–35. https://doi.org/10.1161/HYPERTENSIONAHA.118.12462.
Ichinose M, Saito M, Fujii N, Ogawa T, Hayashi K, Kondo N, et al. Modulation of the control of muscle sympathetic nerve activity during incremental leg cycling. J Physiol. 2008;586:2753–66. https://doi.org/10.1113/jphysiol.2007.150060.
Saito M, Tsukanaka A, Yanagihara D, Mano T. Muscle sympathetic nerve responses to graded leg cycling. J Appl Physiol. 1993;75:663–7. https://doi.org/10.1152/jappl.1993.75.2.663.
Lefferts WK, Augustine JA, Heffernan KS. Effect of acute resistance exercise on carotid artery stiffness and cerebral blood flow pulsatility. Front Physiol. 2014;5:101 https://doi.org/10.3389/fphys.2014.00101.
Chuensiri N, Tanaka H, Suksom D. The acute effects of supramaximal high-intensity intermittent exercise on vascular function in lean vs. obese prepubescent boys. Pediatr Exerc Sci. 2015;27:503–9. https://doi.org/10.1123/pes.2015-0100.
Witte DR, Grobbee DE, Bots ML, Hoes AW. A meta-analysis of excess cardiac mortality an monday. Eur J Epidemiol. 2005;20:401–6. https://doi.org/10.1007/s10654-004-8783-6.
Capodaglio G, Gallerani M, Fedeli U, Manfredini R. Contemporary burden of excess cardiovascular mortality on Monday. A retrospective study in the Veneto region of Italy. Int J Cardiol. 2016;214:307–9. https://doi.org/10.1016/j.ijcard.2016.03.234.
Shigematsu K, Watanabe Y, Nakano H. Weekly variations of stroke occurrence: an observational cohort study based on the Kyoto Stroke Registry, Japan. BMJ Open. 2015;5:1–6. https://doi.org/10.1136/bmjopen-2014-006294.
Gnecchi-ruscone T, Piccaluga E, Guzzetti S, Contini M, Montano N, Nicolis E. Morning and monday: critical periods for the onset of acute myocardial infaction: the GISSI 2 study experience. Eur Heart J. 1994;15:882–7. https://doi.org/10.1093/oxfordjournals.eurheartj.a060605.
Kimura G, Inoue N, Mizuno H, Izumi M, Nagatoya K, Ohtahara A, et al. Increased double product on Monday morning during work. Hypertens Res. 2017;40:671–4. https://doi.org/10.1038/hr.2017.16.
Acknowledgements
We appreciate the support received from all the participants in this study. Moreover, we would like to thank Editage (www.editage.com) for English language editing.
Funding
This work was supported by the JSPS KAKENHI to M Higuchi (Grant-in-Aid for Scientific Research [B], Grant Number: 18H03198).
Author information
Authors and Affiliations
Contributions
T.K., H.M. and N.N. conceived and designed the study. All authors conducted the experiments. N.N. and T.K. analyzed the data. All authors interpreted the data. N.N. and T.K. wrote the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nakamura, N., Akiyama, H., Nishimura, M. et al. Acute social jetlag augments morning blood pressure surge: a randomized crossover trial. Hypertens Res 46, 2179–2191 (2023). https://doi.org/10.1038/s41440-023-01360-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-023-01360-5
Keywords
This article is cited by
-
Social jet lag and morning blood pressure surge—central nervous system matters?
Hypertension Research (2023)