Abstract
To measure blood pressure precisely and make the data comparable among facilities, measurement methods and devices must be standardized. Since the Minamata Convention on Mercury, there is no metrological standard for sphygmomanometers. The current validation methods recommended by non-profit organizations in Japan, the US, and European Union countries are not necessarily applicable to the clinical setting, and no protocol for daily or routine performance of quality control has been defined. In addition, recent rapid technological advances have enabled monitoring blood pressure at home with wearable devices or without a cuff by using a smartphone app. A clinically relevant validation method for this recent technology is not available. The importance of out-of-office blood pressure measurement is highlighted by guidelines for the diagnosis and treatment of hypertension, but an appropriate protocol for validating a device is required.

Similar content being viewed by others
Introduction
The aim of managing hypertension is to reduce cardiovascular and renal complications and to obtain longevity of health. To achieve this aim, blood pressure is the most studied and commonly used biomarker of hypertension. The history of non-invasive blood pressure monitoring started in the early 20th century. Initial reports by Dr. Riva-Rocci [1] and Dr. Korotkoff [2] enabled the noninvasive measurement of blood pressure noninvasively with a cuff and auscultation. Since these reports were published, blood pressure has been measured in the office for a long time. In the 1980s, invasive and non-invasive ambulatory blood pressure monitoring was developed. Invasive blood pressure monitoring can collect all of the blood pressure data in 1 day that is ~0.1 million data/day [3]. However, this monitoring is invasive and not easy to perform repeatedly. Therefore, invasive blood pressure monitoring is limited to research purposes and not routinely used in the clinical setting. In contrast, non-invasive ambulatory blood pressure monitoring (ABPM) can be performed relatively easily. Clinical studies of ABPM have provided a lot of information, such as the importance of nighttime blood pressure, the morning surge, viability of blood pressure, white-coat hypertension, and others [4]. Currently, using not only office blood pressure but also out-of-office blood pressure monitoring to diagnose hypertension is recommended to evaluate the risk of cardiovascular complications and monitor the therapeutic effect of hypertensives. ABPM and home-measured blood pressure are the two main out-of-office blood pressure values currently used.
Two blood pressure measurement methods are used for ABPM and home blood pressure monitoring devices. These methods are the classical Korotkoff method and the oscillometric method. The Korotkoff method has several limitations, such as pseudo-hypertension in patients with atherosclerosis and interference by environmental noise, which interferes with the Korotkoff sound recording and makes the results unreliable. The oscillometric method can overcome the problem with noise and is widely used for ABPM and for home blood pressure monitoring systems. In addition, after the Minamata Convention on Mercury, mercury was banned for use in the medical field, and oscillometric methods are widely used in the clinical setting in Japan. The disadvantages of the oscillometric method are that it determines systolic and diastolic pressure by an algorithm that is different among devices, and manufacturers do not disclose the algorithm.
Biomarker measurements include several factors that induce false positive and false negative results. These factors are classified as preanalytical, analytical, and postanalytical factors. Preanalytical factors can be standardized by educating patients to control dietary intake, lifestyles such as smoking, exercise, and others. To monitor blood pressure, a guideline for standardizing the patients’ status has been published [5, 6]. The analytical error partly depends on care providers’ methods of using the apparatus. Proper use of a cuff and proper positioning of the arm are among factors responsible for an error. These factors are also standardized [5, 6]. Other causes for analytical errors are due to the apparatus, such as the failure of sensors, air inflation/deflation control, and others. Post-analytical errors are mistakes, which include recording on charts and miscalculations of mean BP measurements.
This review focuses on standardization and validation, and current issues of device-dependent analytical errors in the measurement of blood pressure and the future scope.
Standardization
To provide better health care to as many people as possible, healthcare services involve large healthcare facilities to small private clinics. With regard to blood pressure, home blood pressure monitoring is the utmost point of care testing (POCT). Among POCT, semi-quantitative immunochromatography has been used for a long time to diagnose pregnancy and influenza, and for screening colon cancer by fecal occult blood. After the coronavirus disease 2019 pandemic, immunochromatography was used for an antigen test. In addition, some blood chemical analyses, such as blood sugar and cholesterol concentrations, can be measured as POCT, and the results are electrically transferred to healthcare facilities. However, this testing mostly requires commodities, functioning equipment, trained personnel, and infrastructure. Simplification, efficiency, high quality, and affordability of testing are issues for service providers and patients. To achieve these goals, the standardization of methods is critical for strengthening clinical testing under limited resource settings.
The first step in standardization is to select the appropriate method and equipment for measurements. An example of this step is that, to measure aldosterone for screening of primary aldosteronism, we should choose liquid chromatography-mass spectrometry or the chemiluminescent enzyme immunoassay method, and then which machine and kits should be used for measurement should be decided. Each healthcare provider may choose different methods and different equipment. Intra-facility standardization can be achieved by using the equipment appropriately including its maintenance [7]. The most frequently used method of standardization is to measure low and high concentrations of a known standard material, such as pure aldosterone. These reference values are measured periodically, and the mean and standard deviation are calculated. A set of X-bar-R and R charts are constructed for relatively small data sets, and a set of X-bar-S and S charts are constructed for larger data sets (Fig. 1). X-bar-R and R charts are created from the absolute number of data, and X-bar-S and S charts are created from the standard deviation of measured data [7]. The Japanese Industrial Standards (JIS) define eight abnormal patterns of these charts. However, in the real world, too many abnormal criteria may lead to a type I error and this is not clinically applicable. In most laboratories, the shift and trend of these parameters are routinely checked and used to evaluate the validity of tests. A quality assurance (QA) program must include daily quality control (QC) evaluation, documentation, on-site assessments, inventory management, external quality assessment (EQA), staff education, and equipment maintenance. However, when comparing data in an inter-facility fashion, each facility may use different methods and different equipment. Therefore, inter-method standardization and inter-equipment standardization are mandatory.
X-bar and range (X-bar-R) chart of aldosterone by the chemiluminescent enzyme immunoassay (CLEIA) method in International University of Health and Welfare (IUHW) Narita Hospital in 2022. This chart is composed of two charts used in tandem. The chart’s x-axes are time-based so that the chart shows a history of the process, day-by-day, and time-to-time deviations. The X-bar chart is used to evaluate the consistency of process averages by plotting the average of the values when a known concentration of aldosterone is measured. The R chart plots the ranges of each measurement. The R chart is used to evaluate the consistency of process variation. The R chart should be viewed first. If the R chart is outside of control limits, then the control limits on the X-bar chart are meaningless. A low concentration of aldosterone, B high concentration of aldosterone
With regard to external quality control, it is performed by non-profit organizations, such as the Japan Medical Association, the Japanese Association of Medical Technologists, and the College of American Pathologists or Centers for Mediate and Medicaid Services in the US. These organizations send samples or photographs of pathology samples, electrocardiographic results, and other laboratory test data in a blinded fashion to each laboratory. Each laboratory independently analyzes them and returns answers to validate their accuracy.
To perform these steps, not only physicians but also medical technologists, nurses, and other medical staff, are necessary. Among these requirements, EQA may be difficult to perform for sphygmomanometers, but QC, staff education, and equipment maintenance can be carried out.
Standardization of office blood pressure measurement, current status, and future issues
The Japanese Society of Hypertension [8] recommends using the auscultation method with an electric sphygmomanometer or aneroid sphygmomanometer for blood pressure measurement, and they should be inspected. In 1993, a British guideline [9] recommended calibration before use by a Y-connected tube and in connection with a mercury sphygmomanometer. Eguchi et al. proposed a simple method to validate an automatic oscillometric sphygmomanometer [10]. After the abolition of mercury, these methods cannot be used anymore. A digital pressure gauge specialized for a sphygmomanometer is a candidate method for calibration, but this gauge is expensive and not easy to use. Most of the healthcare providers might not be able to routinely perform calibration or validation. The ISO81060-2:2018 guideline (https://www.iso.org/standard/73339.html; accessed 14 Jan 2023) recommends sequential blood pressure measurement in humans by one reference and one under a tested device. This process requires 85 people, and at least 3 valid paired blood pressure values should be obtained, with a maximum of 255 values. In addition to the number of samples, this guideline requires a particular sex distribution (>70% of the subjects should not be one sex) and an age distribution that is older than 12 years. Additionally, in children, another set of validation by 35 children is required. This ISO recommendation is for the manufacturers and not for health care providers. Therefore, healthcare providers rely on the report from the manufacturers. In Japan, the JIS and the ISO regulate the accuracy of sphygmomanometers, but they do not request QA follow up. In contrast, QA control has been discussed for long time in using ultrasound and electrocardiography, and many guidelines have been published [11, 12] on QA of these devices. QA is required for the ISO 15189 standard, and most clinical laboratories worldwide are accredited for this standard (in Japan, ~300 physiology laboratories are accredited as of January 2023).
The current issues of validating devices that should be solved are as follows: 1) establishment of validation and a QA method applicable to health care providers; and 2) establishment of a reference method of pressure monitoring after the discontinuation of mercury manometers. With regard to the sphygmomanometer, a guideline on how to validate its accuracy in the clinical setting should be proposed by ISO 15189 or other non-profit organizations. The current requirement for validation is to perform a quality check when the manufacturer delivers the device, which is too difficult for daily use and impossible to perform. With regard to the second issue, if there was a common and easily accessible reference for a manometer, validation would be much easier. A mercury sphygmomanometer was originally used for standardization, but as mentioned above, it currently cannot be used.
Oscillometric method for in-home and office blood pressure monitoring
The oscillometric method was originally developed for home blood pressure monitoring, but its reliability was questioned in the clinical setting [11]. Tolonen et al. [12] claimed that there is difficulty in comparing devices because the algorithms used for determining systolic and diastolic blood pressure are different in each device and not openly accessible. This problem causes difficulty in replicating validation studies for older models. However, the reliability of this method has been improved, and many validated devices are currently available in the healthcare setting [13] (lists of validated devices are found at: https://www.validatebp.org/, https://medaval.ie/; accessed in January 2023). The Kidney Disease: Improving Global Outcomes guideline for blood pressure management in chronic kidney disease [14] clearly states that the oscillometric method is superior to the auscultatory method, and the oscillometric method should be used. This guideline states that the automated oscillometric method does not have the above-mentioned observers’ bias. Negative aspects of oscillometric blood pressure devices are a potentially higher cost of the device compared with that for a manual device and the requirement of an electric power source. Therefore, oscillometric devices are not able to be used in economically restricted countries. Recent clinical trials used automated office blood pressure (AOBP) because it is more closely correlated with 24-h ambulatory blood pressure than regular blood pressure measurement at the clinic. Additionally, the device used in AOBP mostly uses the oscillometric method. Canadian guidelines [15] recommend using AOBP. These guidelines also state that the total time required to measure blood pressure by AOBP is 4–6 min and shorter than that in the conventional auscultatory method. The conventional method takes ~7–8 min, including a 5-min rest period, before starting the measurement. They also recommend unattended AOBP to avoid the white-coat phenomena, and this method can reduce the work burden of health care providers. However, the AOBP device might increase the deviation of data owing to aging of the sensor, air tube, or other parts. Validation of the device should be performed not only when it arrives from the manufacturer but also while using the device. Physicians should ask the patients to bring their devices to the clinic routinely to perform validation. However, fulfilling the requirements by the ISO, the JIS, and other organizations requires a certain number of blood pressure data from a wide variety of patients. A new appropriate protocol for validating a home blood pressure monitoring device is urgently required. In addition, there remain controversial discussion if AOBP stands for home blood pressure and clinic effect on blood pressure would not be negligible. And in Japan, it is often difficult to spare a room for AOBP in the clinic and we doubt AOBP is feasible in Japan [16].
Ambulatory blood pressure monitoring device
The importance of out-of-office blood pressure is stressed in most of the guidelines. A Japanese guideline [5] defines hypertension by ambulatory blood pressure monitoring (ABPM) showing ≥130/80 mmHg in 24 h, and ≥135/85 and ≥120/70 in the daytime and nighttime, respectively. This guideline also compared office and home blood pressure, and classified blood pressure levels in adults (Table 1). Validation of these automatic and unattended measurable devices is legitimate. As discussed above, current validation methods are complicated and require professional knowledge and a special environment to perform them. ABPM is carried out by health care providers, its validation can be obtained using a sphygmomanometer, and staff education is easily performed. However, there is a concern that a certain percentage of patients have paroxysmal atrial fibrillation or extrasystole during the 24 h of monitoring. The reliability of blood pressure values by an automatic device in the presence of arrhythmia is an important issue. In contrast to a home blood pressure monitoring device, ABPM records reliable blood pressure in patients with sustained atrial fibrillation. Recently, Watanabe et al. reported a novel algorithm to detect paroxysmal atrial fibrillation by an ABPM device [17].
Next generation of blood pressure monitoring devices and their validation
Novel wearable devices that can monitor physiological parameters, such as body temperature, heart rate, respiratory rate, blood glucose concentrations, and extrasystole, have been developed and are widely used. Additionally, blood pressure monitoring devices are still under development. The advantages of wearable devices over ABPM or home blood pressure monitoring devices are that they are more comfortable and can repeatedly collect data with less energy. There is one Japanese government-approved device available and some in the US and other countries. The blood pressure monitoring mechanisms are different between devices. The oscillometric method at the wrist or at the fingers, photoplethysmography, and tonometry is used. The Omron HEM-6410 T [18] (HeartGuide, Omron Healthcare Co., Ltd.) is approved in Japan and the US, but its use is limited under the sitting position, and blood pressure is monitored on demand. Night-time blood pressure or blood pressure during exercise or walking cannot be measured. The finger-type device is uncomfortable for daily use because it is too large; therefore, further technological advances are required. In contrast to the HEM-6410, the tonometry method, which is also not applicable during exercise or the standing position, is suitable for measuring nighttime blood pressure [19]. The third method of photoplethysmography (PPG) is a non-invasive technique through which changes in blood flow are detected during the cardiac cycle [20]. Therefore, PPG requires monitoring of an electrocardiogram, and the R-R time must be measured. The device using this method has not been approved in any countries yet because the stability of the PPG signal is affected by movements, which restricts its use to only the non-ambulatory setting. Another limitation is the need for frequent calibration of the device. A recently integrated method of oscillometry and PPG has been developed using a smartphone [21], and it is a non-physical method of measuring blood pressure by monitoring the color of the face [22].
Although there are great advantages in these wearable devices, the development of appropriate calibration and validation methods is an issue. Most of the clinical data are accumulated with upper-arm blood pressure data and not by wrist blood pressure. The calibration of absolute blood pressure values is required. The device used for measuring blood pressure should be validated in the long term and repetitively. The current regulations by the JIS or the Association for the Advancement of Medical Instrumentation/European Society of Hypertension/International Organization for Standardization (AAMI/ESH/ISO) protocol require validation at the time point of when the device is purchased and are not satisfactory to validate unattended measurement of BP by professionals and for repeated measurements. A proper alarm system when blood pressure is measured inappropriately needs to be developed and validated. As mentioned above, the timing of repeated calibration and validation must be set, and the error ranges must be set in a satisfactory narrow range. Technology advances much faster than expected. Therefore, validation methods should keep up to date with the technology. Cuff-less techniques, such as PPG by face color, cannot be calibrated by the current methods suggested by the authorities. The scientific community and industrial companies should collaborate and develop a reliable protocol for validation and QA that are applicable to the real world.
Conclusion
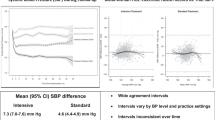
Without mercury, there is no gold standard of calibration for any blood pressure measurement device. Currently, simultaneous blood pressure measurement by auscultation and comparison with other devices is used for calibration, and an error (mean ± standard deviation) of 5 ± 8 mmHg is acceptable. An increasing number of precise measurements are possible in a variety of medical fields, and blood pressure monitoring is also expected to be more precise and reflect a variety of physiological changes. Out-of-office blood pressure monitoring (i.e., unattended blood pressure measurements) may meet some expectations, and technology in this field is rapidly advancing. Flexible, but reliable, protocols for QA of upcoming devices should be set promptly and updated without delay.
References
Riva-Rocci S. Un nuovo sfigmomanometro. Gazz Med di Torino. 1896;47:981–96.
Korotkoff NS. On methods of studying blood pressure [in Russian]. Bull Imperial Mil Med Acad. 1905;11:365–7.
Tochikubo O, Umemura S, Noda K, Kaneko Y. Variability of arterial blood pressure and classification of essential hypertension by multivariate statistical analysis. Jpn Circ J. 1981;45:781–99.
Kario K. Essential manual of 24-hour blood pressure management. 2nd ed., 2022 Wiley Blackwell ISBN-10: 1119799368 ISBN-13: 978-1119799368.
Padwal R, Campbell N, Schutte A, Olsen MH, Delles C, Etyang A, et al. Optimizing observer performance of clinic blood pressure measurement: a position statement from the Lancet Commission on Hypertension Group. J Hypertens. 2019;37:1737–45.
Cheung AK, Whelton PK, Muntner P, Schutte AE, Moran AE, Williams B, et al. International consensus on standardized clinic blood pressure measurement—a call to action. Am J Med. 2023;S0002-9343:00890–7.
Ladwig P, Rychert J. EP19 a framework for using CLSI documents to evaluate medical laboratory test methods, 3rd ed. The Clinical and Laboratory Standards Institute ISBN Number: 978-1-68440-165-9
Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens Res. 2019;42:1235–481.
O’Brien E, Petrie J, Littler WA, de Swiet M, Padfield PL, Altman D, et al. The British Hypertension Society Protocol for the evaluation of blood pressure measuring devices. J Hypertens. 1993;11:S43–S63.
Eguchi K, Kuruvilla S, Ishikawa J, Schwartz JE, Pickering TG. A novel and simple protocol for the validation of home blood pressure monitors in clinical practice. Blood Press Monit. 2012;17:210–3.
Ostchega Y, Zhang G, Sorlie P, Hughes JP, Reed-Gillette DS, Nwankwo T, et al. Blood pressure randomized methodology study comparing automatic oscillometric and mercury sphygmomanometer devices: National Health and Nutrition Examination Survey, 2009-2010. Natl Health Stat Rep. 2012;59:1–15.
Tolonen H, Koponen P, Naska A, Männistö S, Broda G, Palosaari T, et al. Challenges in standardization of blood pressure measurement at the population level. BMC Med Res Methodol. 2015;15:33.
Picone DS, Campbell NRC, Schutte AE, Olsen MH, Ordunez P, Whelton PK, et al. Validation status of blood pressure measuring devices sold globally. JAMA. 2022;327:680–1.
Kidney Disease: Improving Global Outcomes (KDIGO) Blood Pressure Work Group. KDIGO 2021 clinical practice guideline for the management of blood pressure in chronic kidney disease. Kidney Int. 2021;99:S1–S87.
Tobe SW, Stone JA, Anderson T, Bacon S, Cheng AYY, Daskalopoulou SS, et al. Canadian Cardiovascular Harmonized National Guidelines Endeavour (C-CHANGE) guideline for the prevention and management of cardiovascular disease in primary care: 2018 update. CMAJ. 2018;190:E1192–E1206.
Asayama K, Ohkubo T, Rakugi H, Miyakawa M, Mori H, Katsuya T, et al. Japanese Society of Hypertension Working Group on the COmparison of Self-measured home, automated unattended office and Conventional attended office blood pressure (COSAC) study. Comparison of blood pressure values-self-measured at home, measured at an unattended office, and measured at a conventional attended office. Hypertens Res. 2019;42:1726–37.
Watanabe T, Tomitani N, Yasui N, Kario K. Validation of an ambulatory blood pressure monitoring device employing a novel method to detect atrial fibrillation. Hypertens Res. 2022;45:1345–52.
Kuwabara M, Harada K, Hishiki Y, Kario K. Validation of two watch-type wearable blood pressure monitors according to the ANSI / AAMI / ISO81060-2: 2013 guidelines: Omron HEM-6410T-ZM and HEM-6410T-ZL. J Clin Hypertens. 2019;21:853–8.
Kokubo A, Kuwabara M, Nakajima H, Tomitani N, Yamashita S, Shiga T, et al. Automatic detection algorithm for establishing standard to identify “surge blood pressure”. Med Biol Eng Comput. 2020;58:1393–404.
Wang R, Jia W, Mao ZH, Sclabassi RJ, Sun M. Cuff-free blood pressure estimation using pulse transit time and heart rate. Int Conf Signal Process Proc. 2014;2014:115–8.
Chandrasekhar A, Kim CS, Naji M, Natarajan K, Hahn JO, Mukkamala R. Smartphone-based blood pressure monitoring via the oscillometric finger-pressing method. Sci Transl Med. 2018;10:eaap8674.
Luo H, Yang D, Barszczyk A, Vempala N, Wei J, Wu SJ, et al. Smartphone-based blood pressure measurement using transdermal optical imaging technology. Circ Cardiovasc Imaging. 2019;12:e008857.
Acknowledgements
We thank Ellen Knapp, PhD, from Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shimosawa, T. Quality is not an act, it is a habit—Aristotle. Hypertens Res 46, 1221–1226 (2023). https://doi.org/10.1038/s41440-023-01234-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-023-01234-w