Abstract
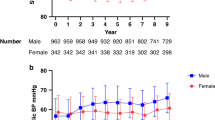
Ambulatory BP monitoring is increasingly used in children and adolescents, and the persistence of discrepant phenotypes, such as white coat or masked hypertension, is a relevant issue. The objective of this study was to assess the persistence of BP phenotypes over time and the factors related to their persistence. The study included 582 children and adolescents (9.4 ± 2.8 years of age) of both sexes (51% females) referred for routine health maintenance. Anthropometric parameters and office and 24-h ABPM measurements were obtained twice (interval 19.5 ± 6.9 months). BP classification and phenotypes were qualified using the 2016 ESH Guidelines. The correlation coefficient and kappa statistics were used to assess the persistence of phenotypes, and the related factors were evaluated using logistic regression. Based on both systolic and diastolic BP measurements, 91.6%, 16%, 17.2% and 13.7% of the subjects with true normotension, sustained HTN, white coat HTN and masked HTN, respectively, remained in the same category (overall agreement 74.2%, kappa 0.20). The multivariate model predicted the lack of persistence and correctly classified 90.3% of the subjects, with the pathological baseline BP phenotype (mainly masked HTN) being the independent variable that contributed most to the model. Excluding the phenotypes, the rest of the model explained 14% of the lack of persistence, and a high office SBP and high waist circumference were related to the lack of persistence. Furthermore, subjects who experienced an increase in their BMI z score and change in their BMI category were at risk of a lack of persistence. In conclusion, children, especially those with BP phenotypes different from true normotension, should be re-evaluated because a large percentage are likely to become normotensive.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Lurbe E, Agabiti-Rosei E, Cruickshank JK, Dominiczak A, Erdine S, Hirth A, et al. 2016 European Society of Hypertension guidelines for the management of high blood pressure in children and adolescents. J Hypertens. 2016;34:1887–920.
Falkner B, Lurbe E. Primary hypertension beginning in childhood and risk for future cardiovascular disease. J Pediatr. 2021;238:16–25.
Flynn JT, Daniels SR, Hayman LL, Maahs DM, McCrindle BW, Mitsnefes M, et al. Update: ambulatory blood pressure monitoring in children and adolescents: a scientific statement from the American Heart Association. Hypertension. 2014;63:1116–35.
Parati G, Stergiou GS, Dolan E, Bilo G. Blood pressure variability: clinical relevance and application. J Clin Hypertens. 2018;20:1133–7.
Sarganas G, Schaffrath Rosario A, Niessner C, Woll A, Neuhauser HK. Tracking of blood pressure in children and adolescents in germany in the context of risk factors for hypertension. Int J Hypertens. 2018;2018:1–10.
Daley MF, Sinaiko AR, Reifler LM, Tavel HM, Glanz JM, Margolis KL, et al. Patterns of care and persistence after incident elevated blood pressure. Pediatrics. 2013;132:e349–355.
Kaelber DC, Localio AR, Ross M, Leon JB, Pace WD, Wasserman RC, et al. Persistent hypertension in children and adolescents: a 6-year cohort study. Pediatrics. 2020;146:e20193778.
Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, Daniels SR, et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. 2017;140:e20171904.
Salice P, Ardissino G, Barbier P, Bacà L, Vecchi DL, Ghiglia S, et al. Differences between office and ambulatory blood pressures in children and adolescents attending a hospital hypertension clinic. J Hypertens. 2013;31:2165–75.
Davis ML, Ferguson MA, Zachariah JP. Clinical predictors and impact of ambulatory blood pressure monitoring in pediatric hypertension referrals. J Am Soc Hypertens. 2014;8:660–7.
Johnson PK, Ferguson MA, Zachariah JP. In-clinic blood pressure prediction of normal ambulatory blood pressure monitoring in pediatric hypertension referrals: clinic prediction of normal ABPM in youth. Congenit Heart Dis. 2016;11:309–14.
Hamdani G, Flynn JT, Becker RC, Daniels SR, Falkner B, Hanevold CD, et al. Prediction of ambulatory hypertension based on clinic blood pressure percentile in adolescents: the SHIP AHOY study. Hypertension. 2018;72:955–61.
Ishikawa J, Ishikawa Y, Edmondson D, Pickering TG, Schwartz JE. Age and the difference between awake ambulatory blood pressure and office blood pressure: a meta-analysis. Blood Press Monit. 2011;16:159–67.
Lurbe E, Torro I, Alvarez V, Nawrot T, Paya R, Redon J, et al. Prevalence, persistence, and clinical significance of masked hypertension in youth. Hypertension. 2005;45:493–8.
Lurbe E, Thijs L, Torro MI, Alvarez J, Staessen JA, Redon J. Sexual dimorphism in the transition from masked to sustained hypertension in healthy youths. Hypertension. 2013;62:410–4.
WHO Multicentre Growth Reference Study Group, Onis M. WHO Child Growth Standards based on length/height, weight and age: WHO child growth standards. Acta Paediatr. 2007;95:76–85.
de Onis M. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007;85:660–7.
Lurbe E, Redon J, Alvarez J, Grau-Pérez M, Martinez F, Mancia G. Insights from matched office and ambulatory blood pressure in youth: clinical relevance. Hypertension. 2022;79:1237–46.
Wühl E, Witte K, Soergel M, Mehls O, Schaefer F. Distribution of 24-h ambulatory blood pressure in children: normalized reference values and role of body dimensions. J Hypertens. 2002;20:1995–2007.
Stergiou GS, Palatini P, Parati G, O’Brien E, Januszewicz A, Lurbe E, et al. European Society of Hypertension Council and the European Society of Hypertension Working Group on Blood Pressure Monitoring and Cardiovascular Variability. 2021 European Society of Hypertension practice guidelines for office and out-of-office blood pressure measurement. J Hypertens. 2021;39:1293–302.
Cohen JB, Lotito MJ, Trivedi UK, Denker MG, Cohen DL, Townsend RR. Cardiovascular Events and Mortality in White Coat Hypertension: A Systematic Review and Meta-analysis. Ann Intern Med. 2019;170:853.
Huang Y, Huang W, Mai W, Cai X, An D, Liu Z, et al. White-coat hypertension is a risk factor for cardiovascular diseases and total mortality. J Hypertens. 2017;35:677–88.
Stabouli S, Kotsis V, Toumanidis S, Papamichael C, Constantopoulos A, Zakopoulos N. White-coat and masked hypertension in children: association with target-organ damage. Pediatr Nephrol. 2005;20:1151–5.
Lande MB, Meagher CC, Fisher SG, Belani P, Wang H, Rashid M. Left ventricular mass index in children with white coat hypertension. J Pediatr. 2008;153:50–54.
Westerståhl M, Forss M, Persson L, Bouma K, Gustavsson T, Wühl E, et al. Hypertension outcomes and cardiovascular status in young adults with childhood-diagnosed white coat hypertension. Arch Dis Child. 2018;103:113–4.
Rucki S, Feber J. Repeated ambulatory blood pressure monitoring in adolescents with mild hypertension. Pediatr Nephrol. 2001;16:911–5.
Miyashita Y, Hanevold C, Faino A, Scher J, Lande M, Yamaguchi I, et al. White coat hypertension persistence in children and adolescents: the Pediatric Nephrology Research Consortium Study. J Pediatr. 2022;S0022347622002864.
Hanevold CD, Miyashita Y, Faino AV, Flynn JT. Changes in ambulatory blood pressure phenotype over time in children and adolescents with elevated blood pressures. J Pediatr. 2020;216::37–43.e2.
Yang Q, Zhong Y, Merritt R, Cogswell ME. Trends in high blood pressure among united states adolescents across body weight category between 1988 and 2012. J Pediatr. 2016;169:166–173.e3.
So HK, Yip GWK, Choi KC, Li AM, Leung LCK, Wong SN, et al. Association between waist circumference and childhood-masked hypertension: a community-based study: WC and childhood-masked hypertension. J Paediatr Child Health. 2016;52:385–90.
Acknowledgements
We acknowledge the expert assistance of Christine Deutsch.
Funding
The study was partially funded by the Centro de Investigación Biomédica en Red Fisiopatología Obesidad y Nutrición (CB06/03), Ministerio de Ciencia, Innovación y Universidades (Grant Number PI20/00269), Instituto de Salud Carlos III and cofinanced by the European Regional Development Fund (to EL). This study was funded by the Instituto de Salud Carlos III (ISCIII) through the project INTEGRActiv, Project title “Identification and validation of integrative biomarkers of physical activity level and health in children and adolescents” and co-funded by Next Generation EU, Mecanismo para la Recuperación y la Resiliencia (MRR). This publication is based upon the work of the COST Action HyperChildNET (CA19115), with the support of COST (European Cooperation in Science and Technology). Fernando Martinez received the support of a Virtual Mobility from COST Action HyperChildNET (CA19115), Identification number E-COST-GRANT-CA19115-5923465e.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Martinez, F., Redon, J., Aguilar, F. et al. Persistence and determinants of blood pressure phenotypes according to office and ambulatory blood pressure measurements in youth. Hypertens Res 46, 1257–1266 (2023). https://doi.org/10.1038/s41440-022-01159-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-022-01159-w
Keywords
This article is cited by
-
Persistence of blood pressure phenotypes defined by office and ambulatory measurements in youth of 5 to 15 years of age
Hypertension Research (2023)
-
Masked Hypertension in Healthy Children and Adolescents: Who Should Be Screened?
Current Hypertension Reports (2023)