Abstract
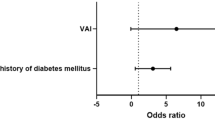
Concurrent autonomous cortisol secretion (ACS) in patients with primary aldosteronism (PA patients) is not uncommon. This work aimed to determine the effect of cortisol levels on incident new-onset type 2 diabetes mellitus (NODM) in PA patients. Using the prospectively designed observational TAIPAI cohort, the PA patients were grouped by cortisol level after an overnight low-dose dexamethasone suppression test (1-mg DST). Of the 476 PA patients, 387 (43.7% men; mean age 52.8 years) did not have baseline DM. After a mean follow-up of 4.3 ± 2.9 years, 32 patients (8.3%) developed NODM. The cutoff value obtained via a generalized additive model showed that a serum cortisol level ≥ 2.65 µg/dL after 1-mg DST was a risk factor for developing NODM (HR, 3.5, p = 0.031) by Cox proportional- hazards model.. In PA patients with a higher body mass index (>25 kg/m2; HR, 3.16), lower estimated glomerular filtration rate (<90 ml/min/1.73 m2; HR, 3.18), longer hypertension duration (>7 years; HR, 3.34), and higher waist-to-hip ratio (>0.9; HR, 3.07), a concomitant cortisol level ≥ 2.65 μg/dL after 1-mg DST were more likely to develop NODM. The high-cortisol group of patients with aldosterone-producing adenoma (APA) using mineralocorticoid receptor antagonist (MRA) was associated with an increased risk of NODM (HR, 5.72). Our results showed that PA patients with a concomitant cortisol level ≥ 2.65 µg/dL after 1-mg DST, independent of the aldosterone level, had a higher incidence of NODM. Such PA patients should be carefully evaluated and managed to achieve better glucose control and prevent metabolic syndrome.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Mulatero P, Stowasser M, Loh KC, Fardella CE, Gordon RD, Mosso L, et al. Increased diagnosis of primary aldosteronism, including surgically correctable forms, in centers from five continents. J Clin Endocrinol Metab. 2004;89:1045–50.
Rossi GP, Bernini G, Caliumi C, Desideri G, Fabris B, Ferri C, et al. A prospective study of the prevalence of primary aldosteronism in 1,125 hypertensive patients. J Am Coll Cardiol. 2006;48:2293–300.
Akehi Y, Yanase T, Motonaga R, Umakoshi H, Tsuiki M, Takeda Y, et al. High prevalence of diabetes in patients with primary aldosteronism (PA) associated with subclinical hypercortisolism and prediabetes more prevalent in bilateral than unilateral PA: a large, multicenter cohort study in Japan. Diabetes Care. 2019;42:938–45.
Wu VC, Chueh SJ, Chen L, Chang CH, Hu YH, Lin YH, et al. Risk of new-onset diabetes mellitus in primary aldosteronism: a population study over 5 years. J Hypertens. 2017;35:1698–708.
Yanase T, Oki Y, Katabami T, Otsuki M, Kageyama K, Tanaka T, et al. New diagnostic criteria of adrenal subclinical Cushing’s syndrome: opinion from the Japan Endocrine Society. Endocr J. 2018;65:383–93.
Spath M, Korovkin S, Antke C, Anlauf M, Willenberg HS. Aldosterone- and cortisol-co-secreting adrenal tumors: the lost subtype of primary aldosteronism. Eur J Endocrinol. 2011;164:447–55.
Nakajima Y, Yamada M, Taguchi R, Satoh T, Hashimoto K, Ozawa A, et al. Cardiovascular complications of patients with aldosteronism associated with autonomous cortisol secretion. J Clin Endocrinol Metab. 2011;96:2512–8.
Peng KY, Liao HW, Chan CK, Lin WC, Yang SY, Tsai YC, et al. Presence of subclinical hypercortisolism in clinical aldosterone-producing adenomas predicts lower clinical success. Hypertension. 2020;76:1537–44.
Gerards J, Heinrich DA, Adolf C, Meisinger C, Rathmann W, Sturm L, et al. Impaired glucose metabolism in primary aldosteronism is associated with cortisol cosecretion. J Clin Endocrinol Metab. 2019;104:3192–202.
Adolf C, Kohler A, Franke A, Lang K, Riester A, Low A, et al. Cortisol excess in patients with primary aldosteronism impacts left ventricular hypertrophy. J Clin Endocrinol Metab. 2018;103:4543–52.
Khan U. Nonfunctioning and subclinical cortisol secreting adrenal incidentalomas and their association with metabolic syndrome: a systematic review. Indian J Endocrinol Metab. 2019;23:332–46.
Wu VC, Hu YH, Wu CH, Kao CC, Wang CY, Yang WS, et al. Administrative data on diagnosis and mineralocorticoid receptor antagonist prescription identified patients with primary aldosteronism in Taiwan. J Clin Epidemiol. 2014;67:1139–49.
Wu VC, Chang HW, Liu KL, Lin YH, Chueh SC, Lin WC, et al. Primary aldosteronism: diagnostic accuracy of the losartan and captopril tests. Am J Hypertens. 2009;22:821–7.
Wu VC, Kuo CC, Wang SM, Liu KL, Huang KH, Lin YH, et al. Primary aldosteronism: changes in cystatin C-based kidney filtration, proteinuria, and renal duplex indices with treatment. J Hypertens. 2011;29:1778–86.
Wu VC, Yang SY, Lin JW, Cheng BW, Kuo CC, Tsai CT, et al. Kidney impairment in primary aldosteronism. Clin Chim Acta. 2011;412:1319–25.
Wu CH, Wu VC, Yang YW, Lin YH, Yang SY, Lin PC, et al. Plasma aldosterone after seated saline infusion test outperforms captopril test at predicting clinical outcomes after adrenalectomy for primary aldosteronism. Am J Hypertens. 2019. https://doi.org/10.1093/ajh/hpz098.
Wu VC, Hu YH, Er LK, Yen RF, Chang CH, Chang YL, et al. Case detection and diagnosis of primary aldosteronism - The consensus of Taiwan Society of Aldosteronism. J Formos Med Assoc. 2017;116:993–1005.
Wu VC, Peng KY, Kuo YP, Liu H, Tan BC, Lin YH, et al. Subtypes of histopathologically classical aldosterone-producing adenomas yield various transcriptomic signaling and outcomes. Hypertension. 2021;78:1791–800.
Lin JH, Peng KY, Kuo YP, Liu H, Tan CB, Lin YF, et al. Aldosterone-producing nodules and CYP11B1 signaling correlate in primary aldosteronism. Endocr Relat Cancer. 2022;29:59–69.
Fassnacht M, Arlt W, Bancos I, Dralle H, Newell-Price J, Sahdev A, et al. Management of adrenal incidentalomas: European Society of Endocrinology Clinical Practice Guideline in collaboration with the European Network for the Study of Adrenal Tumors. Eur J Endocrinol. 2016;175:G1–G34.
Vieira-Correa M, Giorgi RB, Oliveira KC, Hayashi LF, Costa-Barbosa FA, Kater CE. Saliva versus serum cortisol to identify subclinical hypercortisolism in adrenal incidentalomas: simplicity versus accuracy. J Endocrinol Invest. 2019;42:1435–42.
Park J, De Luca A, Dutton H, Malcolm JC, Doyle MA. Cardiovascular outcomes in autonomous cortisol secretion and nonfunctioning adrenal adenoma: a systematic review. J Endocr Soc. 2019;3:996–1008.
American Diabetes A. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2018. Diabetes Care. 2018;41:S13–S27.
Lin YF, Lin SL, Huang TM, Yang SY, Lai TS, Chen L, et al. New-onset diabetes after acute kidney injury requiring dialysis. Diabetes Care. 2018;41:2105–10.
Wu PC, Wu CJ, Lin CJ, Pan CF, Chen CY, Huang TM, et al. Pentoxifylline decreases dialysis risk in patients with advanced chronic kidney disease. Clin Pharmacol Ther. 2015;98:442–9.
Fujimoto K, Honjo S, Tatsuoka H, Hamamoto Y, Kawasaki Y, Matsuoka A, et al. Primary aldosteronism associated with subclinical Cushing syndrome. J Endocrinol Investig. 2013;36:564–7.
Nieman LK, Biller BM, Findling JW, Newell-Price J, Savage MO, Stewart PM, et al. The diagnosis of Cushing’s syndrome: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2008;93:1526–40.
Di Dalmazi G, Vicennati V, Garelli S, Casadio E, Rinaldi E, Giampalma E, et al. Cardiovascular events and mortality in patients with adrenal incidentalomas that are either non-secreting or associated with intermediate phenotype or subclinical Cushing’s syndrome: a 15-year retrospective study. Lancet Diabetes Endocrinol. 2014;2:396–405.
Debono M, Bradburn M, Bull M, Harrison B, Ross RJ, Newell-Price J. Cortisol as a marker for increased mortality in patients with incidental adrenocortical adenomas. J Clin Endocrinol Metab. 2014;99:4462–70.
Mantero F, Armanini D, Boscaro M. Plasma renin activity and urinary aldosterone in Cushing’s syndrome. Horm Metab Res. 1978;10:65–71.
Sugiura Y, Takeo E, Shimma S, Yokota M, Higashi T, Seki T, et al. Aldosterone and 18-oxocortisol coaccumulation in aldosterone-producing lesions. Hypertension. 2018;72:1345–54.
Jin HM, Zhou DC, Gu HF, Qiao QY, Fu SK, Liu XL, et al. Antioxidant N-acetylcysteine protects pancreatic beta-cells against aldosterone-induced oxidative stress and apoptosis in female db/db mice and insulin-producing MIN6 cells. Endocrinology. 2013;154:4068–77.
Sherajee SJ, Fujita Y, Rafiq K, Nakano D, Mori H, Masaki T, et al. Aldosterone induces vascular insulin resistance by increasing insulin-like growth factor-1 receptor and hybrid receptor. Arterioscler Thromb Vasc Biol. 2012;32:257–63.
Hanslik G, Wallaschofski H, Dietz A, Riester A, Reincke M, Allolio B, et al. Increased prevalence of diabetes mellitus and the metabolic syndrome in patients with primary aldosteronism of the German Conn’s Registry. Eur J Endocrinol. 2015;173:665–75.
Hung CS, Chou CH, Liao CW, Lin YT, Wu XM, Chang YY, et al. Aldosterone induces tissue inhibitor of metalloproteinases-1 expression and further contributes to collagen accumulation: from clinical to bench studies. Hypertension. 2016;67:1309–20.
Hung CS, Sung SH, Liao CW, Pan CT, Chang CC, Chen ZW, et al. Aldosterone induces vascular damage. Hypertension. 2019;74:623–9.
Somloova Z, Widimsky J Jr., Rosa J, Wichterle D, Strauch B, Petrak O, et al. The prevalence of metabolic syndrome and its components in two main types of primary aldosteronism. J Hum Hypertens. 2010;24:625–30.
Matrozova J, Steichen O, Amar L, Zacharieva S, Jeunemaitre X, Plouin PF. Fasting plasma glucose and serum lipids in patients with primary aldosteronism: a controlled cross-sectional study. Hypertension. 2009;53:605–10.
Gomez-Sanchez CE. What Is the role of the adipocyte mineralocorticoid receptor in the metabolic syndrome? Hypertension. 2015;66:17–9.
Favero V, Cremaschi A, Falchetti A, Gaudio A, Gennari L, Scillitani A, et al. Management and medical therapy of mild hypercortisolism. Int J Mol Sci. 2021;22:11521–44.
Perogamvros I, Vassiliadi DA, Karapanou O, Botoula E, Tzanela M, Tsagarakis S. Biochemical and clinical benefits of unilateral adrenalectomy in patients with subclinical hypercortisolism and bilateral adrenal incidentalomas. Eur J Endocrinol. 2015;173:719–25.
Acknowledgements
We would like to thank the National Taiwan University Hospital, Taiwan’s National Health Research Institutes, and Taiwan’s Ministry of Science and Technology. We thank the Members of the Taiwan Primary Aldosteronism Investigation (TAIPAI) Study Group.
TAIPAI group
Tai-Shuan Lai7, Shih-Chieh Jeff Chueh7, Shao-Yu Yang7, Kao-Lang Liu7, Chin-Chen Chang7, Bo-Chiag Lee7, Shuo-Meng Wang7, Kuo-How Huang7, Po-Chih Lin7, Yen-Hung Lin7, Lian-Yu Lin7, Shih-Cheng Liao7, Ruoh-Fang Yen7, Ching-Chu Lu7, Chieh-Kai Chan2, Leay-Kiaw Er8, Ya-Hui Hu8, Chia-Hui Chang8, Che-Hsiung Wu8, Yao-Chou Tsai8, Chen-Hsun Ho9, Wei-Chieh Huang10, Ying-Ying Chen11, Vin-Cent Wu12
Funding
This study was supported by the Ministry of Science and Technology (MOST) of the Republic of China (Taiwan) [grant number, MOST 107–2314-B-002-026-MY3, 108-2314-B-002-058, 110-2314-B-002-241, 110-2314-B-002-239], National Science and Technology Council (NSTC) [grant number, NSTC 109-2314-B-002-174-MY3, 110-2314-B-002-124-MY3, 111-2314-B-002-046, 111-2314-B-002-058], National Health Research Institutes [PH-102-SP-09], National Taiwan University Hospital [109-S4634, PC-1246, PC-1309, VN109-09, UN109-041, UN110-030, 111-FTN0011] Grant MOHW 110-TDU-B-212-124005 and Mrs. Hsiu-Chin Lee Kidney Research Fund.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Members of the TAIPAI group are listed below Acknowledgements.
Supplementary Information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wu, VC., Chan, CK., Wu, WC. et al. New-onset diabetes mellitus risk associated with concurrent autonomous cortisol secretion in patients with primary aldosteronism. Hypertens Res 46, 445–455 (2023). https://doi.org/10.1038/s41440-022-01086-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-022-01086-w
Keywords
This article is cited by
-
2023 update and perspectives
Hypertension Research (2024)
-
Autonomous cortisol secretion in patients with primary aldosteronism: A possible risk factor for new-onset diabetes mellitus
Hypertension Research (2023)
-
Prevalence, risk factors and evolution of diabetes mellitus after treatment in primary aldosteronism. Results from the SPAIN-ALDO registry
Journal of Endocrinological Investigation (2023)