Abstract
Angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARBs) are recommended as first-line drugs for hypertension with diabetic nephropathy owing to their renoprotective effect; however, their effect beyond lowering blood pressure (BP) has not been confirmed. Recent studies have shown that aldosterone plays a key role in causing renal injury; therefore, it is likely that mineralocorticoid receptor (MR) blockers inhibit aldosterone-induced renal damage in different ways from ACE inhibitors and ARBs. Therefore, we investigated the mechanism of the effect of an MR blocker on reducing the urinary albumin-to-creatinine ratio (UACR) using data from a randomized, double-blind, placebo-controlled phase 3 study (ESAX-DN) of a new nonsteroidal MR blocker, esaxerenone. This post hoc analysis used a novel statistical method to quantitatively estimate the effect of esaxerenone on UACR reduction mediated, or not mediated, by changes in systolic BP (SBP) and/or estimated glomerular filtration rate (eGFR). The proportion of the mediated effect by SBP changes to the total effect on UACR reduction was 9.8–10.7%; the UACR was reduced to 0.903–0.911 times the baseline at the end of treatment through the SBP-related pathway and to 0.422–0.426 times the baseline through the non-SBP-related pathway. Even considering both SBP and eGFR simultaneously, the proportion of the mediated effect was 21.9–28.1%. These results confirm that esaxerenone has a direct UACR-lowering effect independent of BP lowering and that its magnitude is much larger than that of the BP-dependent effect. Thus, esaxerenone could be a UACR-reducing treatment option for patients with diabetic nephropathy.
Similar content being viewed by others
Introduction
Renin-angiotensin system (RAS) inhibitors, such as angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARBs), are recommended as first-line drugs for hypertensive patients with diabetic nephropathy mainly for their blood pressure (BP)-lowering effects [1]. However, clinical trial data have yet to confirm their renal protective effect beyond lowering BP [2,3,4,5]. Recent studies have shown that aldosterone plays a major pathologic role in causing renal injury [6]; therefore, it is likely that mineralocorticoid receptor (MR) blockers prevent aldosterone-induced renal cell damage in different ways from ACE inhibitors and ARBs [7]. If the unique effect of an MR blocker could be demonstrated, it would help identify new treatment options for hypertension associated with diabetic nephropathy.
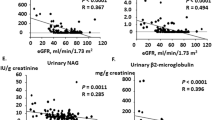
Esaxerenone is a new nonsteroidal MR blocker that has been approved in Japan for the treatment of hypertension and is now under development by Daiichi Sankyo Co., Ltd. for diabetic nephropathy [8]. It has been demonstrated that esaxerenone has renoprotective effects in preclinical and clinical studies [9,10,11,12,13]. In addition, it has been suggested that esaxerenone exerts renoprotective effects independently of its antihypertensive effect in type 2 diabetic mice [14]. A multicenter, randomized, double-blind, placebo-controlled phase 3 trial (ESAX-DN) of esaxerenone confirmed that adding esaxerenone to existing RAS inhibitor therapy significantly reduced the urinary albumin-to-creatinine ratio (UACR) by 61.6% compared with a placebo (geometric least squares mean ratio: 0.384; 95% confidence interval [CI]: 0.334, 0.443) over 52 weeks of treatment in Japanese patients with type 2 diabetes and microalbuminuria [15]. In addition, in another phase 3 study, the UACR decreased by 54.6% (95% CI: 46.9, 61.3) on average from baseline (544.1 mg/g creatinine) to the end of treatment (246.8 mg/g creatinine), and improvement in microalbuminuria was shown in 51.8% of Japanese patients with type 2 diabetes and overt albuminuria during 28 weeks of treatment with esaxerenone [16]. These results clearly show that esaxerenone has a strong UACR-lowering effect in type 2 diabetic patients with albuminuria. Thus, it is now of clinical interest to determine how much of the UACR-lowering effect can be explained by lowering BP or other effects. In the ESAX-DN study, crude correlation analyses were conducted, but no strong correlation was observed between the change in the UACR and the change in BP at the end of treatment. This may indicate that the change in the UACR is irrelevant to the change in BP; however, it does not necessarily indicate that esaxerenone has a UACR-lowering effect independent of BP lowering. To confirm this, further analysis that focuses on the mechanism of the effect of esaxerenone on lowering the UACR is needed. If such an effect is confirmed, it would help to differentiate esaxerenone from other RAS inhibitors as a treatment for diabetic nephropathy.
In statistics, this type of analysis into the mechanism of an agent is called “mediation analysis” and has been used in medical and psychological research [17, 18]. In mediation analysis, the total effect of a treatment on an outcome can be divided into indirect and direct effects; indirect effects act through mediators of interest, whereas direct effects act through other pathways and not through mediators of interest [17,18,19]. Several novel methods to identify indirect and direct effects have been proposed based on the counterfactual-based framework [20, 21]. These statistical methods are practically useful for addressing clinical questions but have not yet been widely used in clinical research.
This post hoc analysis investigated whether esaxerenone has a UACR-lowering effect independent of BP lowering and quantitatively assessed its magnitude using data from the ESAX-DN study. In addition, this analysis aimed to determine whether esaxerenone can be a treatment option for patients with diabetic nephropathy.
Methods
The reporting of this post hoc mediation analysis is in accordance with the consensus-based guidance for the reporting of mediation analyses of randomized trials and observational studies (A Guideline for Reporting Mediation Analyses; AGReMA Statement) [22].
Study design and population
This was a post hoc analysis of a multicenter, randomized, double-blind, placebo-controlled phase 3 trial (JapicCTI-173695), the ESAX-DN study [15]. The study protocol of the ESAX-DN study was approved by the local institutional review board at each participating site and conducted in accordance with the principles of the Declaration of Helsinki and the ICH E6 Guideline for Good Clinical Practice (CPMP/ICH/135/95). All the participants in the ESAX-DN study provided written informed consent prior to enrollment.
In the ESAX-DN study, patients were randomized to either esaxerenone or placebo treatment for 52 weeks after a 4-week run-in period, continuing their treatment with RAS inhibitors at a constant dosage throughout the study. To minimize the risk of increasing serum potassium (K+) levels, esaxerenone or its placebo treatment was started at a dosage of 1.25 mg/d and then titrated to 2.5 mg/d if the serum K+ level of each patient was acceptable. Other details of the study population, such as the inclusion and exclusion criteria, have been previously published [15].
Outcomes
The primary endpoint of the ESAX-DN study was the proportion of patients with UACR remission at the end of treatment, and the key secondary endpoint was the percentage change in the UACR from baseline at the end of treatment. The changes in BP and creatinine levels and the rate of transition to overt albuminuria were also assessed. Safety endpoints included adverse events, serum K+ levels, percentage changes in eGFR from baseline to the end of treatment and time-course changes in eGFR.
Of these outcomes, data for the percentage changes in the UACR from baseline to the end of treatment, changes in BP, and changes in eGFR were used in this post hoc analysis.
Assessments
The UACR, calculated from first morning urine samples, was measured during the run-in period and every 4 weeks up to week 52 during the subsequent treatment period. BP and eGFR were monitored every 2 weeks up to week 8 and every 4 weeks from week 12 to week 52 during the treatment period. The eGFR with the modification in diet in renal disease was calculated using the formula modified by the Japanese Society of Nephrology [23]. Other details of the study visits and assessments have been previously reported [15].
Clinical assumptions
Several mechanisms may explain the renoprotective effect of esaxerenone. First, esaxerenone primarily reduces BP, which then leads to a reduction in glomerular pressure, and it can also reduce urinary albumin excretion. Second, esaxerenone may directly affect renal function and may also affect urinary albumin excretion. In addition to these mechanisms, esaxerenone may have other effects on albuminuria suppression.
Based on these clinical assumptions, we considered SBP and eGFR as mediators that reflect the changes in BP and renal function and assumed the following causal relationships between the variables in this analysis (Fig. 1a). There are four possible pathways through which treatment affects UACR changes: pathways through SBP or eGFR (i.e., treatment-SBP-UACR, treatment-SBP-eGFR-UACR, treatment-eGFR-UACR) and a pathway through neither SBP nor eGFR (i.e., treatment-UACR). The former are indirect effects, and the latter the direct effect (our primary interest in this analysis). When SBP or eGFR are considered separately, the causal relationships are simplified to only two pathways: an indirect effect through SBP or eGFR and a direct effect not through SBP or eGFR (Fig. 1b, c).
The values of SBP and eGFR change longitudinally during treatment. In addition, SBP and eGFR may affect UACR changes in different manners. Therefore, to incorporate the changes in SBP and eGFR during treatment, two types of mediator variables were considered: the cumulative average value of change from baseline up to the end of treatment and the achieved value of change from baseline to just before the end of treatment. The former assumes a cumulative effect, and the latter assumes an acute effect of mediator variables on the outcome.
Statistical analysis
To quantitatively investigate direct and indirect effects, we used the concepts of the “natural direct” effect and the “indirect effect” [20]. The natural direct effect is defined as the between-treatment comparison of the effect on the outcome if the mediator levels were set to what they would have been if the control treatment (e.g., placebo) was initiated. The natural indirect effect is defined as the comparison of the mediator effect on the outcome between mediator levels that would have been observed under the experimental or control treatment while the treatment was set to the experimental treatment (e.g., esaxerenone). The sum of natural direct and indirect effects is the total effect defined as the treatment effect comparison between when all subjects had experimental treatment and when all subjects had control treatment, the so-called intention-to-treat (ITT) effect in randomized trials. Further detailed explanations based on the causal inference framework are included in Supplementary Text 1.
Some strong assumptions are required to identify natural direct and indirect effects: (i) no unmeasured confounding of the exposure-outcome relationship; (ii) no unmeasured confounding of the outcome-mediator relationship; (iii) no unmeasured confounding of the exposure-mediator relationship; and (iv) no mediator-outcome confounder that is itself affected by the exposure. In randomized studies such as the ESAX-DN study, assumptions (i) and (iii) would hold because of the randomization of the treatment, but (ii) and (iv) would not necessarily hold and cannot be confirmed by the data.
To overcome this problem with the assumptions, a methodology with multiple mediators was considered in this analysis. The confounder for the mediator-outcome relationship was considered the mediator, and the joint indirect effect of all mediators was estimated [20]. Another advantage of this method is that we do not need to specify the causal relationships between mediators (i.e., BP and eGFR in this analysis).
To estimate the natural direct and indirect effects, we used the regression-based approach for single mediator and multiple mediator settings (details are shown in Supplementary Text 2). In the multivariate linear regression model, we included the treatment, mediator(s), interaction between treatment and mediator(s), and baseline covariates (i.e., baseline values of the UACR and mediators) as confounders.
In addition to the direct and indirect effects, the proportion of the mediated effect was calculated as (indirect effect/total effect) × 100 (%), which expresses how much of the total effect is mediated through mediators. The CIs for estimates were constructed based on the bootstrap method with 1000 replications.
As in the ESAX-DN study, the log-transformed UACR was used in the analyses and back-transformed and expressed in the original scale in the results (i.e., the effect on UACR reduction was expressed as the geometric mean ratio to baseline, compared with placebo). All statistical analyses were performed using SAS System Release 9.4 (SAS Institute Japan Ltd., Tokyo, Japan).
Results
Patients
A total of 455 patients were randomized, but 6 patients were excluded from the full analysis set (n = 449) due to missing primary endpoints. All the patients in the full analysis set were included in this post hoc analysis. Detailed information on patient characteristics and the time-course changes in the UACR, BP, and eGFR have been previously reported [15].
Direct and indirect effects
The total effect, the placebo-adjusted geometric mean ratio to baseline, was 0.385, indicating that esaxerenone reduced the UACR to 0.385 times the baseline compared to placebo in total. We attempted to decompose this total effect of 0.385 into indirect and direct effects using mediation analysis.
The results are summarized in Table 1, 2. When the cumulative means of SBP and eGFR were considered separately (Table 1), the indirect effect of SBP was 0.911 (95% CI: 0.831, 0.987), and the direct effect was 0.422 (95% CI: 0.351, 0.497), indicating that the total effect of 0.385 was divided into 0.911 × 0.422. An alternative explanation is that esaxerenone reduced the UACR to 0.911 times the baseline through BP-related pathways and to 0.422 times the baseline through non-BP-related pathways at the end of treatment. The proportion of the mediated effect by SBP was 9.8% (95% CI: 2.0, 20.1). The indirect effect of eGFR was 0.793 (95% CI: 0.721, 0.864), the direct effect was 0.485 (95% CI: 0.417, 0.569), and the proportion of the mediated effect through the eGFR-related pathway was 24.3% (95% CI: 16.3, 34.8). Although the indirect effect of eGFR was slightly larger than that of SBP, the proportion of the mediated effect was not very large, even for eGFR. Both for SBP and eGFR, the results were almost consistent with respect to the type of variable (i.e., cumulative mean or achieved value): proportions of the mediated effect were 10.7% (95% CI: 4.6, 19.2) and 16.4% (95% CI: 10.6, 25.3) for the SBP-related pathway and for the eGFR-related pathway, respectively. However, there seems to be a tendency for eGFR to have a cumulative effect (i.e., 24.3% vs. 16.4%) compared to SBP (i.e., 9.8% vs. 10.7%).
When SBP and eGFR were considered simultaneously (Table 2), the proportion of the mediated effect was 28.1% (95% CI: 18.2, 41.4); the indirect effect of esaxerenone on UACR reduction mediated by SBP and/or eGFR changes was 0.765 (95% CI: 0.677, 0.838), and the direct effect mediated neither by SBP nor eGFR changes was 0.503 (95% CI: 0.424, 0.596) at the end of treatment. This means that esaxerenone reduced the UACR mostly by the pathways that are relevant to neither SBP nor eGFR changes. Similar to the single mediator analysis, the results were almost the same with respect to the type of variable, although there seemed to be a trend for a cumulative effect, possibly owing to the effect of eGFR.
Even when diastolic BP (DBP) or mean arterial pressure (MAP) was considered instead of SBP, the results were almost the same; the mediated effect by DBP or MAP accounted for a small portion of the total effect (Supplementary Table 1).
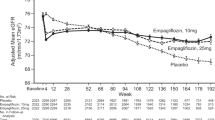
Although we consider the end of treatment as the primary time point of interest, the longitudinal effect is also worth investigating, as the ESAX-DN study showed different patterns in the longitudinal changes in the UACR, SBP, and eGFR; the UACR decreased slowly until week 24 and remained stable until the end of treatment, incremental reductions in SBP were observed up to approximately week 28 or week 32, and eGFR continued to decrease until week 24 and then remained stable in the esaxerenone group [15]. To investigate longitudinal changes in the effect of esaxerenone, we repeated the same analysis changing the endpoint from week 4 to week 52. In this supportive analysis, only patients who had a UACR value at each time point were included in the analysis; therefore, the number of patients analyzed differed slightly among time points. There was some variability in the proportion of the mediated effect; however, the results showed that most effects were consistently independent of SBP and/or eGFR changes (Fig. 2). This indicates that our findings are robust with respect to the treatment duration.
Changes in the proportion of the mediated effect by treatment duration. Changes in the proportion of the mediated effect (%) for different time points from week 4 up to week 52; SBP and eGFR separately (a, b), SBP and eGFR simultaneously (c). SBP systolic blood pressure, eGFR estimated glomerular filtration rate, EOT end of treatment
In addition, we also conducted subgroup analyses to investigate subgroup differences in the proportion of mediated effects with respect to sex (male, female), obesity (Body Mass Index < 25, 25 ≤ [kg/m2]) and diabetes status (HbA1c < 7.4, 7.4 ≤ [%]), baseline UACR (<100, 100 ≤ [mg/g Cr]), baseline eGFR (<60, 60 ≤ [mL/min/1.73 m2]), DPP4 inhibitor use (yes, no), and SGLT2 inhibitor use (yes, no). The results are almost consistent among subgroups in that the majority of the total effect was not mediated by SBP changes (Supplementary Table 2). This might support the generalizability of our findings, although there may be a sample size limitation, and the assumptions for this mediation analysis may not be valid for some subgroups.
Discussion
In this post hoc analysis, we quantitatively investigated whether esaxerenone has a UACR-lowering effect independent of lowering BP, applying a novel statistical methodology to the results of a pivotal phase 3 study, ESAX-DN. To the best of our knowledge, this is the first study to use mediation analysis to investigate the direct and indirect effects of an MR blocker on lowering the UACR via, and not via, lowering BP using clinical trial data. The results show that most of the UACR-lowering effect of esaxerenone is induced by a pathway independent of BP changes, even considering eGFR changes. This suggests that esaxerenone has a UACR-lowering effect beyond lowering BP in patients with microalbuminuria.
This post hoc analysis statistically confirmed that esaxerenone has a direct UACR-lowering effect not mediated through lowering BP; however, the actual mechanism by which esaxerenone directly induces an antialbuminuric effect is not clear from this analysis. As discussed in a previous paper [13], sodium depletion may be one possible mechanism. In addition, preclinical studies have shown that MRs are involved in salt-induced organ damage that is independent of plasma aldosterone levels [24]. Thus, the direct effect of esaxerenone on UACR reduction may be largely due to MR blockade.
There are various discussions in the literature about microalbuminuria changes as a surrogate endpoint of diabetic kidney disease [25]. Two recent meta-analyses reported that a > 30% reduction in albuminuria confers substantial risk reduction for end-stage kidney disease [26, 27]. This post hoc analysis confirmed that esaxerenone has a strong direct effect on UACR reduction (57.4–57.8% relative to placebo) and therefore that the magnitude of the direct effect that is independent of BP changes can be considered clinically significant in terms of the prevention of end-stage kidney disease.
There are several methodologies that can directly handle multiple and/or time-dependent mediators [21, 28, 29]. However, such methods are often not practical, as they require additional assumptions, and their estimation is complicated. Therefore, more practical approaches using multiple and/or time-dependent mediators are desirable, as used in this analysis. Our main analysis and supportive analysis are probably sufficient for the ESAX-DN data, as the indirect mediating effect is relatively small.
The current analysis has several limitations. This was a post hoc analysis with no prespecified analysis plan, and the sample size of the ESAX-DN study was not designed for use in a mediation analysis. However, the sample size is probably sufficient in terms of the precision of the mediation analysis, as the CIs of the estimates were sufficiently narrow. Second, the ESAX-DN study involved only Japanese patients; thus, generalizability of the findings to other ethnic populations may be limited. In addition, the ESAX-DN data were limited to esaxerenone; therefore, we cannot determine if our findings are unique to esaxerenone or applicable to other MR blockers. Further research is needed to address these clinical questions using data from a broader population.
In conclusion, esaxerenone has a UACR-lowering effect beyond lowering BP and thus can be a treatment option for diabetic nephropathy in patients with albuminuria.
Data availability
Deidentified individual participant data and applicable supporting clinical study documents may be available upon request at https://vivli.org/. In cases where clinical study data and supporting documents are provided pursuant to our company policies and procedures, Daiichi Sankyo Co., Ltd. will continue to protect the privacy of our clinical study participants. Details on the data sharing criteria and the procedure for requesting access are available at https://vivli.org/ourmember/daiichi-sankyo/.
References
Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension guidelines for the management of hypertension (JSH 2019). Hypertens Res. 2019;42:1235–481.
Casas JP, Chua W, Loukogeorgakis S, Vallance P, Smeeth L, Hingorani AD, et al. Effect of inhibitors of the renin-angiotensin system and other antihypertensive drugs on renal outcomes: systematic review and meta-analysis. Lancet. 2005;366:2026–33.
Daien V, Duny Y, Ribstein J, du Cailar G, Mimran A, Villain M, et al. Treatment of hypertension with renin-angiotensin system inhibitors and renal dysfunction: a systematic review and meta-analysis. Am J Hypertens. 2012;25:126–32.
Te Riet L, van Esch JH, Roks AJ, van den Meiracker AH, Danser AH. Hypertension: renin-angiotensin-aldosterone system alterations. Circ Res. 2015;116:960–75.
Bavishi C, Bangalore S, Messerli FH. Renin angiotensin aldosterone system inhibitors in hypertension: is there evidence for benefit independent of blood pressure reduction? Prog Cardiovasc Dis. 2016;59:253–61.
Spencer S, Wheeler-Jones C, Elliott J. Aldosterone and the mineralocorticoid receptor in renal injury: a potential therapeutic target in feline chronic kidney disease. J Vet Pharm Ther. 2020;43:243–67.
Hargovan M, Ferro A. Aldosterone synthase inhibitors in hypertension: current status and future possibilities. JRSM Cardiovasc Dis. 2014;3:2048004014522440. https://doi.org/10.1177/2048004014522440.
Duggan S. Esaxerenone: First Global Approval. Drugs. 2019;79:477–81.
Li L, Guan Y, Kobori H, Morishita A, Kobara H, Masaki T, et al. Effects of the novel nonsteroidal mineralocorticoid receptor blocker, esaxerenone (CS-3150), on blood pressure and urinary angiotensinogen in low-renin Dahl salt-sensitive hypertensive rats. Hypertens Res. 2019;42:769–78.
Arai K, Tsuruoka H, Homma T. CS-3150, a novel non-steroidal mineralocorticoid receptor antagonist, prevents hypertension and cardiorenal injury in Dahl salt-sensitive hypertensive rats. Eur J Pharm. 2015;769:266–73.
Arai K, Morikawa Y, Ubukata N, Tsuruoka H, Homma T. CS-3150, a novel nonsteroidal mineralocorticoid receptor antagonist, shows preventive and therapeutic effects on renal injury in deoxycorticosterone acetate/salt-induced hypertensive rats. J Pharm Exp Ther. 2016;358:548–57.
Itoh H, Ito S, Rakugi H, Okuda Y, Nishioka S. Efficacy and safety of dosage-escalation of low-dosage esaxerenone added to a RAS inhibitor in hypertensive patients with type 2 diabetes and albuminuria: a single-arm, open-label study. Hypertens Res. 2019;42:1572–81.
Ito S, Shikata K, Nangaku M, Okuda Y, Sawanobori T. Efficacy and safety of esaxerenone (CS-3150) for the treatment of type 2 diabetes with microalbuminuria: a randomized, double-blind, placebo-controlled, phase II trial. Clin J Am Soc Nephrol. 2019;14:1161–72.
Arai K, Morikawa Y, Ubukata N, Sugimoto K. Synergistic reduction in albuminuria in type 2 diabetic mice by esaxerenone (CS-3150), a novel nonsteroidal selective mineralocorticoid receptor blocker, combined with an angiotensin II receptor blocker. Hypertens Res. 2020;43:1204–13.
Ito S, Kashihara N, Shikata K, Nangaku M, Wada T, Okuda Y, et al. Esaxerenone (CS-3150) in patients with type 2 diabetes and microalbuminuria (ESAX-DN): phase 3 randomized controlled clinical trial. Clin J Am Soc Nephrol. 2020;15:1715–27.
Ito S, Kashihara N, Shikata K, Nangaku M, Wada T, Okuda Y, et al. Efficacy and safety of esaxerenone (CS-3150) in Japanese patients with type 2 diabetes and macroalbuminuria: a multicenter, single-arm, open-label phase III study. Clin Exp Nephrol. 2021;25:1070–8.
VanderWeele TJ. Explanation in Causal Inference: Methods for Mediation and Interaction. Oxford University Press: New York, USA, 2015.
Lee H, Herbert RD, McAuley JH. Mediation analysis. JAMA. 2019;321:697–8.
Vansteelandt S. Understanding counterfactual-based mediation analysis approaches and their differences. Epidemiology. 2012;23:889–91.
VanderWeele TJ, Vansteelandt S. Mediation analysis with multiple mediators. Epidemiol Methods. 2014;2:95–115.
Vansteelandt S, Daniel RM. Interventional effects for mediation analysis with multiple mediators. Epidemiology. 2017;28:258–65.
Lee H, Cashin AG, Lamb SE, Hopewell S, Vansteelandt S, VanderWeele TJ, et al. A Guideline for Reporting Mediation Analyses of Randomized Trials and Observational Studies: the AGReMA Statement. JAMA. 2021;326:1045–56.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–92.
Nagase M, Matsui H, Shibata S, Gotoda T, Fujita T. Salt-induced nephropathy in obese spontaneously hypertensive rats via paradoxical activation of the mineralocorticoid receptor: role of oxidative stress. Hypertension. 2007;50:877–83.
Tuttle KR, Bakris GL, Bilous RW, Chiang JL, de Boer IH, Goldstein-Fuchs J, et al. Diabetic kidney disease: a report from an ADA Consensus Conference. Diabetes Care. 2014;37:2864–83.
Heerspink HJL, Greene T, Tighiouart H, Gansevoort RT, Coresh J, Simon AL, et al. Change in albuminuria as a surrogate endpoint for progression of kidney disease: a meta-analysis of treatment effects in randomised clinical trials. Lancet Diabetes Endocrinol. 2019;7:128–39.
Coresh J, Heerspink HJL, Sang Y, Matsushita K, Arnlov J, Astor BC, et al. Change in albuminuria and subsequent risk of end-stage kidney disease: an individual participant-level consortium meta-analysis of observational studies. Lancet Diabetes Endocrinol. 2019;7:115–27.
VanderWeele TJ, Tchetgen Tchetgen EJ. Mediation analysis with time varying exposures and mediators. J R Stat Soc Ser B Stat Methodol. 2017;79:917–38.
Yamamuro S, Shinozaki T, Iimuro S, Matsuyama Y. Mediational g-formula for time-varying treatment and repeated-measured multiple mediators: application to atorvastatin’s effect on cardiovascular disease via cholesterol lowering and anti-inflammatory actions in elderly type 2 diabetics. Stat Methods Med Res. 2021;30:1782–99.
Acknowledgements
The authors would like to thank all the people who participated in this study and the reviewers for their useful and helpful comments on our manuscript. We also thank Diane Williams, PhD, of Edanz (www.edanz.com) for the editorial check of this manuscript.
Funding
The ESAX-DN study and this post hoc analysis were funded by Daiichi Sankyo Co., Ltd.
Author information
Authors and Affiliations
Contributions
Conceptualization, investigation: all authors. Statistical plan and analysis: YO and MT. All authors agree with the final version of the manuscript, the publication in this journal, and to be held accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
YO and TS are employees of Daiichi Sankyo Co., Ltd. SI, NK, KS, MN and TW have received personal fees from Daiichi Sankyo Co., Ltd., and MT has received consultant fees from Daiichi Sankyo Co., Ltd. NK, KS and MN have received grants/research funding from Daiichi Sankyo Co., Ltd.
Additional information
Publisher note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Okuda, Y., Ito, S., Kashihara, N. et al. The renoprotective effect of esaxerenone independent of blood pressure lowering: a post hoc mediation analysis of the ESAX-DN trial. Hypertens Res 46, 437–444 (2023). https://doi.org/10.1038/s41440-022-01008-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-022-01008-w
Keywords
This article is cited by
-
2023 update and perspectives
Hypertension Research (2024)
-
Exploratory study on the relationship between urinary sodium/potassium ratio, salt intake, and the antihypertensive effect of esaxerenone: the ENaK Study
Hypertension Research (2024)
-
Nighttime home blood pressure lowering effect of esaxerenone in patients with uncontrolled nocturnal hypertension: the EARLY-NH study
Hypertension Research (2023)
-
Is esaxerenone the ultimate mineralocorticoid receptor antagonist?
Hypertension Research (2023)
-
Esaxerenone for nocturnal hypertension and possible future direction for treatment of hypertension-cardiovascular-kidney comorbidity
Hypertension Research (2023)