Abstract
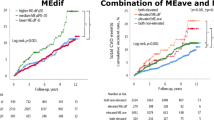
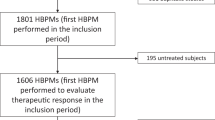
The predictive power of home blood pressure (BP) in the evening compared with home BP in the morning and office BP has been controversial. The predictive power of evening BP was compared to that of morning BP and office BP. The likelihood ratio test between one model containing a single BP index with traditional risk factors and a similar model further containing another BP index was used to assess whether the additional BP index significantly improved the adequacy of the model. Of 3266 patients with mild-to-moderate hypertension who were on antihypertensive medications (men 50.6%, age 59.5 ± 10.0 years), 58 experienced a major adverse cardiovascular event during a median follow-up of 7.1 years. The hazard ratios for a one standard deviation increment of evening home systolic/diastolic BP were 1.26 (0.98–1.62)/1.43 (1.09–1.88) in the baseline untreated period and 1.46 (1.17–1.81)/1.63 (1.26–2.11) during the on-treatment follow-up period. When evening BP at baseline and that during follow-up were included in the same model, only the latter significantly improved the prediction models (P = 0.006/0.005 for systolic/diastolic BP). Then, evening home BP vs. morning BP during follow-up was tested. The former did not improve the prediction models (P > 0.2), but the latter significantly improved the models (P ≤ 0.048). Similarly, when evening home BP and office BP during follow-up were analyzed, only the former significantly improved the prediction models (P ≤ 0.015). In conclusion, evening BP could be a more potent predictor than office BP, but it was inferior compared to morning BP in the treatment of mild-to-moderate hypertensive patients.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Change history
19 April 2022
A Correction to this paper has been published: https://doi.org/10.1038/s41440-022-00917-0
References
The Ministry of Health, Labour and Welfare. Vital statistics Japan. Tokyo: The Ministry of Health, Labour and Welfare; 2018.
Ikeda N, Inoue M, Iso H, Ikeda S, Satoh T, Noda M, et al. Adult mortality attributable to preventable risk factors for non-communicable diseases and injuries in Japan: a comparative risk assessment. PLoS Med. 2012;9:e1001160.
Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens Res. 2019;42:1235–481.
The Ministry of Health, Labour and Welfare: Tokyo. The National Health and Nutrition Survey in Japan, 2010. 2012.
Imai Y, Obara T, Asamaya K, Ohkubo T. The reason why home blood pressure measurements are preferred over clinic or ambulatory blood pressure in Japan. Hypertens Res. 2013;36:661–72.
Imai Y, Nishiyama A, Sekino M, Aihara A, Kikuya M, Ohkubo T, et al. Characteristics of blood pressure measured at home in the morning and in the evening: the Ohasama study. J Hypertens. 1999;17:889–98.
Ito K, Obara T, Ohkubo T, Gonokami K, Shinki T, Shibamiya T, et al. Influence of home blood pressure measuring conditions in the evening on the morning-evening home blood pressure difference in treated hypertensive patients: the J-HOME study. Blood Press Monit. 2009;14:160–5.
Aparicio LS, Barochiner J, Cuffaro PE, Alfie J, Rada MA, Morales MS, et al. Determinants of the morning-evening home blood pressure difference in treated hypertensives: the HIBA-Home Study. Int J Hypertens. 2014;2014:569259.
Johansson JK, Niiranen TJ, Puukka PJ, Jula AM. Factors affecting the difference between morning and evening home blood pressure: the Finn-Home study. Blood Press. 2011;20:27–36.
Chonan K, Hashimoto J, Ohkubo T, Tsuji I, Nagai K, Kikuya M, et al. Insufficient duration of action of antihypertensive drugs mediates high blood pressure in the morning in hypertensive population: the Ohasama study. Clin Exp Hypertens. 2002;24:261–75.
Ménard J, Chatellier G, Day M, Vaur L. Self-measurement of blood pressure at home to evaluate drug effects by the trough: peak ratio. J Hypertens Suppl. 1994;12:S21–5.
Hoshide S, Yano Y, Haimoto H, Yamagiwa K, Uchiba K, Nagasaka S, et al. Morning and evening home blood pressure and risks of incident stroke and coronary artery disease in the japanese general practice population: the Japan Morning Surge-Home Blood Pressure Study. Hypertension. 2016;68:54–61.
Asayama K, Ohkubo T, Kikuya M, Obara T, Metoki H, Inoue R, et al. Prediction of stroke by home “morning” versus “evening” blood pressure values: the Ohasama study. Hypertension. 2006;48:737–43.
Niiranen TJ, Johansson JK, Reunanen A, Jula AM. Optimal schedule for home blood pressure measurement based on prognostic data: the Finn-Home Study. Hypertension. 2011;57:1081–6.
Hansson L, Hedner T, Dahlöf B. Prospective randomized open blinded end-point (PROBE) study. A novel design for intervention trials. Prospective randomized open blinded end-point. Blood Press. 1992;1:113–9.
Asayama K, Ohkubo T, Metoki H, Obara T, Inoue R, Kikuya M, et al. Cardiovascular outcomes in the first trial of antihypertensive therapy guided by self-measured home blood pressure. Hypertens Res. 2012;35:1102–10.
World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310:2191–4.
Watabe D, Asayama K, Hanazawa T, Hosaka M, Satoh M, Yasui D, et al. Predictive power of home blood pressure indices at baseline and during follow-up in hypertensive patients: HOMED-BP study. Hypertens Res. 2018;41:622–8.
Imai Y, Ohkubo T, Kikuya M, Hashimoto J. Practical aspect of monitoring hypertension based on self-measured blood pressure at home. Intern Med. 2004;43:771–8.
Chonan K, Kikuya M, Araki T, Fujiwara T, Suzuki M, Michimata M, et al. Device for the self-measurement of blood pressure that can monitor blood pressure during sleep. Blood Press Monit. 2001;6:203–5.
Staessen J, Bulpitt C, Clement D, De Leeuw P, Fagard R, Fletcher A, et al. Relation between mortality and treated blood pressure in elderly patients with hypertension: report of the European Working Party on High Blood Pressure in the Elderly. BMJ. 1989;298:1552–6.
White WB, Anwar YA. Evaluation of the overall efficacy of the Omron office digital blood pressure HEM-907 monitor in adults. Blood Press Monit. 2001;6:107–10.
Seino Y, Nanjo K, Tajima N, Kadowaki T, Kashiwagi A, Araki E, et al. Report of the committee on the classification and diagnostic criteria of diabetes mellitus. J Diabetes Investig. 2010;1:212–28.
Woodward M. Epidemiology: study design and data analysis. London: Chapman and Hall/CRC Texts in Statistical Science; 2005.
Stergiou GS, Nasothimiou EG, Kalogeropoulos PG, Pantazis N, Baibas NM. The optimal home blood pressure monitoring schedule based on the Didima outcome study. J Hum Hypertens. 2010;24:158–64.
Asayama K, Tabara Y, Oishi E, Sakata S, Hisamatsu T, Godai K, et al. Recent status of self-measured home blood pressure in the Japanese general population: a modern database on self-measured home blood pressure (MDAS). Hypertens Res. 2020. https://doi.org/10.1038/s41440-020-0530-1.
Obara T, Ohkubo T, Fukunaga H, Kobayashi M, Satoh M, Metoki H, et al. Practice and awareness of physicians regarding home blood pressure measurement in Japan. Hypertens Res. 2010;33:428–34.
Li W, Jin C, Vaidya A, Wu Y, Rexrode K, Zheng X, et al. Blood pressure trajectories and the risk of intracerebral hemorrhage and cerebral infarction: a prospective study. Hypertension. 2017;70:508–14.
Böhm M, Schumacher H, Teo KK, Lonn EM, Mahfoud F, Mann JFE, et al. Achieved blood pressure and cardiovascular outcomes in high-risk patients: results from ONTARGET and TRANSCEND trials. Lancet. 2017;389:2226–37.
Hansson L, Zanchetti A, Carruthers SG, Dahlöf B, Elmfeldt D, Julius S, et al. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. HOT Study Group. Lancet. 1998;351:1755–62.
Sprint Research Group, Wright JT Jr., Williamson JD, Whelton PK, Snyder JK, Sink KM, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373:2103–16.
Ohkubo T, Asayama K, Kikuya M, Metoki H, Hoshi H, Hashimoto J, et al. How many times should blood pressure be measured at home for better prediction of stroke risk? Ten-year follow-up results from the Ohasama study. J Hypertens. 2004;22:1099–104.
Niiranen TJ, Hänninen MR, Johansson J, Reunanen A, Jula AM. Home-measured blood pressure is a stronger predictor of cardiovascular risk than office blood pressure: the Finn-Home study. Hypertension. 2010;55:1346–51.
Niiranen TJ, Asayama K, Thijs L, Johansson JK, Ohkubo T, Kikuya M, et al. Outcome-driven thresholds for home blood pressure measurement: international database of home blood pressure in relation to cardiovascular outcome. Hypertension. 2013;61:27–34.
Acknowledgements
The authors are grateful to all the HOMED-BP study collaborators as listed previously [16] for their valuable contributions. The authors would also like to thank the staff of Tohoku University and Teikyo University for their valuable help and Fujitsu Systems East Limited (Tokyo, Japan) and Omron Healthcare Co., Ltd (Kyoto, Japan), who developed and maintained the internet-based infrastructure for the measurement of blood pressure at home and the management of patients.
Funding
This study was funded by grants from the Japan Cardiovascular Research Foundation, the Japan Arteriosclerosis Prevention Fund, and Tohoku University. This study was also supported by Grants-in-Aid for Scientific Research (16K15359, 17H04126, and 18K06759) from the Ministry of Education, Culture, Sports, Science and Technology, and ACRO Incubation Grants of Teikyo University. No funding agencies had any role in the design or conduct of the study, in the collection, analysis, or interpretation of the data, or in the preparation, review, or approval of the manuscript.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
KA, YI, and TO were concurrent directors of the Tohoku Institute for Management of Blood Pressure, which was supported by Omron Healthcare Co., Ltd. The remaining authors have no disclosures to report.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: In the sentence beginning ‘A total of 252 patients’ in this article, the term ‘office BP at baseline’, and the number of patients ‘n = 7’ and ‘n = 5’ should have read ‘office BP at follow-up’, ‘n = 5’, and ‘ n = 7’, respectively.
Supplementary information
Rights and permissions
About this article
Cite this article
Uchida, S., Kikuya, M., Asayama, K. et al. Predictive power of home blood pressure in the evening compared with home blood pressure in the morning and office blood pressure before treatment and in the on-treatment follow-up period: a post hoc analysis of the HOMED-BP study. Hypertens Res 45, 722–729 (2022). https://doi.org/10.1038/s41440-022-00860-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-022-00860-0