Abstract
The prognostic value of home blood pressure monitoring (HBPM) has been investigated in several studies in the general population, demonstrating its independent association with cardiovascular events. However, in the case of treated hypertensive subjects, evidence is controversial. Our purpose was to evaluate the prognostic value of HBPM in this population. Medicated hypertensive patients who performed a 4-day HBPM (Omron® HEM-705CP-II) between 2008 and 2015 were followed up for a median of 5.9 years, registering the occurrence of a composite primary outcome of fatal and non-fatal cardiovascular events. Cox regression models were used to analyze the prognostic value of HBPM, considering 4-day measurements, discarding the first day, and analyzing morning, afternoon and evening periods separately. We included 1582 patients in the analysis (33.4% men, median age 70.8 years, on an average of 2.1 antihypertensive drugs). During follow-up, 273 events occurred. HBPM was significantly associated with cardiovascular events in all five scenarios in the unadjusted models. When adjusting for office BP and other cardiovascular risk factors, the association remained marginally significant for the 4-day period, discarding first-day measurements HBPM (HR 1.04 [95% CI 1–1.1] and 1.04 [95% CI 1–1.1], respectively) and statistically significant for all separate periods of measurement: HR 1.32 (95% CI 1.01–1.72); 1.33 (95% CI 1.02–1.72); and 1.30 (95% CI 1.01–1.67), for morning, afternoon and evening, respectively. When analyzing separately fatal and non-fatal events, statistical significance was held for the former only. In conclusion, HBPM is an independent predictor of cardiovascular events in hypertensives under treatment.
Similar content being viewed by others
Introduction
Out-of-office blood pressure (BP) measurement is currently considered crucial in the management of hypertensive patients [1, 2]. Among the two recommended techniques—ambulatory blood pressure monitoring (ABPM) and home blood pressure monitoring (HBPM)—the latter has been repositioned as an invaluable tool in the context of COVID-19 pandemic since it is similar (and better tolerated) than ABPM in clinical practice and can be entirely performed in the patient’s home [3].
The prognostic value of HBPM has been investigated in several studies conducted in the general population which demonstrated the independent association of baseline HBPM with cardiovascular events [4,5,6]. However, in the case of hypertensive subjects who are already under treatment, evidence is less overwhelming, since not only is it scanter but there are also methodological issues that preclude the generalization of the findings. For instance, some studies evaluated only a kind of antihypertensive treatment, i.e., angiotensin receptor blockers [7, 8]; other studies failed to find significant results for the primary endpoint for which they were designed [9], and others did not make an adjustment for office blood pressure [9, 10]. In fact, recent hypertension guidelines state that there is a gap in the evidence regarding the incremental benefit for cardiovascular risk prediction of the addition of out-of-office BP to office BP measurement [2]. Therefore, we aimed at evaluating the prognostic value of HBPM, in terms of cardiovascular events, in hypertensive patients under treatment.
Materials and methods
Study population
This was a cohort study that included hypertensive patients, according to established criteria in national and international guidelines [1, 2, 11], who were 18 years or older and under stable antihypertensive treatment for at least 4 weeks. Participants performed a baseline HBPM, prescribed by their treating physician, between September, 1, 2008 and December, 31, 2015, in the Hypertension Section of Hospital Italiano de Buenos Aires. Duplicate HBPMs as well as HBPMs with less than 16 readings were excluded from the analysis.
The design of the study complied with the Code of Ethics of the World Medical Association (Declaration of Helsinki, 1964 and Declaration of Tokyo, 1975, as revised in 2008). The study protocol was approved by the local ethics committee. The patients duly authorized the use of the information in their medical records under the protection of their confidentiality through informed consent.
Home blood pressure monitoring
We used an automatic oscillometric device, Omron 705 CP (Omron® HEM-705CP-II, Omron®,Tokyo, Japan), previously validated [12] against a mercury sphygmomanometer according to the revised protocol of the British Hypertension Society [13], and appropriate cuff sizes according to each individual’s arm circumference. Patients received appropriate training to measure home BP after a 5-min rest, keeping their legs uncrossed, their back supported, and not talking. They registered duplicate sitting BP readings (1 min apart) in the non-dominant arm, during fixed hours in the morning (8–12 a.m.), afternoon (14–18 p.m.) and evening (20–24 p.m.), for four days. The reliability and reproducibility of this protocol of measurements has previously been addressed [14]. Briefly, in the cited study we assessed the reproducibility and reliability of a 4-day HBPM protocol with and without first-day measurements, analyzing a cohort of 353 subjects who required an HBPM for diagnostic purposes or evaluation of treatment efficacy. Reproducibility was quantified by test-re-test correlations and standard deviation of differences (SDD) between BP measurements obtained during the entire 4 days, with and without exclusion of the first day. The reliability criterion was the stabilization of the mean and standard deviation (SD). On the one hand, we found a strong test-re-test correlation between days 1 and 4 (0.80–0.91), which improved when we excluded the first day (p < 0.001). On the other, we found a reduction of the mean BP when we increased the number of days and a reduction of standard deviation of differences when we excluded day 1.
In the present study, morning readings were taken before breakfast and drug intake. The average of BP readings stored in the devices’ memory (not self–reported measurements) was used for analysis. According to current recommendations, first-day measurements were discarded [15, 16].
For the analysis, we considered a 4-day average of systolic and diastolic home BP, the average discarding first day measurements, and at each measurement period (morning, afternoon, and evening) separately. We also categorized home BP into adequate control when the average was <135/85 mmHg, and inadequate control if systolic BP was ≥135 and/or diastolic BP was ≥85 mmHg, for each of the five scenarios.
Outcomes
Our primary outcome was a composite of fatal and non-fatal cardiovascular events, including cardiovascular death, myocardial infarction, unstable angina, surgical and percutaneous coronary revascularization, congestive heart failure, atrial fibrillation, stroke (ischemic, hemorrhagic, or undetermined) and transient ischemic attack, occurring during follow-up. We also analyzed total mortality, cardiovascular mortality, and non-fatal cardiac and cerebrovascular events as secondary outcomes. Data regarding outcomes were obtained through the exhaustive manual review of each electronic health record, in all its modules: Ambulatory, Hospitalization, Emergency Room, and Home Hospitalization. The World Health Organization International Classification of Diseases (ICD-10), Volume 1, was used to codify the causes of death. Since patients who perform an HBPM in our hospital are affiliated to a prepaid medicine plan, they constitute a “captive” population, receiving healthcare only at the institution. This allows access to all follow-up data (without loss), except in the rare occasions when the prepaid plan cancellation occurs.
In all outcome analyses, we only considered the first event per participant within each category.
Other variables included
Medical records of all patients were reviewed to extract data regarding office BP level prior to HBPM, the type of antihypertensive drugs used at baseline, the presence of risk factors (diabetes, smoking status), and the history of cardiovascular disease (coronary heart disease and cerebrovascular disease). Laboratory data from 6 months prior to HBPM were also collected from medical records.
Regarding office BP, one to three measurements were taken after at least 5-min sitting rest using a standard validated aneroid sphygmomanometer (Riester®, Jungingen, Germany or Wellch-Allyn®, Amsterdam, The Netherlands) or a validated automated upper arm-cuff devices (Omron® HEM-705CP-II or Omron® 7 200, Omron®,Tokyo, Japan) and appropriate cuff sizes according to each individual’s arm circumference. The average BP of available readings was used in the analysis.
Statistical considerations
Sample size calculation
The sample size was estimated assuming an annual cardiovascular event rate of 2.5%. This figure was extracted from other cohorts that also evaluated hypertensive patients under treatment [9, 10]. For a mean follow-up of 6 years in our cohort, we expected to have 15 events per each 100 included subjects. According to Peduzzi et al., in order to ensure the accuracy and precision of estimated coefficients though Cox regression models, the number of events for each included independent variable must be at least 10 [17]. Given that we planned to include 13 co-variables, plus our main variable of interest -home BP- we needed to observe at least 140 events (14*10). Therefore, we had to include at least 934 patients (100*140/15).
Statistical analysis
Quantitative data are expressed as mean and standard deviation or median and interquartile range, according to data distribution. Qualitative data are expressed as absolute and relative frequency.
The prognostic value of home BP in terms of cardiovascular events was analyzed through Cox regression models (proportional hazards analysis), which accommodate censored data, estimating unadjusted and adjusted hazard ratios along with their 95% confidence interval. In the adjusted models, hazard ratios were adjusted for office systolic and diastolic BP, sex, age, body mass index, number of antihypertensive drugs, smoking habits, diabetes, history of cardiac and cerebrovascular disease, fasting plasma glucose, total cholesterol and creatinine level. Home BP was analyzed as a continuous and as a dichotomous variable (uncontrolled vs. controlled BP). We used the Akaike information criteria (AIC) to compare different modeling strategies. AIC are model selection criteria, i.e., statistical tools that help identify the best-fitted candidate model among a set of candidates. The best model is the one that obtains the lowest score, which measures how much the evaluated model deviates from a theoretical model that shows a perfect fit. To compare models, the AIC of each model is calculated. If a model is more than 2 AIC units lower than another, then it is considered significantly better than that model [18].
All hypothesis tests were two-tailed, and a p value <0.05 was considered statistically significant.
Results
Between September 2008 and December 2015, a total of 2732 HBPMs were performed. After discarding untreated subjects, duplicate HBPMs and those with <16 readings, 1582 patients remained for the analysis (Fig. 1). Baseline patient characteristics and antihypertensive treatment profile are depicted in Table 1. BP profile is depicted in Table 2. Briefly, 33.4% of participants were men, median age was 70.8 years, 11.4% had diabetes and 14.3% had a history of ischemic cardiopathy or cerebrovascular disease. Patients were treated with an average of 2.1 antihypertensive drugs, and had a mean office and home BP of 137.6/77.8 and 132.9/73.6 mmHg, respectively.
Follow-up ended on April, 30 2 020, with a median of 5.9 years (IQR 4.9–8.7), during which 164 deaths (37 of cardiovascular cause) were registered. On that date, vital status was known for 81.2% of the sample. Our primary outcome (composite of fatal and non-fatal cardiovascular events) was observed in 273 patients. Table 3 describes in detail the cardiac and cerebrovascular events that occurred.
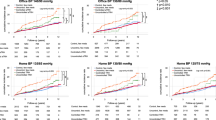
For our primary outcome (fatal and non-fatal cardiovascular events), we found a significant higher risk for uncontrolled vs. controlled home BP. This was true for the five scenarios, i.e., considering 4-day BP average, discarding first day measurements and analyzing morning, afternoon and evening separately. Figures 2 and 3 depict Nelson–Aalen cumulative hazard estimates for the primary outcome along these scenarios.
Table 4 shows the hazard ratios and their 95% CI for the unadjusted and adjusted models. Home BP was significantly associated with cardiovascular events in the unadjusted models for 4-day average home BP, discarding first-day measurements and for morning, afternoon, and evening home BP. Regarding the adjusted models, 4-day average and the average discarding first-day measurements were only marginally significant for systolic BP. In a sensitivity analysis excluding patients with previous cardiovascular disease, our results remained unchanged (Supplementary Table 1). Similar results were also obtained when analyzing major adverse cardiovascular events (cardiovascular mortality, myocardial infarction or stroke) as the outcome, and when adjusting for office systolic and office diastolic BP in separate models (Supplementary Tables 2 and 3). Of note, the association between home BP and cardiovascular events remained statistically significant in the adjusted models when analyzing morning, afternoon, and evening periods separately. When comparing models for these three periods of measurement through the AIC, the model with the lower score, i.e., the best predictor among the three models, was the one that included afternoon home BP readings: 3472 for afternoon home BP vs. 3622 for morning home BP vs. 3623 for evening home BP.
Multicollinearity between office and home BP was tested through a correlation matrix of the coefficients in the Cox models. The cut-off value used to consider the presence of multicollinearity through the correlation coefficient was 0.5, that is, absolute values of the coefficient greater than 0.5 were considered positive for the presence of multicollinearity. In these analyses, we found that, in all cases, the correlation coefficients were <0.5, which supports the absence of multicollinearity, and allows us to introduce both variables in the same model.
Considering our secondary outcomes, home BP was significantly associated with total mortality and cardiovascular mortality in the adjusted models, considering 4-day measurements, discarding first-day measurements, and analyzing morning, afternoon, and evening separately. Regarding non-fatal cardio and cerebrovascular events, no significant associations were found in any of the adjusted model scenarios (Table 5).
Discussion
In our study, we found that increased baseline home BP is associated with an increased risk of fatal and non-fatal cardiovascular and cerebrovascular events in patients with hypertension under treatment. This association is independent from office BP and other vascular risk factors and is observed in all measurement periods (morning, afternoon, and evening). The association with an increased risk of events would appear to occur primarily at the expense of fatal events.
There are several reasons that might explain why home BP is a better predictor of cardiovascular events than office BP: on the one hand, HBPM allows a significantly higher number of BP measurements than the one to three measurements that are usually performed in the office, making the former more reproducible [15, 16]. On the other, given that office BP is frequently assessed through the auscultatory method, it is subject to observer bias, manifested, for example, in rounding up the last digit of the reading preferably to 0 or 5. This is not an issue in HBPM, where the oscillometric method is used. Office BP readings are also particularly more susceptible to the alerting reaction, a frequent phenomenon, where the first reading is higher than the subsequent ones [19]. Finally, home BP measurements tend to drop 20% less with treatment than office BP measurements, allowing a more accurate warning of the presence of sub-optimal treatment [20].
When considering studies that evaluated hypertensive patients under treatment, our study is similar to the SHEAF study, conducted in older treated hypertensive patients in France [9]. The SHEAF was designed for the primary outcome “cardiovascular mortality”, for which the authors did not find a significant association, although the follow-up period was 3.2 years vs. 5.9 years in our study. For their secondary outcome “fatal and non-fatal cardiovascular events”, there was a significant association with home BP, but the model did not include office BP as an adjustment variable. Other relevant data come from the International Database of HOme blood pressure in relation to Cardiovascular Outcome (IDHOCO) [10], where 22.4% of the subjects were hypertensive patients under treatment. In this subgroup, an association between baseline home BP and cardiovascular events was found. Of note, no adjustment for office BP was made in the analysis. We therefore consider that our finding that home BP has added value to predict cardiovascular events beyond office BP and other factors in this particular population, is an original contribution.
An important issue in patients that are already under treatment is the moment of the day when home BP measurements are taken, given the influence that medication could have in the different periods evaluated. Few studies, mainly from Asian origin, have evaluated different periods during HBPM separately. In the J-HOP study, for example, patients with uncontrolled morning home BP had a higher risk of stroke in comparison with those with controlled morning BP [21]. Of note, the predictive ability of morning BP was attenuated when combining these measurements with evening BP ones. Other studies found similar results [22]. As a consequence, a recent consensus highlighted the importance of the moment at which home BP is measured in patients under treatment and stated that isolated morning hypertension could be a marker of an inadequate antihypertensive regimen, urging to screen patients for this situation [23]. In accordance with these results, we found that combining all the periods in a single average might not be an appropriate strategy (only marginally significance was reached regarding the adjusted models), perhaps being better to inform BP average for each period separately. In fact, the latter case maintained statistical significance for cardiovascular risk prediction. Interestingly, the measurement period found to be the best predictor was the afternoon. In a study conducted by Almeida et al., a measurement protocol that included afternoon readings had a higher association with prognostic biomarkers, such as microalbuminuria and left ventricular hypertrophy, than a protocol that only included morning and evening measurements [24]. Of note, we decided to use Akaike information criteria, a well-known estimator of relative quality of statistical models for a given set of data, to compare models that considered BP measurements at different times of the day. These findings might have been different had other comparison strategies been used.
Another finding of our research is that, when analyzing fatal and non-fatal events separately, HBPM constitutes a significant independent predictor of fatal events whereas statistical significance is lost for non-fatal events. Studies evaluating hypertensive patients under treatment have shown heterogeneous results on this subject: while the SHEAF study, for example, failed to find an association between HBPM and cardiovascular death [9], in the IDHOCO database, HBPM was an independent predictor of this event in the subgroup of medicated patients [10], although, once again, we emphasize that no adjustment was made for office BP in the models. Consequently, given that our study was designed based on the primary endpoint, the results emanating from the secondary endpoints, such as an eventual higher prognostic value of HBPM for fatal events, are currently simple hypothesis generators.
When comparing HBPM with the other available technique for out-of-office BP assessment, i.e., ABPM, it is important to consider that the former is better tolerated by patients, more widely available and less expensive than ABPM, while it provides similar information for the usual clinical scenarios of everyday practice [25, 26]. Moreover, HBPM is currently the preferred method for long-term follow-up of patients that are already under treatment [27, 28]. This underscores the relevance of having found an independent predictive value of HBPM in this subgroup of patients.
Our study has some limitations that must be taken into consideration. First, this research was conducted in a single center, a community hospital in the city of Buenos Aires, representative of Argentine middle-class patients, mainly from European descent. As a consequence, our results may not be generalizable to other populations. Second, only about 20% of the patients in our study had their BP measured twice or thrice in the office: most subjects had one office BP reading only. Although this is in line with common clinical practice, it reduces the reproducibility of office BP, increasing its disadvantage compared to HBPM. Third, the time at which the patients took their antihypertensive medication was not controlled. This could have led to differences in BP in the different moments of the day considered. Additionally, Cox models, usually employed in this kind of analysis in all similar research, evaluate a basal measurement (in this case, home BP with the antihypertensive medication taken at that moment) and then estimate what occurs during follow-up, regarding events. As a result, possible changes in antihypertensive medication during follow-up are not taken into account in the analysis. Moreover, drug adherence was not formally tested in the present study. Fourth, LDL-cholesterol level is a more reliable predictor of cardiovascular events than the total cholesterol level used in our study. Finally, although the main advantage of using composites is increased statistical efficiency, this approach -used in our study- might also open the door to misdirection, especially when there is heterogeneity of response among components of composite outcomes. In some situations, the overall positive effect may be related to the less clinically relevant component(s) of the composite measure, leading to inadequate conclusions. In addition, the choice to combine of different types of events in one composite endpoint could also lead to different results. In this study, we followed the analytical strategies from previous similar studies against which we pretended to make comparisons.
On the other hand, our study also has some strengths: all patients used a validated oscillometric device (same brand and model) and followed the same HBPM protocol, the cuff was adapted to each patient´s arm circumference, and the readings stored in the devices’ memory were used for analysis, avoiding a possible reporting bias [29]. Regarding the recording of events, our hospital has a long history in the use of patient-centered electronic medical records, being the first Argentine hospital certified as 100% computerized by the Healthcare Information and Management Systems Society (HIMSS). Therefore, the use of Systematized nomenclature of medicine clinical terms (SNOMED CT) enables the coding of all medical concepts and allows the multiple classifications to be related. This improves the quality of the registry, by storing both controlled codes and narrative text in the clinical data repository, resulting in a high-quality registry of the events in the present study.
In conclusion, home BP is a predictor of cardiovascular events in hypertensive patients under treatment, independent from office BP and other vascular risk factors. Such association is observed in all measurement periods (morning, afternoon, and evening) and would seem to occur primarily at the expense of fatal events.
Summary
What is known about the topic
-
Home blood pressure monitoring is recommended for out-of-office blood pressure assessment, especially in patients under treatment.
-
It has prognostic value in the general population.
-
Evidence in medicated hypertensive patients is controversial.
What this study adds
-
Home blood pressure monitoring was an independent predictor of cardiovascular events in hypertensives under treatment.
-
This held true for all measurement periods: morning, afternoon, and evening.
Data availability
Additional data are available from the corresponding author on reasonable request.
Code availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, et al. 2020 International Society of Hypertension global hypertension practice guidelines. J Hypertens. 2020;38:982–1004.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 Practice Guidelines for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. Blood Press. 2018;27:314–40.
Robbins CL, Ford ND, Hayes DK, Ko JY, Kuklina E, Cox S, et al. Clinical practice changes in monitoring hypertension early in the COVID-19 pandemic. Am J Hypertens. 2022:hpac049. https://doi.org/10.1093/ajh/hpac049.
Niiranen TJ, Hänninen MR, Johansson J, Reunanen A, Jula AM. Home-measured blood pressure is a stronger predictor of cardiovascular risk than office blood pressure: the Finn-Home study. Hypertension. 2010;55:1346–51.
Imai Y, Ohkubo T, Sakuma M, Tsuji II, Satoh H, Nagai K, et al. Predictive power of screening blood pressure, ambulatory blood pressure and blood pressure measured at home for overall and cardiovascular mortality: a prospective observation in a cohort from Ohasama, northern Japan. Blood Press Monit. 1996;1:251–4.
Sega R, Facchetti R, Bombelli M, Cesana G, Corrao G, Grassi G, et al. Prognostic value of ambulatory and home blood pressures compared with office blood pressure in the general population: follow-up results from the Pressioni Arteriose Monitorate e Loro Associazioni (PAMELA) study. Circulation. 2005;111:1777–83.
Shimada K, Fujita T, Ito S, Naritomi H, Ogihara T, Shimamoto K, et al. The importance of home blood pressure measurement for preventing stroke and cardiovascular disease in hypertensive patients: a sub-analysis of the Japan Hypertension Evaluation with Angiotensin II Antagonist Losartan Therapy (J-HEALTH) study, a prospective nationwide observational study. Hypertens Res. 2008;31:1903–11.
Kario K, Saito I, Kushiro T, Teramukai S, Ishikawa Y, Mori Y, et al. Home blood pressure and cardiovascular outcomes in patients during antihypertensive therapy: primary results of HONEST, a large-scale prospective, real-world observational study. Hypertension. 2014;64:989–96.
Bobrie G, Chatellier G, Genes N, Clerson P, Vaur L, Vaisse B, et al. Cardiovascular prognosis of “masked hypertension” detected by blood pressure self-measurement in elderly treated hypertensive patients. JAMA. 2004;291:1342–9.
Niiranen TJ, Asayama K, Thijs L, Johansson JK, Ohkubo T, Kikuya M, et al. International Database of Home blood pressure in relation to Cardiovascular Outcome Investigators. Outcome-driven thresholds for home blood pressure measurement: international database of home blood pressure in relation to cardiovascular outcome. Hypertension. 2013;61:27–34.
Delucchi A, Marín M, Páez O, Bendersky M, Rodríguez P. en representación de los participantes designados por la Sociedad Argentina de Cardiología, Federación Argentina de Cardiología y Sociedad Argentina de Hipertensión Arterial. Principales conclusiones del Consenso Argentino de Hipertensión Arterial [Principal conclusions of the Argentine Consensus on Arterial Hypertension]. Hipertens Riesgo Vasc. 2019;36:96–109. Spanish
Artigao LM, Llavador JJ, Puras A, López Abril J, Rubio MM, Torres C, et al. Evaluación y validación de los monitores Omron Hem 705 CP y Hem 706/711 para automedidas de presión arterial [Evaluation and validation of Omron Hem 705 CP and Hem 706/711 monitors for self-measurement of blood pressure]. Aten Primaria. 2000;25:96–102. Spanish
O’Brien E, Mee F, Atkins N, Thomas M. Evaluation of three devices for self-measurement of blood pressure according to the revised British Hypertension Society Protocol: the Omron HEM-705CP, Philips HP5332, and Nissei DS-175. Blood Press Monit. 1996;1:55–61.
Barochiner J, Cuffaro PE, Aparicio LS, Elizondo CM, Giunta DH, Rada MA, et al. Reproducibilidad y confiabilidad de un protocolo de 4 días de monitoreo domiciliario de presión arterial con y sin exclusión del primer día [Reproducibility and reliability of a 4-day HBPM protocol with and without first day measurements]. Rev Fac Cien Med Univ Nac Cordoba. 2011;68:149–53.
Lin HJ, Wang TD, Yu-Chih Chen M, Hsu CY, Wang KL, Huang CC, et al. 2020 consensus statement of the Taiwan Hypertension Society and the Taiwan Society of Cardiology on home blood pressure monitoring for the management of arterial hypertension. Acta Cardiol Sin. 2020;36:537–61.
Villar R, Sánchez RA, Boggia J, Peñaherrera E, Lopez J, Barroso WS, et al. Recommendations for home blood pressure monitoring in Latin American countries: a Latin American Society of Hypertension position paper. J Clin Hypertens. 2020;22:544–54.
Peduzzi P, Concato J, Feinstein AR, Holford TR. Importance of events per independent variable in proportional hazards regression analysis. II. Accuracy and precision of regression estimates. J Clin Epidemiol. 1995;48:1503–10.
Kamikubo K, Murase H, Murayama M, Miura K. Microcomputer-based nonlinear regression analysis of ligand-binding data: application of Akaike’s information criterion. Jpn J Pharmacol. 1986;40:342–6.
Barochiner J, Aparicio LS, Alfie J, Cuffaro PE, Marin MJ, Morales MS, et al. Alerting reaction in office blood pressure and target organ damage: an innocent phenomenon? Curr Hypertens Rev. 2017;13:104–8.
Ishikawa J, Carroll DJ, Kuruvilla S, Schwartz JE, Pickering TG. Changes in home versus clinic blood pressure with antihypertensive treatments: a meta-analysis. Hypertension. 2008;52:856–64.
Hoshide S, Yano Y, Haimoto H, Yamagiwa K, Uchiba K, Nagasaka S, et al. J-HOP Study Group. Morning and evening home blood pressure and risks of incident stroke and coronary artery disease in the Japanese general practice population: the Japan Morning Surge-Home Blood Pressure Study. Hypertension. 2016;68:54–61.
Tamaki S, Nakamura Y, Yoshino T, Matsumoto Y, Tarutani Y, Okabayashi T, et al. The association between morning hypertension and metabolic syndrome in hypertensive patients. Hypertens Res. 2006;29:783–8.
Wang JG, Kario K, Chen CH, Park JB, Hoshide S, Huo Y, et al. Management of morning hypertension: a consensus statement of an Asian expert panel. J Clin Hypertens. 2018;20:39–44.
Almeida AE, Stein R, Gus M, Nascimento JA, Belli KC, Arévalo JR, et al. Relevance to home blood pressure monitoring protocol of blood pressure measurements taken before first- morning micturition and in the afternoon. Arq Bras Cardiol. 2014;103:338–47.
Muntner P, Shimbo D, Carey RM, Charleston JB, Gaillard T, Misra S, et al. Measurement of blood pressure in humans: a scientific statement from the American Heart Association. Hypertension 2019;73:e35–e66.
Peixoto AJ. Practical aspects of home and ambulatory blood pressure monitoring. Methodist Debakey Cardiovasc J. 2015;11:214–8.
Liyanage-Don N, Fung D, Phillips E, Kronish IM. Implementing home blood pressure monitoring into clinical practice. Curr Hypertens Rep. 2019;21:14.
Stergiou GS, Kario K, Kollias A, McManus RJ, Ohkubo T, Parati G, et al. Home blood pressure monitoring in the 21st century. J Clin Hypertens. 2018;20:1116–21.
Schwartz CL, Seyed-Safi A, Haque S, Bray EP, Greenfield S, Hobbs FDR, et al. Do patients actually do what we ask: patient fidelity and persistence to the Targets and Self-Management for the Control of Blood Pressure in Stroke and at Risk Groups blood pressure self-management intervention. J Hypertens. 2018;36:1753–61.
Acknowledgements
We are grateful to Ms. Erika Barochiner for language editing.
Funding
This study was partially funded by a grant from Asociación Mutual de Profesionales del Hospital Italiano (AMPHI).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and data collection were performed by JBa, LA, and RM. Analysis of data was performed by JBa and JBo. The first draft of the manuscript was written by JBa and all authors commented on subsequent versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The study protocol was approved by the local ethics committee (Comité de Ética de Protocolos de Investigación [CEPI], approval #3319).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Barochiner, J., Aparicio, L.S., Martínez, R. et al. Prognostic value of home blood pressure monitoring in patients under antihypertensive treatment. J Hum Hypertens 37, 775–782 (2023). https://doi.org/10.1038/s41371-022-00758-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-022-00758-x