Abstract
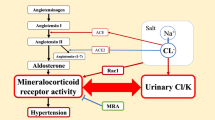
Mineralocorticoid receptor antagonists are frequently used for the treatment of primary aldosteronism. Steroidal mineralocorticoid receptor antagonists may have antagonistic actions on androgen receptors, agonistic actions on progesterone receptors, and antagonistic actions on mineralocorticoid receptors. Because anti-androgen effects may cause body fat accumulation and skeletal muscle atrophy, there are concerns that this drug may have adverse effects on body composition. Therefore, in this randomized prospective study, we compared the adverse effects of spironolactone, a steroidal mineralocorticoid receptor antagonist, and esaxerenone, a nonsteroidal mineralocorticoid receptor antagonist, on sex hormone levels and body composition in patients with primary aldosteronism without severe renal dysfunction. The serum concentration of free testosterone was significantly higher in the spironolactone group than in the esaxerenone group in both males and females. However, the levels of estradiol, progesterone, luteinizing hormone, and follicle stimulating hormone did not significantly increase. Changes in body fat percentage and muscle mass rate were not significantly different between the two groups. No patient showed a serum potassium level ≥6.0 mEq/L; however, serum potassium levels were significantly higher in the spironolactone group than in the esaxerenone group. These data indicate that spironolactone may have antagonistic effects on androgen receptors. Esaxerenone did not show any apparent adverse effects, suggesting that it can be safely used in patients with primary aldosteronism.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Käyser SC, Dekkers T, Groenewoud HJ, van der Wilt GJ, Carel Bakx J, van der Wel MC, et al. Study heterogeneity and estimation of prevalence of primary aldosteronism: a systematic review and meta-regression analysis. J Clin Endocrinol Metab. 2016;101:2826–35. https://doi.org/10.1210/jc.2016-1472
Rossi GP, Bernini G, Desideri G, Fabris B, Ferri C, Giacchetti G, et al. Renal damage in primary aldosteronism. Hypertension. 2006;48:232–8. https://doi.org/10.1161/01.HYP.0000230444.01215.6a
Pitt B, Zannad F, Remme WJ, Cody R, Castaigne A, Perez A, et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Surv Anesthesiol. 2000;44:182 https://doi.org/10.1097/00132586-200006000-00059
Samuel JL, Delcayre C. Heart failure: Aldosterone antagonists are underused by clinicians. Nat Rev Cardiol 2010;7:125–7.
Weinberger MH, Roniker B, Krause SL, Weiss RJ. Eplerenone, a selective aldosterone blocker, in mild-to-moderate hypertension. Am J Hypertens. 2002;15:709–16. https://doi.org/10.1016/S0895-7061(02)02957-6
Wan N, Rahman A. Nishiyama A. Esaxerenone, a novel nonsteroidal mineralocorticoid receptor blocker (MRB) in hypertension and chronic kidney disease. J Hum Hypertens. 2021;35:148–56. https://doi.org/10.1038/s41371-020-0377-6
Arai K, Homma T, Morikawa Y, Ubukata N, Tsuruoka H, Aoki K, et al. Pharmacological profile of CS-3150, a novel, highly potent and selective non-steroidal mineralocorticoid receptor antagonist. Eur J Pharm. 2015;761:226–34. https://doi.org/10.1016/j.ejphar.2015.06.015
Itoh H, Ito S, Rakugi H, Okuda Y, Nishioka S. Efficacy and safety of dosage-escalation of low-dosage esaxerenone added to a RAS inhibitor in hypertensive patients with type 2 diabetes and albuminuria: a single-arm, open-label study. Hypertens Res. 2019;42:1572–81. https://doi.org/10.1038/s41440-019-0270-2
Arai K, Morikawa Y, Ubukata N, Sugimoto K. Synergistic reduction in albuminuria in type 2 diabetic mice by esaxerenone (CS-3150), a novel nonsteroidal selective mineralocorticoid receptor blocker, combined with an angiotensin II receptor blocker. Hypertens Res. 2020;43:1204–13. https://doi.org/10.1038/s41440-020-0495-0
Satoh F, Ito S, Itoh H, Rakugi H, Shibata H, Ichihara A, et al. Efficacy and safety of esaxerenone (CS-3150), a newly available nonsteroidal mineralocorticoid receptor blocker, in hypertensive patients with primary aldosteronism. Hypertens Res. 2021;44:464–72. https://doi.org/10.1038/s41440-020-00570-5
Ito S, Itoh H, Rakugi H, Okuda Y, Iijima S. Antihypertensive effects and safety of esaxerenone in patients with moderate kidney dysfunction. Hypertens Res. 2021;44:489–97. https://doi.org/10.1038/s41440-020-00585-y
Takahashi M, Ubukata O, Homma T, Asoh Y, Honzumi M, Hayashi N, et al. Crystal structure of the mineralocorticoid receptor ligand‐binding domain in complex with a potent and selective nonsteroidal blocker, esaxerenone (CS‐3150). FEBS Lett. 2020;594:1615–23. https://doi.org/10.1002/1873-3468.13746
Ferrando AA, Sheffield-Moore M, Yeckel CW, Gilkison C, Jiang J, Achacosa A, et al. Testosterone administration to older men improves muscle function: molecular and physiological mechanisms. Am J Physiol Metab. 2002;282:E601–E607. https://doi.org/10.1152/ajpendo.00362.2001
Ferrando AA, Sheffield-Moore M, Paddon-Jones D, Wolfe RR, Urban RJ. Differential anabolic effects of testosterone and amino acid feeding in older men. J Clin Endocrinol Metab. 2003;88:358–62. https://doi.org/10.1210/jc.2002-021041
Urban RJ, Bodenburg YH, Gilkison C, Foxworth J, Coggan AR, Wolfe RR, et al. Testosterone administration to elderly men increases skeletal muscle strength and protein synthesis. Am J Physiol Metab. 1995;269:E820–E826. https://doi.org/10.1152/ajpendo.1995.269.5.E820
The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2014). Hypertens Res 2014;37:253–53. https://doi.org/10.1038/hr.2014.20
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–92. https://doi.org/10.1053/j.ajkd.2008.12.034
Roush GC, Ernst ME, Kostis JB, Yeasmin S, Sica DA. Dose doubling, relative potency, and dose equivalence of potassium-sparing diuretics affecting blood pressure and serum potassium: systematic review and meta-analyses. J Hypertens. 2016;34:11–9. https://doi.org/10.1097/HJH.0000000000000762
Palmer BF, Clegg DJ. Diagnosis and treatment of hyperkalemia. Cleve Clin J Med. 2017;84:934–42. https://doi.org/10.3949/ccjm.84a.17056
Sato A, Fukuda S. Effect of aldosterone breakthrough on albuminuria during treatment with a direct renin inhibitor and combined effect with a mineralocorticoid receptor antagonist. Hypertens Res. 2013;36:879–84. https://doi.org/10.1038/hr.2013.74
de Gasparo M, Joss U, Ramjoué HP, Whitebread SE, Haenni H, Schenkel L, et al. Three new epoxy-spirolactone derivatives: characterization in vivo and in vitro. J Pharm Exp Ther. 1987;240:650–6. http://www.ncbi.nlm.nih.gov/pubmed/2949071
Bachelot A, Chabbert-Buffet N, Salenave S, Kerlan V, Galand-Portier M-B. Anti-androgen treatments. Ann Endocrinol (Paris). 2010;71:19–24. https://doi.org/10.1016/j.ando.2009.12.001
Ito S, Itoh H, Rakugi H, Okuda Y, Yamakawa S. Efficacy and safety of esaxerenone (CS-3150) for the treatment of essential hypertension: a phase 2 randomized, placebo-controlled, double-blind study. J Hum Hypertens. 2019;33:542–51. https://doi.org/10.1038/s41371-019-0207-x
Layton AM, Eady EA, Whitehouse H, Del Rosso JQ, Fedorowicz Z, van Zuuren EJ. Oral spironolactone for acne vulgaris in adult females: a hybrid systematic review. Am J Clin Dermatol. 2017;18:169–91. https://doi.org/10.1007/s40257-016-0245-x
Feraco A, Marzolla V, Scuteri A, Armani A, Caprio M. Mineralocorticoid receptors in metabolic syndrome: from physiology to disease. Trends Endocrinol Metab. 2020;31:205–17. https://doi.org/10.1016/j.tem.2019.11.006
Brown NJ. Aldosterone and vascular inflammation. Hypertension. 2008;51:161–7. https://doi.org/10.1161/HYPERTENSIONAHA.107.095489
Funder JW. Aldosterone, mineralocorticoid receptors and vascular inflammation. Mol Cell Endocrinol. 2004;217:263–9. https://doi.org/10.1016/j.mce.2003.10.054
Turchin A, Guo CZ, Adler GK, Ricchiuti V, Kohane IS, Williams GH. Effect of acute aldosterone administration on gene expression profile in the heart. Endocrinology. 2006;147:3183–9. https://doi.org/10.1210/en.2005-1674
Guo C, Ricchiuti V, Lian BQ, Yao TM, Coutinho P, Romero JR, et al. Mineralocorticoid receptor blockade reverses obesity-related changes in expression of adiponectin, peroxisome proliferator-activated receptor-γ, and proinflammatory adipokines. Circulation. 2008;117:2253–61. https://doi.org/10.1161/CIRCULATIONAHA.107.748640
Hirata A, Maeda N, Hiuge A, Hibuse T, Fujita K, Okada T, et al. Blockade of mineralocorticoid receptor reverses adipocyte dysfunction and insulin resistance in obese mice. Cardiovasc Res. 2009;84:164–72. https://doi.org/10.1093/cvr/cvp191
Schäfer N, Lohmann C, Winnik S, van Tits LJ, Miranda MX, Vergopoulos A, et al. Endothelial mineralocorticoid receptor activation mediates endothelial dysfunction in diet-induced obesity. Eur Heart J. 2013;34:3515–24. https://doi.org/10.1093/eurheartj/eht095
Caprio M, Fève B, Claës A, Viengchareun S, Lombès M, Zennaro M-C. Pivotal role of the mineralocorticoid receptor in corticosteroid‐induced adipogenesis. FASEB J. 2007;21:2185–94. https://doi.org/10.1096/fj.06-7970com
Travison TG, Basaria S, Storer TW, Jette AM, Miciek R, Farwell WR, et al. Clinical meaningfulness of the changes in muscle performance and physical function associated with testosterone administration in older men with mobility limitation. J Gerontol Ser A Biol Sci Med Sci. 2011;66A:1090–9. https://doi.org/10.1093/gerona/glr100
Acknowledgements
We would like to thank the ward staff and physicians who took good care of the patients enrolled in this study.
Author information
Authors and Affiliations
Contributions
The study was designed by TI and AI. Data analysis and interpretation were conducted by TI and SM. The manuscript was written by TS and SM and was approved by AI.
Corresponding author
Ethics declarations
Conflict of interest
SM and AI received honorarium as a lecture fee from Daiichi Sankyo Company Limited.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ishikawa, T., Morimoto, S. & Ichihara, A. Effects of mineralocorticoid receptor antagonists on sex hormones and body composition in patients with primary aldosteronism. Hypertens Res 45, 496–506 (2022). https://doi.org/10.1038/s41440-021-00836-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-021-00836-6