Abstract
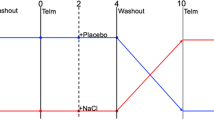
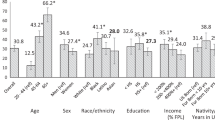
Advanced glycation end product (AGE) clearance may cause renal tubular injuries, such as changes in sodium reabsorption. We hypothesize that AGEs interact with sodium metabolism to influence blood pressure (BP). The study participants were outpatients who were suspected of having hypertension but had not been treated with antihypertensive medication. Clinic and ambulatory blood pressures were measured at baseline (n = 989) and during follow-up (median, 4.4 years, n = 293). Plasma AGE concentrations were measured by enzyme-linked immunosorbent assay. Twenty-four-hour urine was collected for measurements of creatinine, sodium and lithium. In a cross-sectional analysis (n = 989), subjects in the top quintile versus quintiles 1–4 of plasma AGE concentration had significantly (P ≤ 0.004) lower fractional excretion of lithium (18.3% vs. 21.6%) and fractional distal reabsorption rate of sodium (95.0% vs. 95.8%) but similar BP (P ≥ 0.25). However, there was an interaction between plasma AGE concentration and urinary sodium excretion in relation to diastolic BP (P ≤ 0.058). Only in participants with low urinary sodium chloride excretion (≤6 grams/day, n = 189), clinic (84.3 vs. 80.2 mmHg), 24-h (83.9 vs. 80.4 mmHg), daytime (87.8 vs. 84.8 mmHg) and nighttime (75.1 vs. 72.1 mmHg) diastolic BP at baseline were higher (P ≤ 0.05) in the top quintile than in quintiles 1–4 of plasma AGE concentration. In the longitudinal study (n = 383), similar trends were observed, with significant (P ≤ 0.05) differences in the increment in daytime diastolic BP (6.8 vs. −1.7 mmHg) and incidence of ambulatory and treated hypertension (hazard ratio 3.73) during follow-up. In conclusion, AGEs were associated with high BP, probably via enhanced proximal sodium handling and on low dietary sodium intake.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Basta G, Schmidt AM, De Caterina R. Advanced glycation end products and vascular inflammation: implications for accelerated atherosclerosis in diabetes. Cardiovasc Res. 2004;63:582–92.
Goh SY, Cooper ME. Clinical review: the role of advanced glycation end products in progression and complications of diabetes. J Clin Endocrinol Metab. 2008;93:1143–52.
Huang QF, Sheng CS, Liu M, Li FH, Li Y, Wang JG. Arterial stiffness and wave reflections in relation to plasma advanced glycation end products in a Chinese population. Am J Hypertens. 2013;26:754–61.
Huang QF, Sheng CS, Kang YY, Zhang L, Wang S, Li FK, et al. Central and peripheral blood pressures in relation to plasma advanced glycation end products in a Chinese population. J Hum Hypertens. 2016;30:430–5.
Hwang JY, Kan WC, Liu YB, Chuang LY, Guh JY, Yang YL, et al. Angiotensin-converting enzyme inhibitors attenuated advanced glycation end products-induced renal tubular hypertrophy via enhancing nitric oxide signaling. J Cell Physiol. 2019;234:17473–81.
Li J, Qu X, Yao J, Caruana G, Ricardo SD, Yamamoto Y, et al. Blockade of endothelial-mesenchymal transition by a smad3 inhibitor delays the early development of streptozotocin-induced diabetic nephropathy. Diabetes. 2010;59:2612–24.
Yuan Y, Sun H, Sun Z. Advanced glycation end products (AGEs) increase renal lipid accumulation: a pathogenic factor of diabetic nephropathy (DN). Lipids Health Dis. 2017;16:126.
Garagliano JM, Katsurada A, Miyata K, Derbenev AV, Zsombok A, Navar LG, et al. Advanced glycation end products stimulate angiotensinogen production in renal proximal tubular cells. Am J Med Sci. 2019;357:57–66.
Chang CT, Wu MS, Tian YC, Chen KH, Yu CC, Liao CH, et al. Enhancement of epithelial sodium channel expression in renal cortical collecting duct cells by advanced glycation end products. Nephrol Dial Transpl. 2007;22:722–31.
Bohlender JM, Franke S, Stein G, Wolf G. Advanced glycation end products and the kidney. Am J Physiol Ren Physiol. 2005;289:F645–F659.
He FJ, MacGregor GA. A comprehensive review on salt and health and current experience of worldwide salt reduction programmes. J Hum Hypertens. 2009;23:363–84.
Brown IJ, Tzoulaki I, Candeias V, Elliott P. Salt intakes around the world: implications for public health. Int J Epidemiol. 2009;38:791–813.
Forman JP, Scheven L, de Jong PE, Bakker SJ, Curhan GC, Gansevoort RT. Association between sodium intake and change in uric acid, urine albumin excretion, and the risk of developing hypertension. Circulation. 2012;125:3108–16.
Intersalt Cooperative Research Group. Intersalt: an international study of electrolyte excretion and blood pressure. Result for 24 h urinary sodium and potassium excretion. Br Med J. 1988;297:319–28.
Elliott P, Stamler J, Nichols R, Dyer AR, Stamler R, Kesteloot H, et al. Intersalt revisited: further analyses of 24 h sodium excretion and blood pressure within and across populations. Intersalt Cooperative Research Group. Br Med J. 1996;312:1249–53.
Tuomilehto J, Jousilahti P, Rastenyte D, Moltchanov V, Tanskanen A, Pietinen P, et al. Urinary sodium excretion and cardiovascular mortality in Finland: a prospective study. Lancet. 2001;357:848–51.
He J, Ogden LG, Vupputuri S, Bazzano LA, Loria C, Whelton PK. Dietary sodium intake and subsequent risk of cardiovascular disese in overweight adults. J Am Med Ass. 1999;282:2027–34.
Umesawa M, Iso H, Date C, Yamamoto A, Toyoshima H, Watanabe Y, et al. Relations between dietary sodium and potassium intakes and mortality from cardiovascular disease: the Japan Collaborative Cohort Study for Evaluation of Cancer Risks. Am J Clin Nutr. 2008;88:195–202.
Carlstrom M, Sallstrom J, Skott O, Larsson E, Persson AE. Uninephrectomy in young age or chronic salt loading causes salt-sensitive hypertension in adult rats. Hypertension. 2007;49:1342–50.
He FJ, Marciniak M, Markandu ND, Antonios TF, MacGregor GA. Effect of modest salt reduction on skin capillary rarefaction in white, black, and asian individuals with mild hypertension. Hypertension. 2010;56:253–9.
Sheng CS, Cheng YB, Wei FF, Yang WY, Guo QH, Li FK, et al. Diurnal blood pressure rhythmicity in relation to environmental and genetic cues in untreated referred patients. Hypertension. 2017;69:128–35.
Cheng YB, Li LH, Guo QH, Li FK, Huang QF, Sheng CS, et al. Independent effects of blood pressure and parathyroid hormone on aortic pulse wave velocity in untreated Chinese patients. J Hypertens. 2017;35:1841–8.
Guo QH, Cheng YB, Zhang DY, Wang Y, Huang QF, Sheng CS, et al. Comparison between home and ambulatory morning blood pressure and morning hypertension in their reproducibility and associations with vascular injury. Hypertension. 2019;74:137–44.
World Medical Association. Declaration of Helsinki. J Am Med Ass. 2013;227:184–9.
Stevenson PH. Height-weight-surface formula for the estimation of surface area in Chinese subjects. Chin J Physiol. 1937;12:327–30.
Writing Group of 2018 Chinese Guidelines for the Management of Hypertension. 2018 Chinese guidelines for the management of hypertension. Chin J Cardiovasc Med. 2019;24:1–46.
Ma YC, Zuo L, Chen JH, Luo Q, Yu XQ, Li Y, et al. Modified glomerular filtration rate estimating equation for Chinese patients with chronic kidney disease. J Am Soc Nephrol. 2006;17:2937–44.
Sacks DB, Arnold M, Bakris GL, Bruns DE, Horvath AR, Kirkman MS, et al. Guidelines and recommendations for laboratory analysis in the diagnosis and management of diabetes mellitus. Diabet Care. 2011;34:e61–e99.
Zou J, Li Y, Yan CH, Wei FF, Zhang L, Wang JG. Blood pressure in relation to interactions between sodium dietary intake and renal handling. Hypertension. 2013;62:719–25.
Gelzinsky J, Mayer O Jr, Seidlerova J, Materankova M, Mares S, Kordíkova V, et al. Serum biomarkers, skin autofluorescence and other methods. Which parameter better illustrates the relationship between advanced glycation end products and arterial stiffness in the general population? Hypertens Res. 2021;44:518–27.
Liu CY, Huang QF, Cheng YB, Guo QH, Chen Q, Li Y, et al. A comparative study on skin and plasma advanced glycation end products and their associations with arterial stiffness. Pulse. 2016;4:208–18.
Zieman SJ, Melenovsky V, Kass DA. Mechanisms, pathophysiology, and therapy of arterial stiffness. Arterioscler Thromb Vasc Biol. 2005;25:932–43.
Chinese Diabetes Society. Guideline for the prevention and treatment of type 2 diabetes mellitus in China (2020 edition). Chin J Diabetes Mellitus. 2021;13:315–409.
O’Brien E, Parati G, Stergiou G, Asmar R, Beilin L, Bilo G, et al. European society of hypertension position paper on ambulatory blood pressure monitoring. J Hypertens. 2013;31:1731–68.
Kang YY, Cheng YB, Guo QH, Sheng CS, Huang QF, Xu TY, et al. Renal sodium handling in relation to environmental and genetic factors in untreated Chinese. Am J Hypertens. 2021;34:394–403.
Acknowledgements
We gratefully acknowledge the voluntary participation of all patients and the expert technical support of the technical staff from The Shanghai Institute of Hypertension (Junwei Li, Beiwen Lv, Jiaye Qian, Yuzhong Shi, Qian Yu, Jie Zhou, Yi Zhou, Yini Zhou, and Jiajun Zong).
Funding
This study was financially supported by grants from the National Natural Science Foundation of China (grants 81970353, 82070432, 82070435, 81770455, 91639203, 81400312 and 81470533); the Ministry of Science and Technology (2016YFC0900902, 2016YFC1300100, and 2018YFC1704902), Beijing, China; the Shanghai Commissions of Science and Technology (grants 19ZR1443300, 19YF1441000, 15XD1503200 and 14ZR1436200); the Shanghai Municipal Health Commission (201940297, 20204Y0001, 2017BR025, 15GWZK0802 and a Grant for Leading Academics); and the Three-year Action Program of Shanghai Municipality for Strengthening the Construction of Public Health System (GWV-10.1-XK05) Big Data and Artificial Intelligence Application, Shanghai, China.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Huang, QF., Cheng, YB., Guo, QH. et al. Clinic and ambulatory blood pressure in relation to the interaction between plasma advanced glycation end products and sodium dietary intake and renal handling. Hypertens Res 45, 665–674 (2022). https://doi.org/10.1038/s41440-021-00805-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-021-00805-z
Keywords
This article is cited by
-
2023 update and perspectives
Hypertension Research (2024)
-
Seasonality in nighttime blood pressure and its associations with target organ damage
Hypertension Research (2023)
-
AGEs and renal sodium handling: association with hypertension
Hypertension Research (2022)