Abstract
The sodium-to-potassium ratio (Na/K) of a urine sample is a simple index of salt loading. To practically use Na/K, we aimed to determine whether the Na/K value affects blood pressure (BP) at any age, irrespective of urinary Na and K levels. We analyzed a dataset of the general population (the Nagahama study), including baseline and second-visit measurements performed 5 years after the baseline. Spot urine samples were used for Na/K assessments. A total of 18,505 observations were analyzed using a linear mixed model, including the measurement term as a random effect. Urinary Na/K values showed a positive association with BP. When the highest quartile of Na/K was further divided by the urinary Na/creatinine (Cre) and K/Cre levels, the high-Na/Cre (3.58) and high-K/Cre (0.75) (Na/K = 4.80) groups, as well as the low Na/Cre (1.23) and low-K/Cre (0.26) (Na/K = 4.87) groups, exhibited similar effects on systolic BP (6.82 mmHg [95% CI: 5.72–7.92] and 6.63 mmHg [95% CI: 5.35–7.91], respectively). A similar association was observed in other Na/K quartiles. The positive association of Na/K and Na/Cre with BP was steeper in the older groups, while the inverse association of K/Cre was predominant in the younger population. The results of the multivariate analysis identified interaction terms between age and Na/K, Na/Cre and K/Cre as significant determinants for SBP. The positive association of urinary Na/K with BP was independent of the urinary Na and K levels. The association between Na/K and BP may not be uniform across ages by decade.
Similar content being viewed by others
Introduction
Excessive salt intake is an established risk factor for hypertension [1] and may influence arterial properties [2] and increase cardiovascular disease risk [3]. Accurate assessment of daily salt intake is therefore important for hypertension prevention, as well as for blood pressure (BP)-lowering interventions, including antihypertensive medications. Measurement of the 24-h urinary sodium (Na) excretion is the most reliable method for estimating daily salt intake, although 24-h urine collection is troublesome and cannot be easily adapted for clinical and epidemiological settings. Another method to estimate daily salt intake includes the calculation of 24-h urinary Na excretion using second morning voiding urine [4] or spot urine samples [5]. Although these equations have been used in several epidemiological studies [6], the accuracy of estimation is limited by the large dispersion between the estimation and actual measurements of urinary Na and K values [1, 4].
The sodium-to-potassium ratio (Na/K) of a urine sample is another simple index of salt loading not affected by the urine volume and therefore does not require creatinine measurement. Furthermore, as the potassium excretion level is inversely associated with BP [6], the association between Na/K and BP [1, 7] and end organ damage [8, 9] has been reported to be superior to either measure alone. Although these studies were based on 24-h urine samples, our preceding study revealed that the association of Na/K with BP was superior to that of estimated daily salt intake, even when a spot urine sample was used for analysis [10]. However, because Na/K is a ratio and not an absolute value, it is unclear whether the same Na/K values have a similar influence on BP irrespective of the Na and K levels. Thus, we proposed to discern whether the same Na/K values calculated as a high Na-to-high K ratio and a low Na-to-low K ratio have similar influences on BP.
To support the practical use of Na/K as an index of salt loading, we analyzed a dataset of the Nagahama study, a large-scale general population-based study in Japan, with twice-measured clinical values, including a spot urine sample. Because urinary Na/K and BP values involve random measurement errors, multiple measurements are preferable for their association analysis. We also investigated age-dependency in the relationship between urinary Na/K and BP.
Methods
Study participants
We analyzed the datasets from the Nagahama study [11, 12]. Participants were recruited from the general population of Nagahama, a rural city located in central Japan inhabited by ~125,000 people.
A baseline investigation of the Nagahama study was performed between 2008 and 2010. Community residents aged 30–74 years living independently without any physical impairment or dysfunction were eligible. Of 9764 participants at baseline, a total of 9154 participants were included in the analysis after excluding individuals who met the following criteria: pregnancy (n = 42), unavailability of urinary Na and K values due to menstruation (n = 438), severe renal functional decline (estimated glomerular filtration rate [eGFR] < 30 mL/min/1.73 m2 or urinary albumin ≥ 300 mg/g creatinine [Cre]; n = 82), incomplete clinical values or responses to the questionnaire administered (n = 31), pacemaker implantation (n = 10), receipt of hemodialysis therapy (n = 2) at the second health survey, and wide deviation of urinary Na and K values (Mahalanobis distance > 7, n = 5).
Of the baseline population, 8289 individuals participated in the second health survey performed 5 years after the baseline evaluation (2013–2016). By further recruiting 1561 participants meeting the inclusion criteria, the second-visit dataset of the Nagahama Study comprised 9850 participants. A total of 9351 participants were included in the analysis after excluding 499 individuals who met the same exclusion criteria as described above.
This study was approved by the Ethics Committee of the Kyoto University Graduate School of Medicine and by the Nagahama Municipal Review Board. Written informed consent was obtained from all study participants.
Spot urine samples
Spot urine samples were collected at the baseline measurement (0900–1700 h) and the second-visit measurement (0800–1400 h). Urinary Na, K, and Cre levels were measured on each day of sampling. The time since the last meal was recorded for each participant. Quartiles of Na/K, as well as of Na/Cre and K/Cre, were calculated within the baseline and the second-visit datasets and then combined to avoid potential stratification.
BP measurement
Brachial BP was measured after a 5-min rest in the sitting position using a cuff-oscillometric device (HEM-9000AI; Omron Healthcare, Kyoto, Japan). Measurements were taken twice, and the mean value was used in the analysis. Hypertension was defined as a participant meeting any or all of the following criteria: SBP ≥ 140 mmHg, diastolic BP ≥ 90 mmHg, or taking antihypertensive drugs.
Basic clinical parameters
The basic clinical parameters used in this study were obtained at the baseline and the second-visit measurements. Daily salt intake was estimated from spot urine Na and Cre values using the following formula: [5] 21.98 × {Na (mEq/l) × predicted 24-h Cre excretion / [Cre (mg/dl) × 10]}0.392 × 0.0585, where the 24-h Cre excretion was predicted using the following formula: body weight (kg) × 14.89 + body height (cm) × 16.14 − age × 2.04 − 2444.45. Renal function was assessed by the eGFR calculated using the following formula: 194 × Cre−1.094 × age−0.287 × 0.739 (if female) [13]. Alcohol consumption was obtained by a self-administered questionnaire using Japanese traditional units of alcohol (Go), where 1 Go corresponds to 22 g of ethanol. The use of antihypertensive drugs was also assessed by using a questionnaire.
Statistical analysis
Values are presented as the mean ± standard deviation or frequency. Group differences in numeric variables were assessed by analysis of variance. Linear mixed model analysis using a total of 18,505 observations (baseline observations: 9154; second-visit observations: 9351) was applied to identify independent determinants for SBP. The linear mixed model included the measurement term (baseline or second-visit measurements) as a random effect, while the following factors were included as fixed effects: age, sex, body mass index, alcohol consumption, antihypertensive medication, eGFR, fasting condition, and measurement season. Covariate-adjusted group differences in SBP were also calculated by the linear mixed model. Statistical analyses were performed using JMP version 14.3.0 software (SAS Institute, Cary, NC, USA). A P value of less than 0.05 was considered statistically significant.
Results
The clinical characteristics of the study participants are summarized in Table 1. Of a total of 11,012 participants, 7493 individuals participated in both the baseline and second-visit measurements, whereas 1661 and 1858 individuals, respectively, participated in either the baseline or second-visit measurement.
Brachial SBP was positively associated with Na/Cre quartiles and inversely associated with K/Cre quartiles (Supplementary Figure 1); thus, it linearly increased with Na/K quartiles in either analysis using the baseline dataset (Q1: 121 ± 17, Q2: 122 ± 18, Q3: 124 ± 17, and Q4: 127 ± 18 mmHg, P < 0.001) or the second-visit dataset (Q1: 121 ± 17, Q2: 124 ± 17, Q3: 126 ± 18, and Q4: 129 ± 19 mmHg, P < 0.001). However, there were wide variations in Na/Cre and K/Cre values within the Na/K quartiles, and the distributions largely overlapped among the quartiles (Supplementary Fig. 2), suggesting a wide variation in Na and K excretion levels even when the Na/K value was constant. In addition, several clinical factors were also different among the Na/K quartiles (Supplementary Tables 1).
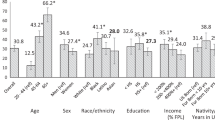
To clarify whether the association of Na/K with BP was independent of urinary Na and K levels, the adjusted SBP of each Na/K quartile was calculated by further subdividing the quartiles at the median of urinary Na/Cre and K/Cre (Supplementary Fig. 3). Figure 1 depicts group differences in the adjusted SBP calculated by the mixed model analysis using the low-Na and low-K subgroups of the first Na/K quartile as a reference. There were no substantial differences in BP between the low Na−low K and high Na−high K subgroups in each quartile, and the association of Na/K with SBP was independent of urinary Na and K levels (Table 2). The number of measurements and mean Na/K, Na/Cre, and K/Cre values in all subgroups are summarized in Supplementary Table 2. Similar results were observed in the analysis of participants not taking antihypertensive drugs (Supplementary Fig. 4).
Differences in SBP by Na/K quartiles and urinary Na/Cre and K/Cre. Upper panel: Values are the estimated SBP difference and 95% confidence intervals calculated by the linear mixed model using the low-Na and low-K subgroup of the first Na/K quartile as a reference. The model included measurement term as a random effect, while the following factors were included as fixed effects: age, sex, body mass index, alcohol consumption, antihypertensive medication, eGFR, fasting condition, and measurement season. Study participants were subdivided by Na/K quartiles (baseline: Q1: <1.97, Q2: <2.82, Q3: <3.98, and Q4 ≥3.98; second visit: Q1: <1.79, Q2: <2.54, Q3: <3.57, and Q4 ≥2.57), as well as the medians of Na/Cre (baseline: 167 mEq/gCre; second visit: 146 mEq/gCre) and K/Cre (baseline: 59 mEq/gCre; second visit: 58 mEq/gCre) (Supplementary Figure 3). The number of measurements, as well as the mean Na/K, Na/Cre, and K/Cre, of all subgroups are summarized in Supplementary Table 2. §P = 0.153, #P < 0.001. Lower panel: crude mean SBP calculated by the linear regression model included measurement term as a random effect
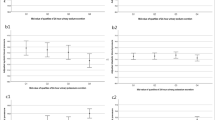
Figure 2a depicts age-dependency in the association between urinary Na/K and SBP. When covariate-adjusted SBP differences by Na/K quartiles and by age decades were calculated using the first quartile of the youngest subgroup as a reference, the SBP increased linearly with the Na/K quartiles in any age group, although the correlation was steeper in the older groups. In a separate analysis by urinary Na (Fig. 2b) and K (Fig. 2c) levels, SBP in the older groups linearly increased with the Na/Cre quartiles (Fig. 2b), but not with the K/Cre quartiles (Fig. 2c), whereas SBP in the younger groups had an inverse association with K/Cre quartiles (Fig. 2c). Similar results were observed upon analyzing participants who were not taking antihypertensive drugs (Supplementary Figure 5). The results of the linear mixed model analysis (Table 3) identified the interaction term age × Na/K (Model 1) and the interaction terms between age and Na/Cre (Model 2) and K/Cre (Model 3) as significant determinants for SBP. The number of measurements in each subgroup is summarized in Supplementary Table 3.
Age-dependent association of urinary Na/K, Na/Cre, and K/Cre with SBP. Values are estimated SBP differences and 95% confidence intervals calculated by the linear mixed model using the first quartiles of the youngest subgroup as a reference. The model included measurement term as a random effect, while the following factors were included as fixed effects: sex, body mass index, alcohol consumption, antihypertensive medication, eGFR, fasting condition, and measurement season. Age was not included in the model to stratify the participants by decade. Study participants were subdivided by quartiles of Na/K (baseline: Q1: <1.97, Q2: <2.82, Q3: <3.98, and Q4: ≥3.98; second visit: Q1: <1.79, Q2: <2.54, Q3: <3.57, and Q4: ≥2.57), Na/Cre (baseline: Q1: <115, Q2: <167, Q3: <232, and Q4: ≥232 mEq/gCre, second visit: Q1: <98, Q2: <146, Q3: <208, and Q4: ≥208 mEq/gCre) and K/Cre (baseline: Q1: <44, Q2: <59, Q3: <77, and Q4: ≥77 mEq/gCre, second visit: Q1: <42, Q2: <58, Q3: <76, and Q4: ≥76 mEq/gCre). The number of measurement values in each subgroup is shown in Supplementary Table 3
Discussion
In this cross-sectional analysis of a large general population with twice-measured clinical values, we clarified that the positive association of urinary Na/K and BP was independent of the ratio composition, i.e., the same Na/K values calculated as high Na-to-high K ratio and low Na-to-low K ratio had similar influences on BP. Na/K is therefore a simple risk marker for hypertension that does not require consideration of the Na and K excretion levels. The association between Na/K and BP may not be uniform across age by decade, particularly when the association of Na and K is analyzed separately. Age-dependent nutritional intervention may be a better approach to decrease Na/K.
Urinary excretory Na and K levels were oppositely associated with SBP in accordance with previous studies [14], and the ratio of Na and K showed a linear additive association with BP. Importantly, the association of Na/K with BP was independent of the Na and K levels, i.e., even a smaller amount of Na intake may have the potential to be a risk factor for increasing BP when K intake is limited. Similar results, i.e., an association of Na/K with BP that did not differ by the amount of daily salt intake, were reported from another observational study [15]. In addition to the reduction of salt intake, a well-established method to reduce BP [16], our finding emphasizes the importance of K supplementation for BP reduction. Such a BP-lowering effect has been reported in several studies [17, 18]. We previously reported [11] a positive association of vegetable, fruit, and dairy product consumption with urinary K excretion levels, whereas a lower education level was associated with smaller amounts of K excretion.
The results of the present study indicate the possibility that a high salt intake may not always be deleterious when the K consumption is adequate. Previous experimental studies in humans [19] and animals [20] have reported that K supplementation may compensate for the BP-raising effect of salt loading. However, considering the large differences in the absolute levels of Na/Cre and K/Cre among the Na/K quartiles, it might be difficult to maintain Na/K sufficiently enough to lower the BP levels via only K supplementation. Furthermore, as this study had a cross-sectional setting, the longitudinal effect of the compensatory action of K must be clarified.
The positive association between Na excretion level and BP was prominent in the older subpopulation. Because older persons are more likely to be salt-sensitive [21] as a result of reduced kidney function, Na excretion levels may be more closely associated with BP than K excretion levels are. Previously, our findings in the same population [9], namely, that decreases in Na excretion due to renal functional decline were larger than those in K excretion, also supported this consideration. Although we adjusted for renal function (eGFR) in this analysis, this step might not have been adequate to control for individual differences in salt sensitivity because several factors, particularly muscle mass decline, in the older population may have large influences on serum Cre levels [22]. In contrast, in the younger population, the K, but not Na, excretion level was inversely associated with BP, suggesting salt wasting as a primary factor for lower BP in healthy individuals with better renal function. The results of previous interventional studies [23, 24] reporting BP-lowering effects of K supplementation in middle-aged normotensive individuals support our present findings. For public health practitioners, age-dependent nutritional intervention, i.e., salt restriction in older persons and K supplementation in younger individuals, may be a better approach to decrease Na/K with an aim to reduce the BP.
Na/K has been reported to be more closely associated with BP than the estimated salt intake [1, 7]. A plausible explanation for the superior association of Na/K has been suggested to be the opposite effects of Na and K with respect to BP. However, considering the present findings, a weak association of urinary Na with BP in the younger population may be another reason because the equation for salt intake estimation only requires urinary Na levels [4, 5]. The strong inverse association of urinary K with BP in younger populations may compensate for the weak association of Na in this age group and account for the positive association of Na/K with BP across all age groups.
An advantage of this study is the large population size with repeated measurements of urinary Na/K after 5 years. Although urinary electrolyte and BP values involve random measurement errors, the use of repeated measurements may have decreased bias. However, there are several limitations in this study. First, we used spot urine samples (obtained at the health check-up program performed as part of the cohort study), which may not always r epresent daily salt intake. Indeed, the estimated daily salt intake in this study population was slightly lower than that estimated by the National Health and Nutrition Survey (9.9 g/day). However, as we used repeated measurements of urinary Na/K that helped to close the estimation of 24-h urine Na/K [25], the slight discrepancy in daily salt intake would not cause a serious bias. Second, several samples were obtained under nonfasting conditions, although a previous study reported a diurnal variation in urinary Na/K [26]. We therefore adjusted for fasting time in the analyses to avoid potential bias. Third, our study population was monolithic, comprising only Japanese individuals, for whom the within-country variation in salt intake was small [27]. Additional studies in other populations are warranted to generalize the present findings.
In summary, our study emphasizes the usefulness of urinary Na/K as a risk factor for hypertension, irrespective of excretion levels of Na and K. Age-dependent nutritional approaches, such as salt restriction in older populations and K supplementation in younger populations, may decrease the urinary Na/K and thereby prevent hypertension.
References
Adrogué HJ, Madias NE. Sodium and potassium in the pathogenesis of hypertension. N Engl J Med. 2007;356:1966–78. https://doi.org/10.1056/NEJMra064486
Han W, Han X, Sun N, Chen Y, Jiang S, Li M. Relationships between urinary electrolytes excretion and central hemodynamics, and arterial stiffness in hypertensive patients. Hypertens Res. 2017;40:746–51. https://doi.org/10.1038/hr.2017.29
Liu H, Gao X, Zhou L, Wu Y, Li Y, Mai J, et al. Urinary sodium excretion and risk of cardiovascular disease in the Chinese population: a prospective study. Hypertens Res. 2018;41:849–55. https://doi.org/10.1038/s41440-018-0091-8
Kawasaki T, Itoh K, Uezono K, Sasaki H. A simple method for estimating 24 h urinary sodium and potassium excretion from second morning voiding urine specimen in adults. Clin Exp Pharm Physiol. 1993;20:7–14.
Tanaka T, Okamura T, Miura K, Kadowaki T, Ueshima H, Nakagawa H, et al. A simple method to estimate populational 24-h urinary sodium and potassium excretion using a casual urine specimen. J Hum Hypertens. 2002;16:97–103. https://doi.org/10.1038/sj.jhh.1001307
Mente A, O'Donnell MJ, Rangarajan S, McQueen MJ, Poirier P, Wielgosz A, et al. PURE Investigators. Association of urinary sodium and potassium excretion with blood pressure. N Engl J Med. 2014;371:601–11. https://doi.org/10.1056/NEJMoa1311989
Morris RC Jr, Sebastian A, Forman A, Tanaka M, Schmidlin O. Normotensive salt sensitivity: effects of race and dietary potassium. Hypertension. 1999;33:18–23.
Rodriguez CJ, Bibbins-Domingo K, Jin Z, Daviglus ML, Goff DC Jr, Jacobs DR Jr.. Association of sodium and potassium intake with left ventricular mass: coronary artery risk development in young adults. Hypertension. 2011;58:410–6. https://doi.org/10.1161/HYPERTENSIONAHA.110.16805
Cook NR, Obarzanek E, Cutler JA, Buring JE, Rexrode KM, Kumanyika SK, et al. Trials of Hypertension Prevention Collaborative Research Group. Joint effects of sodium and potassium intake on subsequent cardiovascular disease: the Trials of Hypertension Prevention follow-up study. Arch Intern Med. 2009;169:32–40. https://doi.org/10.1001/archinternmed.2008.523
Tabara Y, Takahashi Y, Kumagai K, Setoh K, Kawaguchi T, Takahashi M, et al. Nagahama study group. Descriptive epidemiology of spot urine sodium-to-potassium ratio clarified close relationship with blood pressure level: the Nagahama study. J Hypertens. 2015;33:2407–13. https://doi.org/10.1097/HJH.0000000000000734
Yamashita M, Tabara Y, Higo Y, Setoh K, Kawaguchi T, Takahashi Y, et al. Nagahama Study group. Association between socioeconomic factors and urinary sodium-to-potassium ratio: the Nagahama Study. Hypertens Res. 2018;41:973–80. https://doi.org/10.1038/s41440-018-0101-x
Tabara Y, Igase M, Setoh K, Kawaguchi T, Okada Y, Ohara M, et al. J-SHIPP and Nagahama study groups. Clinical significance of an elevated ankle-brachial index differs depending on the amount of appendicular muscle mass: the J-SHIPP and Nagahama studies. Hypertens Res. 2018;41:354–62. https://doi.org/10.1038/s41440-018-0020-x
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–92. https://doi.org/10.1053/j.ajkd.2008.12.034
Jackson SL, Cogswell ME, Zhao L, Terry AL, Wang CY, Wright J, et al. Association between urinary sodium and potassium excretion and blood pressure among adults in the United States: National Health and Nutrition Examination Survey, 2014. Circulation. 2018;137:237–46. https://doi.org/10.1161/CIRCULATIONAHA.117.029193
Yin L, Deng G, Mente A, Sun Y, Liu X, Zhang X, et al. Association patterns of urinary sodium, potassium, and their ratio with blood pressure across various levels of salt-diet regions in China. Sci Rep. 2018;8:6727 https://doi.org/10.1038/s41598-018-25097-1
He FJ, Li J, Macgregor GA. Effect of longer term modest salt reduction on blood pressure: cochrane systematic review and meta-analysis of randomized trials. BMJ. 2013;346:f1325 https://doi.org/10.1136/bmj.f1325
Whelton PK, He J, Cutler JA, Brancati FL, Appel LJ, Follmann D, et al. Effects of oral potassium on blood pressure. Meta-analysis of randomized controlled clinical trials. JAMA. 1997;277:1624–32.
Aaron KJ, Sanders PW. Role of dietary salt and potassium intake in cardiovascular health and disease: a review of the evidence. Mayo Clin Proc. 2013;88:987–95. https://doi.org/10.1016/j.mayocp.2013.06.005
Liu Z, Peng J, Lu F, Zhao Y, Wang S, Sun S, et al. Salt loading and potassium supplementation: effects on ambulatory arterial stiffness index and endothelin-1 levels in normotensive and mild hypertensive patients. J Clin Hypertens. 2013;15:485–96. https://doi.org/10.1111/jch.12109
Tobian L. Dietary sodium chloride and potassium have effects on the pathophysiology of hypertension in humans and animals. Am J Clin Nutr. 1997;65:606S–611S. https://doi.org/10.1093/ajcn/65.2.606S
Elijovich F, Weinberger MH, Anderson CA, Appel LJ, Bursztyn M, Cook NR, et al. American Heart Association Professional and Public Education Committee of the Council on Hypertension; Council on Functional Genomics and Translational Biology; and Stroke Council. Salt sensitivity of blood pressure: a scientific statement from the American Heart Association. Hypertension. 2016;68:e7–e46. https://doi.org/10.1161/HYP.0000000000000047
Baxmann AC, Ahmed MS, Marques NC, Menon VB, Pereira AB, Kirsztajn GM, et al. Influence of muscle mass and physical activity on serum and urinary creatinine and serum cystatin C. Clin J Am Soc Nephrol. 2008;3:348–54. https://doi.org/10.2215/CJN.02870707
Braschi A, Naismith DJ. The effect of a dietary supplement of potassium chloride or potassium citrate on blood pressure in predominantly normotensive volunteers. Br J Nutr. 2008;99:1284–92.
Naismith DJ, Braschi A. The effect of low-dose potassium supplementation on blood pressure in apparently healthy volunteers. Br J Nutr. 2003;90:53–60.
Iwahori T, Ueshima H, Miyagawa N, Ohgami N, Yamashita H, Ohkubo T, et al. Six random specimens of daytime casual urine on different days are sufficient to estimate daily sodium/potassium ratio in comparison to 7-day 24-h urine collections. Hypertens Res. 2014;37:765–71. https://doi.org/10.1038/hr.2014.76
Iwahori T, Ueshima H, Torii S, Saito Y, Kondo K, Tanaka-Mizuno S, et al. Diurnal variation of urinary sodium-to-potassium ratio in free-living Japanese individuals. Hypertens Res. 2017;40:658–64. https://doi.org/10.1038/hr.2016.187
Uechi K, Asakura K, Masayasu S, Sasaki S. Within-country variation of salt intake assessed via urinary excretion in Japan: a multilevel analysis in all 47 prefectures. Hypertens Res. 2017;40:598–605. https://doi.org/10.1038/hr.2016.185
Acknowledgements
The authors thank the Nagahama City Office and the nonprofit organization Zeroji Club for their assistance in performing the Nagahama study. They also thank Crimson Interactive Pvt. Ltd. for editing the manuscript.
Funding
The study was supported by a university grant, The Center of Innovation Program, The Global University Project, and a Grant-in-Aid for Scientific Research (25293141, 26670313, 26293198, 17H04182, and 17H04126, 17H04123, 18K18450) from the Ministry of Education, Culture, Sports, Science, and Technology of Japan: the Practical Research Project for Rare/Intractable Diseases (ek0109070, ek0109070, ek0109196, ek0109348), the Comprehensive Research on Aging and Health Science Research Grants for Dementia R&D (dk0207006, dk0207027), the Program for an Integrated Database of Clinical and Genomic Information (kk0205008), and the Practical Research Project for Lifestyle-related Diseases including Cardiovascular Diseases and Diabetes Mellitus (ek0210066, ek0210096, ek0210116), and the Research Program for Health Behavior Modification by Utilizing IoT (le0110005), from the Japan Agency for Medical Research and Development (AMED); the Takeda Medical Research Foundation; the Mitsubishi Foundation; Daiwa Securities Health Foundation, and Sumitomo Foundation.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Higo, Y., Nagashima, S., Tabara, Y. et al. Association of the spot urine sodium-to-potassium ratio with blood pressure is independent of urinary Na and K levels: The Nagahama study. Hypertens Res 42, 1624–1630 (2019). https://doi.org/10.1038/s41440-019-0276-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-019-0276-9
Keywords
This article is cited by
-
Prediction of endogenous mineralocorticoid receptor activity by depressor effects of mineralocorticoid receptor antagonists in patients with primary aldosteronism
Hypertension Research (2024)
-
Spot urinary sodium-to-potassium ratio is associated with blood pressure levels in healthy adolescents: the Wakayama Study
Journal of Human Hypertension (2023)
-
The spot urine sodium-to-potassium ratio as a marker of hypertension risk
Hypertension Research (2022)
-
Investigation of the urinary sodium-to-potassium ratio target level based on the recommended dietary intake goals for the Japanese population: The INTERMAP Japan
Hypertension Research (2022)
-
Sodium/potassium ratio change was associated with blood pressure change: possibility of population approach for sodium/potassium ratio reduction in health checkup
Hypertension Research (2021)