Abstract
The aim of this trial was to evaluate the feasibility and effect of home-based transcutaneous electrical acupoint stimulation (TEAS) in patients with hypertension. In this randomized pilot trial, patients with hypertension were randomly assigned to the TEAS group or the usual care group. Participants in the usual care group were instructed to continue taking their antihypertensive drugs and received education on lifestyle modifications. In addition, participants in the TEAS group received 4 weekly sessions of noninvasive acupoint stimulation for 12 weeks at home. The primary outcome was the change in office systolic blood pressure at week 12 from baseline. Withdrawal from the study and adverse events associated with TEAS were also recorded. Sixty patients were randomized, with 30 patients in the TEAS group, of whom 1 was lost at week 36, and 30 patients in the usual care group, of whom 3 were lost by week 12. The reduction in systolic blood pressure at week 12 was greater in the TEAS group (−8.53 mm Hg; 95% CI [−13.37, −3.70 mm Hg]) than in the usual care group (−1.70 mm Hg; 95% CI [−4.29, −0.89 mm Hg]), with a between-group difference of −6.83 mm Hg (95% CI, [−12.23, −1.43 mm Hg]; P = 0.014). No TEAS-related adverse events occurred. In conclusion, home-based TEAS added to usual care for patients with hypertension was acceptable and safe and may be a potential treatment option. A larger randomized controlled trial of this intervention is warranted.
Similar content being viewed by others
Introduction
Hypertension is a common risk factor for cardiovascular diseases. Cardiovascular disease morbidity and mortality are positively correlated with the degree of elevation of blood pressure [1]. According to the World Health Organization (WHO), the global prevalence of hypertension is 20% for females and 25% for males, implying that 1.13 billion people are affected [2]. Hypertension accounted for 9.4 million deaths and 7.0% of global disability-adjusted life-years (DALYs) in 2010 [3]. By 2030, the total costs of hypertension could increase to $274 billion [4]. Hypertension has become a vital public health problem.
Lifestyle modifications are recommended by all guidelines in different countries [5,6,7], which include the Dietary Approaches to Stop Hypertension (DASH) diet, reduced dietary sodium intake, exercise, reduced alcohol intake, and weight loss if overweight. Unfortunately, the reality is that most patients are unable to start or sustain lifestyle changes. Although antihypertensive drugs are widely prescribed for patients with hypertension, only half of them have controlled blood pressure [4, 8]. The reasons for the low control rate of blood pressure may include poor adherence. Identifying novel nonpharmaceutical therapies that allow for high adherence is urgently needed.
Acupuncture, as a nonpharmaceutical therapy, is used for cardiovascular diseases, including chronic stable angina [9], heart failure [10] and hypertension [11, 12]. A recent systematic review found that acupuncture as adjunctive therapy may be effective for hypertension [13]. However, acupuncture has the limitations of logistical burdens and patient aversion to needles. Transcutaneous electrical acupoint stimulation (TEAS), a noninvasive acupuncture treatment, has a similar effect as electroacupuncture but could be performed at home by patients themselves. The aim of this randomized controlled pilot trial was to evaluate the feasibility and effect of home-based TEAS as an adjunctive therapy for hypertension.
Methods
Study design
This two-armed, randomized, controlled, outcome assessor-blind pilot trial was approved by the ethics committee of Beijing University of Chinese Medicine (No 2019BZHYLL0208) and was conducted in accordance with the Declaration of Helsinki. The protocol was registered in the Chinese clinical trial registry (No ChiCTR1900025042) prior to participant enrollment and was previously published [14]. Protocol changes, including the removal of the secondary outcome of heart rate variability and the addition of the secondary outcome of the 8-item Morisky Medication Adherence Scale (MMAS-8), were made before recruitment of patients. Written informed consent was provided by all participants before randomization. The TEAS instrument was given to the patients for free.
Participants
Participants were recruited at Nanyuan Community Health Service Center in Beijing through the community’s hypertension patient cohort and on-site flyers at the outpatient department. Patients who had been diagnosed with grade 1 hypertension according to the European and Chinese guidelines [5, 6], were eligible if they ① were 35–65 years old, ② had systolic blood pressure (SBP) from 140 to 159 mm Hg and/or diastolic blood pressure (DBP) from 90 to 99 mm Hg for patients who did not take antihypertensive drugs previously or SBP from 120 to 159 mm Hg and/or DBP from 80 to 99 mm Hg for patients who did not change antihypertensive therapy within the last 1 month, ③ could complete the study questionnaires and ④ signed an informed consent form. Exclusion criteria included the following: secondary hypertension (primary aldosteronism, renal artery stenosis, etc.), contraindications for the use of the TEAS instrument (wearing a pacemaker or other implanted medical devices or scars, bruises, scratches or inflammation on the skin of LI4, LI11, ST36, or LR3), use of drugs that affect blood pressure except antihypertensive drugs in the previous 2 months (glucocorticoids, central nervous system inhibitors, etc.), uncontrolled diabetes, drug or alcohol abuse, pregnancy or lactation, acupuncture treatment or participation in another clinical study within the past month.
Randomization and masking
Eligible patients were randomly assigned to the TEAS group or usual care group at a ratio of 1:1 using a randomization sequence generated with SAS 9.3 software by an independent statistician (Li-Qiong Wang, Beijing University of Chinese Medicine). The block size of randomization sequence was 4. Details about allocation concealment were described in the published protocol [14]. The patients and the acupuncturists who taught patients how to locate acupoints and use the TEAS instrument were not blinded. However, outcome assessors and statisticians were blinded to group allocation.
Interventions
Usual care group
If patients were on antihypertensive medication, they were instructed to continue this medication but to abstain from changing the type or dosage of drugs. Relevant antihypertensive information was sent to patients every week. The content of this information included the hazard of hypertension; the benefit of controlling blood pressure; influence of lifestyle on hypertension control, especially the importance of diet; and the importance of performing moderate physical exercise, maintaining normal weight and quitting smoking.
TEAS group
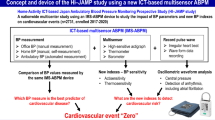
In addition to usual care, the participants in the TEAS group received 48 sessions of acupoint stimulation over a period of 12 weeks (4 sessions/week, ideally every other day) at home. TEAS was performed using a portable instrument for low-frequency electrotherapy (SDP-330, Yuwell, Suzhou Medical Appliances Co, Ltd., Suzhou, China). Patients were told that the acupoint stimulation could be done when the participants were spending leisure time at home. According to a previous study [15] and our clinical experience, bilateral Hegu (LI4), Quchi (LI11), Zusanli (ST36), and Taichong (LR3) were used in our trial. In the first session, the electrodes were placed at the ipsilateral LI4 and LI11, and then the patients chose the appropriate stimulus intensity according to their tolerance. The TEAS would end automatically after 15 min. Then, the same acupoints on the opposite limb were stimulated in the same way for 15 min. In the second session, the ST36 and LR3 acupoints of the leg were treated for 15 min in the same way. Two pairs of acupoints were stimulated alternatively every other day. Locations of acupoints are shown in Supplementary Table 1 and Supplementary Fig. 1. The acupuncturists trained the participants on how to locate the acupoints and use the TEAS instrument face-to-face in the first week. Instructions and acupoint maps were created to help patients perform the TEAS treatment at home. The patients were instructed to record the date, time, and specific acupoints when using the instrument.
Outcomes
Primary outcome
The primary outcome of the study was the change in mean SBP at week 12 from baseline. SBP was measured and recorded by using an electronic sphygmomanometer (HEM-7136, Omron Corporation, Kyoto, Japan) in office in both groups. Patients were asked to rest quietly for at least 5 min before taking blood pressure measurements on the upper arm in the sitting position, with the upper arm at heart level [16]. Blood pressures were measured on both upper arms at baseline. The side with higher blood pressure was selected as the research arm. At subsequent detection time points, the SBP measurement was repeated 3 times every 5 min, and the average value of the last 2 readings was taken as the mean blood pressure [17].
Secondary outcomes
Secondary outcomes, including mean DBP, body mass index (BMI), International Sports Activity Questionnaire (IPAQ), MMAS-8 and 12-item Short Form Health Survey (SF-12), were evaluated at baseline and weeks 12, 24 and 36. The DBP measurement method is consistent with the SBP measurement method. BMI was calculated as weight (kg) divided by the square of height. The IPAQ includes information on the frequency, intensity, timing, and type of exercise [18], which is used to divide physical activity into low, middle, and high levels according to metabolic equivalent. The SF-12 is a questionnaire to evaluate general health outcomes, including psychological and physical domains [19].
Adverse events
Any adverse events were reported by the patients and outcome assessors, including severe pain, local infection, or unbearable tingling during the trial. If any serious adverse events or uncontrolled hypertension occurred, patients immediately reported them to the primary investigator.
Statistical analysis
The following null hypothesis was tested for the primary outcome: there was no difference in SBP between the TEAS and usual care groups. Given that this was a pilot trial, the sample size was determined to be n = 60 participants based on the minimum sample size of a pilot trial [20].
Baseline characteristics were summarized in the two groups. Continuous variables were described using the mean ± standard deviation or median and quartile intervals if the normality assumption was violated. Categorical variables were described by frequencies and percentages. The primary outcome, the change in SBP between baseline and 12 weeks after treatment, was compared using Student’s t test based on the intention-to-treat principle, which included all randomized patients. Missing data were imputed using the last observation carried forward (LOCF) method. For secondary outcomes, Student’s t test, chi-squared test, Fisher’s exact test or the Wilcoxon rank sum test were used to test the differences in the outcomes, including DBP, BMI, IPAQ, and SF-12, between groups according to the distribution of variables. The relationship between compliance of TEAS and improvements in SBP at week 12 was explored as a post hoc analysis.
Statistical analyses were conducted by SPSS version 23.0 (IBM SPSS Statistics, New York, USA). There was no interim analysis or additional analyses in this trial. The level of significance was set at α < 0.05 for two-sided tests.
Results
Recruitment and retention
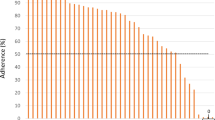
A total of 86 patients were screened from September 4th, 2019 to January 10th, 2020. Of them, 60 patients were included and randomly assigned to the two study groups (Fig. 1). By week 36, 56 patients (93.3%) had completed the follow-up. Baseline demographic and clinical characteristics were similar between the two groups (Table 1). Participants in the TEAS group received 44.43 ± 3.95 (mean ± standard deviation) sessions. Twenty-six (86.7%) participants attended 39 or more sessions (80% of targeted 48 sessions).
Scientific outcomes
For the primary outcome, the SBP was 130.00 mm Hg (95% CI, [125.47, 134.53 mm Hg]) at baseline and 121.47 mm Hg (95% CI, [117.03, 125.93 mm Hg]) at week 12 in the TEAS group and 129.10 mm Hg (95% CI, [124.88, 133.32 mm Hg]) at baseline and 127.40 mm Hg (95% CI, [123.38, 131.42 mm Hg]) at week 12 in the usual care group. The reduction in SBP at week 12 was greater in the TEAS group (mean, −8.53 mm Hg) than in the usual care group (−1.70 mm Hg), with a mean difference of −6.83 mm Hg (95% CI, −12.23, −1.43 mm Hg; P = 0.014) (Table 2). The improvements in SBP were related to compliance of TEAS (R2 = 0.28, P = 0.003) (Fig. 2). The benefit persisted through week 24 (mean difference, −7.03 mm Hg; 95% CI [−12.96, −1.11 mm Hg], P = 0.021), but by week 36, the difference was not significant (mean difference, −5.73 mm Hg; 95% CI [−11.94, 0.48 mm Hg], P = 0.070). No significant difference between groups was found in any secondary outcome (P > 0.05), except for the change in SF-12 physical health at week 24 (mean difference, 2.11; 95% CI [0.12, 4.09], P = 0.038) (Tables 2 and 3). Neither TEAS-related adverse events nor serious adverse events occurred.
Discussion
To our knowledge, this is the first randomized clinical trial to investigate the effect of home-based TEAS combined with usual care in hypertensive individuals. This trial found that TEAS as adjunctive therapy resulted in a significantly greater reduction in SBP at week 12 in patients with hypertension than usual care and that the benefit was sustained through week 36. Withdrawal from the TEAS group was no greater than that in the usual care group.
Trial feasibility
In this study, 70.0% (60/86) of individuals were randomized during the screening period. This recruitment rate reflects that patients with hypertension are willing to be involved in a trial and that TEAS as adjunctive therapy is acceptable. After a 12-week treatment period, at least 26 participants (86.7%) attended 80% of targeted sessions in the TEAS group. At 36 weeks after randomization, only 4 participants (6.7%) dropped out. Moreover, no TEAS-related adverse events occurred. The results from this pilot trial provide evidence regarding the feasibility and safety of TEAS as an adjunctive therapy in patients with hypertension. Accordingly, a future larger randomized controlled trial would be feasible. A sample size of 392 patients in each group was needed to assess SBP change on the basis of an alpha level of 0.025 (one-sided), a beta level of 0.80, an expected between-group difference of 6 mm Hg, a standard deviation of 10 mm Hg, and a superiority margin of 4 mm Hg [21].
Effects of TEAS on blood pressure
As a noninvasive acupuncture therapy, TEAS has the potential to lower blood pressure in patients with hypertension. A previous randomized, crossover trial found that electrical stimulation reduced office blood pressure by 5/1.5 mm Hg and that blood pressure was further reduced after washout [22]. Given the chronic nature of the disease, the relatively weak antihypertensive effect in that trial may be related to the shorter period of electrical stimulation. The period of electrical stimulation was 4 weeks in that trial, while the period in our trial was 12 weeks. The other reason may be that the mechanisms underlying different acupoints are diverse. Two acupoints (LI 4 and LI 10) on the arms were used in the previous trial. Four acupoints, two (LI 4 and LI 11) on the arms and two (ST36 and LR3) on the legs, were alternately stimulated in our trial.
Conventional acupuncture combined with antihypertensive drugs was found to be more effective than antihypertensive drugs alone for hypertension [23]. However, conventional acupuncture has the limitations of logistical burden and patient aversion to needles. As a noninvasive acupuncture therapy, TEAS can be performed at home by patients themselves without a prescription. To our knowledge, no study has directly compared the efficacy of TEAS to that of conventional acupuncture. This may be an interesting study in the future.
In agreement with the Food and Drug Administration, superiority is established by a margin of 4 mm Hg for SBP and by a margin of 2 mm Hg for DBP [24]. The changes in both SBP (−6.83 mm Hg) and DBP (−4.60 mm Hg) exceeded the superiority margins of SBP and DBP. Furthermore, a cohort study with 36,022 hypertension patients found that the hazard ratios for major adverse cardiovascular events and all-cause mortality and myocardial infarction were significantly lower in the acupuncture group than in the nonacupuncture group [25].
Mechanism of TEAS for hypertension
The underlying mechanism of the blood pressure-lowering effect of TEAS is not yet well known. A recent study suggested that transcutaneous electrical stimulation decreases sympathetic nervous system activity and increases parasympathetic nervous system activity [26]. Electrical stimulation has also been shown to have a vasodilator effect, which may contribute to reducing blood pressure [27]. Acupuncture could decrease high blood pressure and nicotinamide adenine dinucleotide phosphate oxidase in the rostral ventrolateral medulla of spontaneously hypertensive rats, and mitogen-activated protein kinases and the sciatic nerve were involved in the mechanism of acupuncture’s amelioration of hypertension [28].
Study limitations
This trial has several limitations. First, the participants in the trial were not blinded; however, the primary outcome was relatively objective. TEAS was performed at home by the patients themselves, and it would be easy to determine whether TEAS worked. Thus, sham TEAS is not a suitable control and was not adopted in our trial. Second, patient compliance with TEAS treatment was recorded by patients. The investigator could not recognize patients with poor compliance in a timely manner and could not then prompt them to complete the predesigned 48 sessions. Real-time viewing of the actual treatment sessions through the TEAS software may help to accurately record and improve the patient’s treatment compliance. Third, lifestyle modification regarding physical exercise and weight loss was not implemented well due to home quarantine induced by COVID-19. Fourth, heart rate should be added as a secondary outcome. Finally, this is a pilot study carried out in only one center, and the generalizability of the results is uncertain.
In conclusion, this randomized clinical pilot trial provided evidence that home-based TEAS as adjunctive therapy may reduce systolic blood pressure in patients with hypertension compared with the effects of usual care. Further larger randomized controlled trials with a tool that can view actual treatment sessions in real time are warranted to confirm the effectiveness of home-based TEAS for hypertension in real-world circumstances.
References
Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Prospective studies collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–13.
World Health Organize. Hypertension [EB/OL]. https://www.who.int/health-topics/hypertension/, 2021-2-5.
Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–60.
Writing Group Members, Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, et al. Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2016 Update: A Report From the American Heart Association. Circulation. 2016;133:e38–360.
Guidelines for the prevention and treatment of hypertension in China (Revised edition in 2018). Chinese Journal of Cardiovascular Medicine [in Chinese] 2019;24:24-56.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–104.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: a Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2018;138:e484–484e594.
Yoon SS, Gu Q, Nwankwo T, Wright JD, Hong Y, Burt V. Trends in blood pressure among adults with hypertension: United States, 2003 to 2012. Hypertension. 2015;65:54–61.
Zhao L, Li D, Zheng H, Chang X, Cui J, Wang R, et al. Acupuncture as adjunctive therapy for chronic stable angina: a randomized clinical trial. JAMA Intern Med. 2019;179:1388–97.
Kristen AV, Schuhmacher B, Strych K, Lossnitzer D, Friederich HC, Hilbel T, et al. Acupuncture improves exercise tolerance of patients with heart failure: a placebo-controlled pilot study. Heart. 2010;96:1396–400.
Flachskampf FA, Gallasch J, Gefeller O, Gan J, Mao J, Pfahlberg AB, et al. Randomized trial of acupuncture to lower blood pressure. Circulation. 2007;115:3121–9.
Zheng H, Li J, Li Y, Zhao L, Wu X, Chen J, et al. Acupuncture for patients with mild hypertension: A randomized controlled trial. J Clin Hypertens. 2019;21:412–20.
Yang J, Chen J, Yang M, Yu S, Ying L, Liu GJ, et al. Acupuncture for hypertension. Cochrane Database Syst Rev. 2018;11:CD008821.
Tian ZX, Liu CZ, Qi YS, Tu JF, Lin Y, Wang Y, et al. Transcutaneous electrical acupoint stimulation for stage 1 hypertension: protocol for a randomized controlled pilot trial. Trials. 2020;21:558.
Liu HH, Wang YY, Gao HB, Chen YR, Yang JS, Lv AP. Acupoint selection rule of acupuncture and moxibustion for hypertension: a systematic review. J Traditional Chin Med. 2014;55:1055–8. [in Chinese]
Climie RE, Schultz MG, Nikolic SB, Ahuja KD, Fell JW, Sharman JE. Validity and reliability of central blood pressure estimated by upper arm oscillometric cuff pressure. Am J Hypertens. 2012;25:414–20.
Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2014). Hypertens Res. 2014;37:253–390.
Hallal PC, Victora CG. Reliability and validity of the International Physical Activity Questionnaire (IPAQ). Med Sci Sports Exerc. 2004;36:556.
Wan E, Yu E, Chin WY, Choi E, Wu T, Lam C. Evaluation of the responsiveness of Short Form-12 Health Survey version 2 (SF-12v2) in Chinese patients with hypertension in primary care. Qual Life Res. 2019;28:2851–7.
Sim J, Lewis M. The size of a pilot study for a clinical trial should be calculated in relation to considerations of precision and efficiency. J Clin Epidemiol. 2012;65:301–8.
Staessen JA, Wang JG, Thijs L. Cardiovascular protection and blood pressure reduction: a meta-analysis. Lancet. 2001;358:1305–15.
Sanderson JE, Tomlinson B, Lau MS, So KW, Cheung AH, Critchley JA, et al. The effect of transcutaneous electrical nerve stimulation (TENS) on autonomic cardiovascular reflexes. Clin Auton Res. 1995;5:81–4.
Chen H, Shen FE, Tan XD, Jiang WB, Gu YH. Efficacy and safety of acupuncture for essential hypertension: a meta-analysis. Med Sci Monit. 2018;24:2946–69.
Food and Drug Administration. Principles for clinical evaluation of new antihypertensive drugs [EB/OL]. https://www.fda.gov/media/71363/download, 2021-2-5.
Jung H, Yeo S, Lim S. Effects of acupuncture on cardiovascular risks in patients with hypertension: a Korean cohort study. Acupunct Med. 2020;39:964528420920290–125.
do Amaral Sartori S, Stein C, Coronel CC, Macagnan FE, Plentz R. Effects of transcutaneous electrical nerve stimulation in autonomic nervous system of hypertensive patients: a randomized controlled. Trial Curr Hypertens Rev. 2018;14:66–71.
Mannheimer C, Emanuelsson H, Waagstein F. The effect of transcutaneous electrical nerve stimulation (TENS) on catecholamine metabolism during pacing-induced angina pectoris and the influence of naloxone. Pain. 1990;41:27–34.
Wang XR, Yang JW, Ji CS, Zeng XH, Shi GX, Fisher M, et al. Inhibition of NADPH oxidase-dependent oxidative stress in the rostral ventrolateral medulla mediates the antihypertensive effects of acupuncture in spontaneously hypertensive rats. Hypertension. 2018;71:356–65.
Funding
The study was funded by the National Key R&D Program of China (2019YFC1712102) and the Distinguished Young Scholars Project of Beijing University of Chinese Medicine (BUCM-2019-JCRC011).
Data sharing statementIndividual anonymous participant data will be shared with researchers whose proposed use of the data has been approved. For inquiries about data sharing, please send requests at https://www.lcz623780@126.com.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Tu, JF., Wang, LQ., Liu, JH. et al. Home-based transcutaneous electrical acupoint stimulation for hypertension: a randomized controlled pilot trial. Hypertens Res 44, 1300–1306 (2021). https://doi.org/10.1038/s41440-021-00702-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-021-00702-5