Abstract
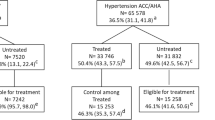
The 2017 American College of Cardiology/American Heart Association Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults reduced the systolic/diastolic blood pressure thresholds to define hypertension, including recommendations about treatment initiations and goals. We estimated the age-stratified prevalence, treatment status, and factors associated with hypertension among US adults aged ≥ 20 years based on this guideline. This cross-sectional study used the 2011–2016 National Health and Nutrition Examination Survey data. The primary outcomes were the presence and treatment status of hypertension. Among 16,103 participants, the proportions (95% confidence interval) of hypertensive, treatment-indicated, untreated individuals among treatment-indicated, and treatment goals not met among treated for hypertension by age groups were, respectively, 17.4% (15.8–19.1), 6.9% (6.1–7.8), 67.6% (61.0–73.5), and 58.6% (46.1–70.2) among 20–34 years; 39.2% (37.0–41.5), 24.4% (22.4–26.5), 41.8% (37.7–46.0), and 50.4% (44.7–56.1) among 35–49 years; 62.3% (60.1–64.6), 51.4% (49.0–53.8), 31.0% (28.2–34.0), and 51.9% (47.6–56.1) among 50–64 years; 77.7% (75.3–79.8), 77.0% (74.7–79.2), 27.0% (24.3–29.8), and 63.1% (59.4–66.5) among ≥ 65 years; and 46.8% (45.4–48.3), 36.9% (35.4–38.5), 33.2% (30.9–35.5), and 56.7% (54.1–59.3) among overall population. Despite some dissimilarities, the prevalence, treatment eligibility, and odds of hypertension were higher among non-Hispanic blacks and among people with high cholesterol, low high-density lipoprotein, chronic kidney disease, diabetes, increased body weight, and low leisure-time physical activity in all age strata. The prevalence and treatment eligibility were high among adults from all age groups; however, a significant proportion of participants, especially those who were younger, had blood pressure levels above the treatment goals or were untreated. Addressing the associated characteristics from a younger age may help prevent the complications of hypertension.
Similar content being viewed by others
Introduction
Cardiovascular disease (CVD) is one of the leading causes of death in the United States [1], and uncontrolled hypertension is the primary risk factor for CVD [2,3,4]. As per the ‘2017 American College of Cardiology/American Health Association (ACC/AHA) Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults’ prevalence estimate by Muntner et al., more than 45% of US adults (aged ≥ 20 years) could be hypertensive [5]. Lowering the systolic/diastolic blood pressure (SBP/DBP) cutoffs from ≥140/90 mm Hg to ≥130/80 mm Hg has changed the prevalence from previous estimates [5, 6]. Furthermore, the new guideline has modified the recommendations and goals of treatment [6]. The estimated proportion of people with unmet treatment goals has also been found to be high among treated people [5].
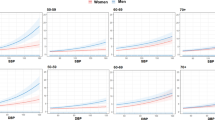
The prevalence, treatment indications, and risks of hypertension vary according to sociodemographic and behavioral characteristics. Age is an established risk factor for hypertension; older people usually have a higher likelihood of developing hypertension [5, 6] due to the changes in blood vessel walls that occur with aging [7]. For instance, Muntner et al. found the prevalence of hypertension as 24.0, 47.1, 66.6, 75.6, and 82.3% among people aged 20–44, 45–54, 55–64, 65–74, and ≥75 years, respectively [5]. Awareness and control levels also differ with age. In addition, prevalence, awareness, treatment, and control could differ by sex, race, body mass index (BMI), and other comorbidities [5, 6, 8, 9].
The application of the 2017 ACC/AHA guideline could significantly reduce the burden of future CVD events [6, 10, 11]. Stratifying the prevalence, treatment patterns, and associated factors of hypertension by age could help formulate age-specific prevention strategies if these factors differ between age groups. Although earlier studies have investigated the awareness [12] and control [9] of hypertension according to the new guideline in terms of the overall prevalence [5, 6, 8], the age-stratified prevalence of hypertension and the prevalence of pharmacotherapy-indicated, and untreated hypertensive individuals were not estimated. Furthermore, the risk factors for hypertension were not stratified by age. Considering the significant changes in prevalence between individuals of varying age categories following the adoption of the new guideline [5, 6, 8], the factors associated with hypertension in these groups may differ compared with those in the overall population. Due to the clinical and public health significance of hypertension, these estimates would be helpful for prevention, treatment, and control purposes.
Using the 2017 ACC/AHA guideline, this study attempted to identify and fill these existing gaps in the literature by obtaining the following age-stratified and overall estimates according to sociodemographic and clinical characteristics among US adults: the prevalence of hypertension; the proportion of people eligible for antihypertensive treatment; the proportion of untreated individuals among treatment-eligible individuals; and the proportion of individuals with unmet treatment goals among treated (i.e., taking antihypertensive medication) persons. In addition, age-stratified factors associated with hypertension were determined.
Methods
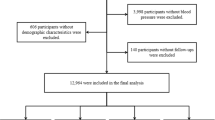
Data source
The present study utilized data from the 2011–2016 National Health and Nutrition Examination Survey (NHANES). This biennial cross-sectional survey aims to obtain nationally representative samples of noninstitutionalized US people using a multistage cluster-sampling design. Details of the NHANES, including the survey design, methodologies, and datasets are available elsewhere [13,14,15,16]. Datasets were downloaded and merged according to the identification numbers. All respondents provided written informed consent. The Ethics Review Board of the National Center for Health Statistics Research approved the protocols [17].
Blood pressure
Respondents aged ≥ 20 years with ≥ 3 BP measurements were eligible for analysis. The mean of the first three measurements was used to categorize BP. Trained physicians used factory-calibrated Baumanometer® mercury true gravity wall model sphygmomanometers with appropriate cuff sizes to measure BP while the participants were seated in mobile examination centers. Before the measurements, participants remained in a seated position for 5 min [18].
Individuals with SBP/DBP ≥130/80 mm Hg or who currently reported taking antihypertensive drugs were considered hypertensive. Stage 1 and stage 2 hypertension were defined as SBP/DBP 130–139/80–89 and ≥140/90 mm Hg, respectively, while elevated BP was considered when the SBP was 120–129 mm Hg with a normal DBP (i.e., < 80 mm Hg) [6].
Study variables
Participants reported their age (in years), gender (i.e., male or female), and race. Due to different treatment indications and goals, individuals with ≥ 65 years of age were considered as a separate stratum. Other age groups were stratified into three approximately equal-sized strata: 20–34, 35–49, and 50–64 years.
Cholesterol levels from 200–239 and ≥240 mg/dl were stratified into ‘borderline elevated’ and ‘high’ cholesterol levels, respectively. Participants who reported taking cholesterol-lowering drugs were also grouped in the high-cholesterol group. High-density lipoprotein (HDL) cholesterol levels were categorized as low if the concentration was < 40 mg/dl for men and < 50 mg/dl for women. Participants reported if they were ever diagnosed with prediabetes or diabetes by a physician. The glomerular filtration rate (GFR) was obtained using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation. Persons with an albumin-creatinine ratio ≥ 30 mg/g or a GFR < 60 ml/min per 1.73 m2 were categorized as having CKD [19].
Myocardial infarction, coronary heart disease, stroke, or heart failure was considered as CVD events. The 10-year predicted CVD risk was calculated with Pooled Cohort Risk equations among people without a history of CVD events [20]. Although the Pooled Cohort Risk equations are recommended to calculate CVD risk for individuals aged 40–79 years, to conform to the 2017 ACC/AHA guideline, these equations were used for all age groups in this study because the equations were the only currently available tools [5, 20]. A person was considered to have high CVD risk if s/he had a history of CVD or had a ≥10% 10-year CVD risk [5, 6].
The BMI was calculated as ‘weight in kilograms’ divided by ‘height in meters squared’ and was categorized as underweight/normal weight (i.e.,<25 kg/m2), overweight (i.e., 25–29.9 kg/m2), and obese (i.e., ≥30 kg/m2). In NHANES, the family income to poverty ratio is determined from the ratio of the family’s income to the poverty thresholds according to the number of family members. A higher ratio indicates that the participant is from a wealthier family. This ratio was categorized into ‘< 2’ and ‘≥ 2’ [9, 21]. Participants reported the usual amount of time they spent doing moderate and vigorous recreational physical activity (PA) in a week. Minutes spent performing vigorous PA were multiplied by 2, and this number was added to the minutes of moderate PA to calculate leisure-time PA (LTPA). LTPA was stratified into none (i.e., 0 min/week), low (i.e., >0 to <150 min/week), and high (i.e., ≥150 min/weeks) [9].
Persons with the following characteristics were considered to have an indication (i.e., treatment-eligible) for pharmacotherapy: stage 2 hypertension; stage 1 hypertension with diabetes, CKD, or high CVD risk; and SBP ≥130 mmHg with ≥65 years of age. Unmet treatment goals were considered when the SBP/DBP was ≥130/80 mmHg if the age was <65 years or when the SBP was ≥130 mmHg if the age was ≥65 years among individuals currently taking antihypertensive medications [5, 6].
Based on the published literature, biologic plausibility, and data structure, the following potential factors were selected for investigation: age (only for the overall population), sex, race, cholesterol, HDL cholesterol, body weight, CKD, diabetes, LTPA, and family income to poverty ratio (Supplementary Table 1).
Statistical analysis
The background characteristics of the respondents were reported according to age. Continuous variables were described by mean and standard error (SE). Unweighted numbers and weighted percentages were used to report categorical variables. The prevalence (with 95% confidence interval [CI]) of hypertension was determined according to the background characteristics of all age groups. The proportion of persons with indications for pharmacotherapy was estimated. Then, among treatment-indicated persons, untreated persons (i.e., persons who were not receiving pharmacotherapy despite being eligible for treatment) were reported separately. Furthermore, among the people who reported that they were currently taking antihypertensive drugs, the proportion of persons who were not meeting the treatment goals was estimated. Logistic regression analysis was then conducted to obtain crude odd ratios (CORs). Variables with predetermined significance levels (p < 0.2) from the CORs (Supplementary Table 1) were included in the multivariable models to obtain adjusted ORs (AORs) [22]. Adjusted models were created for all age strata and the overall study population. AORs were presented with 95% CIs and p-values. The proportion of missing data was low (Supplementary Table 2). The multistage cluster-sampling design was used to report the weighted proportions and ORs; the sample weights from the mobile examination centers were used to obtain all the estimates. Stata 14.0 (College Station, Texas, USA) was used to analyze the data [23].
Results
Table 1 describes the background characteristics of the hypertensive participants and the overall study population. The analysis included 16,103 individuals (7811 men and 8292 women) representing 223,364,258 US adults. The mean SBP, DBP, and age of the participants were 124.2 mm Hg (SE: 0.1), 70.5 mm Hg (SE: 0.1), and 49.5 years (SE: 0.1), respectively. The proportion of men and women participants was roughly equal in the overall study population; however, the proportion of females in the group of hypertensive participants increased with age. About two-thirds of the participants were non-Hispanic whites (65.6%) followed by other races/ethnicities (14.5%), non-Hispanic blacks (11.4%), and Mexican-Americans (8.5%). Among the hypertensive subjects, the proportion of individuals with high cholesterol, CKD, diabetes, and high CVD risk increased gradually with age. In contrast, the proportion of people with low HDL-cholesterol levels, obesity, and high LTPA decreased gradually among hypertensive individuals with increasing age. Approximately 63.0% of the overall people were from the top wealth category (i.e., family income to poverty ratio ≥2).
The overall prevalence (95% CI) of hypertension was 46.8% (45.4–48.3). The prevalence of hypertension was 17.4% (15.8–19.1), 39.2% (37.0–41.5), 62.3% (60.1–64.6), and 77.7% (75.3–79.8) among people with 20–34, 35–49, 50–64, and ≥ 65 years of age, respectively (Table 2). The prevalence increased with age regardless of characteristics. Among the races, non-Hispanic blacks had the highest prevalence of hypertension in all age groups. For individuals in the 20–34, 35–49, 50–64, and ≥65 year age groups, the prevalence (95% CI) of hypertension was 24.0% (21.5–26.6), 44.5% (41.2–47.9), 65.2% (61.9–68.3), and 74.5% (70.6–78.1) in men and 10.8% (9.0–12.8), 34.3% (31.7–36.9), 59.7% (55.9–63.4), and 80.1% (77.5–82.4) in women, respectively. People with high cholesterol levels, low HDL-cholesterol levels, CKD, and no LTPA had the highest prevalence of hypertension in all age groups; however, the differences within subcategories of many of these characteristics declined with increasing age. Although the prevalence of stage 1 hypertension was similar across age groups, the prevalence of stage 2 hypertension increased progressively with age. More than one-third of people aged 50–64 years were taking BP-lowering drugs, and more than half of those aged 65 years or older were taking BP-lowering drugs, 35.4% (95% CI: 33.0–37.9) and 56.2% (95% CI: 53.4–59.0), respectively. The prevalence (95% CI) of treated individuals who did not meet their treatment goals was 58.6% (46.1–70.2), 50.4% (44.7–56.1), 51.9% (47.6–56.1), 63.1% (59.4–66.5), and 56.7 (54.1–59.3) among people with 20–34, 35–49, 50–64, ≥ 65 years of age, and the overall population, respectively.
The proportion (95% CI) of treatment-eligible individuals was 6.9% (6.1–7.8), 24.4% (22.4–26.5), 51.4% (49.0–53.8), and 77.0% (74.7–79.2) among people 20–34, 35–49, 50–64, and ≥ 65 years of age, respectively (Table 3). The characteristics that were associated with a higher prevalence of hypertension (e.g., non-Hispanic black race, high cholesterol, CKD, diabetes, or high CVD risk) were also associated with an increased indication of antihypertensive treatment.
The percentage (95% CI) of people who had an indication for pharmacotherapy but remained untreated was 67.6% (61.0–73.5), 41.8% (37.7–46.0), 31.0% (28.2–34.0), and 27.0% (24.3–29.8) among 20–34, 35–49, 50–64, and ≥ 65-year-old people, respectively (Table 4). In all age groups, a greater proportion of males were untreated compared to females. Although the proportion of untreated individuals decreased with age, these proportions remained substantially high regardless of characteristics. Even with a high CVD risk, approximately one-third of the people were untreated, 30.0% (95% CI: 28.0–32.2).
Table 5 shows the proportion of individuals who were not meeting the treatment goals despite taking medicine. Regardless of characteristics or age, more than half of the individuals had unmet treatment goals, 56.7% (95% CI: 54.2–59.3). Although males had higher unmet goals before the age of 65 years, the proportion was higher among females after that age: 67.3% (95%: 62.4–71.8) and 57.0% (95% CI: 52.9–60.9), respectively. Non-Hispanic blacks had the highest proportion of people with unmet needs in all age strata. Despite the higher prevalence of hypertension among people with elevated cholesterol levels, low HDL, and CKD, these groups had a lower proportion of people with unmet treatment goals. Excluding the youngest (i.e., 20–34 years) age group, people with higher CVD risk had a greater proportion of people with unmet goals. Figure 1 summarizes all four studied proportions according to age. With an overall awareness of 63.7% (95% CI: 61.9–65.6), approximately 31.0% (95% CI: 27.6–34.6), 52.7% (95% CI: 48.9–56.5), 67.3% (95% CI: 64.7–69.8), and 78.0% (95% CI: 75.4–80.4) of people in the 20–34, 35–49, 50–64, and ≥ 65 years of age groups did not meet their treatment goals, respectively (Supplementary Table 3). Some of the characteristics had low awareness levels in all age groups.
Prevalence of individuals with hypertension, individuals who are eligible for hypertension treatment, individuals who are untreated among the treatment-eligible group, and individuals with unmet treatment goals among the participants who reported taking antihypertensive medication by age, National Health and Nutrition Examination Survey 2011–2016
In the crude analysis, most of the factors were significantly associated with hypertension in all age groups, including in the overall population (Supplementary Table 1). As Table 6 shows, the odds of hypertension increased progressively with age for the overall population. The highest AOR was 10.7 (95% CI: 9.0–12.8) among people with ≥ 65 years of age. The overall AOR of hypertension was lower among women, 0.6 (95% CI: 0.6–0.7) compared with men. While the odds of hypertension were lower for women aged < 65 years, the AOR of hypertension was higher for women aged ≥65 years, 1.3 (95% CI: 1.0–1.7). In all age strata, non-Hispanic blacks had higher odds of hypertension than non-Hispanic whites. Although borderline elevated cholesterol was a significant factor in the youngest age group and the overall population, it was not associated with hypertension in all age groups. Moreover, a low HDL-cholesterol level was associated with a higher odds of hypertension only among the 20–34 years age group (AOR: 1.4, 95% CI: 1.2–1.7). Diabetes, CKD, and elevated BMI were associated with higher odds of hypertension in all age groups. Higher LTPA (i.e., ≥150 min) was associated with lower odds of hypertension. Although a high family income to poverty ratio was associated with lower odds of hypertension among people aged ≥65 years, it was not significant in other age groups or the overall population.
Discussion
Using a large nationally representative sample, this study stratified prevalence, treatment status, and associated factors of hypertension among US adults according to age based on the application of the 2017 ACC/AHA guideline. After stratification, the findings indicate that roughly ‘1 in 5’, ‘2 in 5’, ‘3 in 5’, and ‘4 in 5’ adults in the 20–34, 35–49, 50–64, and ≥65 year age groups, including approximately half of the overall population, could have hypertension. A substantial proportion of these individuals could either have an indication for pharmacotherapy but not be taking medication or be receiving treatment but not meeting treatment goals. Sex, race, high cholesterol, low HDL, CKD, diabetes, and LTPA were associated with higher prevalence, treatment indication, and odds of hypertension. These are known risk factors for hypertension [5, 6, 8, 9]. This study reconfirmed the significance of these known factors after stratifying by age.
The prevalence of hypertension observed in this study is in agreement with the past research by Muntner et al. that also estimated the prevalence in the same age ranges using the 2011–2014 NHANES datasets [5]. Unlike prior studies, this study reported the proportion of individuals who require pharmacotherapy, have higher CVD risks, were untreated despite having a treatment indication, and have unmet treatment goals, as well as associated factors according to age and among the overall population on a wide range of sociodemographic and clinical characteristics using the 2017 ACC/AHA guideline.
Similar to previous studies, in all age strata, non-Hispanic black individuals had a higher prevalence, treatment indication, and odds of hypertension than their non-Hispanic white counterparts [5, 10, 24, 25]. Although Mexican-American individuals had an overall lower prevalence of hypertension, including those in the age groups younger than 64 years, the prevalence was higher after that age. Africans living in Africa have a lower prevalence of hypertension than the global prevalence; however, African-Americans in the US consistently have a higher prevalence [26,27,28]. Despite similarities in genetic characteristics, the substantial socioeconomic differences between these two regions of the world could be responsible for this discrepancy [28]. The complications of hypertension are also more severe among African-Americans [10, 26]. Differences in awareness, lifestyle, and socioeconomic status between races could be responsible for this difference [9, 12]. Considering treatment status, a greater proportion of African-Americans than of individuals of other races were receiving treatment; however, the proportion of individuals not meeting treatment goals was also higher among African-Americans in all age strata.
Elevated BMI, diabetes, high cholesterol, low HDL, and CKD were significantly associated with hypertension. All of these conditions correlate with one another [29]. The complex mechanisms by which these factors interact are only partially understood and are beyond the scope of this discussion; nevertheless, preventing and treating these comorbid conditions could minimize future disease risks and complications not only from hypertension but also from the conditions themselves [10, 26, 28]. These comorbidities are also of clinical and public health significance, and the prevalence of these conditions increases with increasing age [6, 29].
Although the proportion of individuals who require pharmacotherapy or who were taking antihypertensive medication increased along with the overall prevalence, a substantial proportion of these individuals remained untreated or were not meeting the treatment goals. Young adults (i.e., ages 20–34 years) need more awareness and preventive and treatment measures considering that they had the highest proportion of untreated individuals or people with less awareness (Supplementary Table 3). Even among the treated individuals, a large proportion did not meet their treatment goals. Young adults also had slightly different correlates than other people. In addition to the 17.4% prevalence of hypertension in the youngest age group, ~15% of them also had elevated BP (i.e., SBP: 120–129 mmHg), which was the highest of all the age groups. Hypertension and other correlated conditions are more likely to develop in later stages of life if preventive measures are not taken. At least, preventive measures may slow down the progression to hypertension and other associated conditions [6].
It is recommended that all individuals with hypertension or elevated BP adhere to lifestyle and dietary recommendations, regardless of CVD risk [5, 6]. Overall, a higher level of LTPA had an inverse association with hypertension. Among hypertensive subjects from each age stratum, a small proportion of people was engaged in ≥150 min of LTPA and that proportion declined with age (Table 1). Increasing LTPA is also essential for the prevention of the aforementioned conditions, including overweight/obesity, dyslipidemia, and diabetes [9, 27, 28, 30]. In addition to lifestyle measures, maintaining ideal BP levels using pharmacotherapy among treatment-indicated people is especially important for reducing CVD, kidney, and other disease burdens. Those who are untreated or have unmet treatment goals with characteristics such as CKD or high CVD risks are more vulnerable to the adverse consequences of hypertension. Connecting treatment-indicated hypertensive people to the proper therapy is essential [6, 10, 11]. Furthermore, if the participants of the current study ever received an evaluation, were treated and evaluated according to prior guidelines that differ from the 2017 ACC/AHA guideline [6, 31]. Therefore, reevaluating and regularly monitoring the BP of treated individuals to ensure that they are being treated appropriately is important.
The strengths of the study include the generalizability of the results as NHANES yields large nationally representative samples that allow for adequate subgroup analysis. NHANES follows standardized validated protocols. The proportions were obtained after applying sample weights with appropriate statistical procedures.
Limitations
Although the 2017 ACC/AHA recommends measuring BP on multiple occasions, NHANES measures BP on a single day [5, 6]; some hypertensive subjects could have white coat hypertension [32, 33]. Furthermore, due to the cross-sectional nature of the datasets, the observed associations may not be causal. However, all these characteristics were confirmed by earlier cohort studies [6]. As the study participants (NHANES 2011–2016) were evaluated or treated based on previous guidelines, calculating the prevalence of people with unmet treatment goals or people who are untreated despite treatment eligibility may cause some overestimation.
Conclusion
Implementing the new guideline revealed that a large proportion of US adults across all age groups were hypertensive and at risk for complications resulting from hypertension. The adoption of preventive lifestyle and dietary measures from a young age may prevent and reduce the burden of hypertension and other correlated conditions. Ensuring adequate treatment from a younger age is also important because a large proportion of the individuals in this study were untreated despite being eligible or were not meeting their treatment goals. Addressing characteristics associated with a higher prevalence of hypertension and ensuring adequate treatment for people with indications for pharmacotherapy, particularly from a younger age, are essential. Regardless of age, reevaluation and regular BP monitoring of individuals with unmet treatment goals or who are being treated with pharmacotherapy are important.
Data availability
The datasets are publicly available at the Centers for Disease Control and Prevention’s website. Dr. Kibria has full access to the data and takes responsibility for theintegrity of the data analysis.
References
Heron M. National Vital Statistics Reports National Center for Health Statistics. Annual. Hyattsville, MD. 2018. https://www.cdc.gov/nchs/data/nvsr/nvsr67/nvsr67_06.pdf. Accessed 5 Dec 2018.
Forouzanfar MH, Liu P, Roth GA, Ng M, Biryukov S, Marczak L, et al. Global Burden of Hypertension and Systolic Blood Pressure of at Least 110 to 115 mm Hg, 1990–2015. JAMA. 2017;317:165–82.
GBD 2015 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1603–58.
GBD 2016 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1260–344.
Muntner P, Carey RM, Gidding S, Jones DW, Taler SJ, Wright JT, et al. Potential U.S. Population Impact of the 2017 American College of Cardiology/American Heart Association High Blood Pressure Guideline. Circulation. 2017;109–18. https://doi.org/10.1161/CIRCULATIONAHA.117.032582.
Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2017; HYP.0000000000000065.
Celermajer DS, Sorensen KE, Spiegelhalter DJ, Georgakopoulos D, Robinson J, Deanfield JE. Aging is associated with endothelial dysfunction in healthy men years before the age-related decline in women. J Am Coll Cardiol. 1994;24:471–6.
Dorans KS, Mills KT, Liu Y, He J. Trends in Prevalence and Control of Hypertension According to the 2017 American College of Cardiology/American Heart Association (ACC/AHA) Guideline. J Am Heart Assoc. 2018;7:e008888.
Ostchega Y, Zhang G, Hughes JP, Nwankwo T. Factors associated with hypertension control in US adults using 2017 ACC/AHA Guidelines: National Health and Nutrition Examination Survey 1999–2016. Am J Hypertens. 2018;31:886–94.
Yano Y, Reis JP, Colangelo LA, Shimbo D, Viera AJ, Allen NB, et al. Association of blood pressure classification in young adults using the 2017 American College of Cardiology/American Heart Association blood pressure guideline with cardiovascular events later in life. JAMA. 2018;320:1774.
Bundy JD, Mills KT, Chen J, Li C, Greenland P, He J. Estimating the association of the 2017 and 2014 hypertension guidelines with cardiovascular events and deaths in US adults: an analysis of national data. JAMA Cardiol. 2018;3:572.
Park S, Gillespie C, Baumgardner J, Yang Q, Valderrama AL, Fang J, et al. Modeled state-level estimates of hypertension prevalence and undiagnosed hypertension among US adults during 2013–2015. J Clin Hypertens. 2018;20:1395–410.
Borrud L, Chiappa MM, Burt Vi.L., Gahche J, Zipf G, Dohrmann SM, et al. National Health and Nutrition Examination Survey: National Youth Fitness Survey Plan, operations, and analysis, 2012. 2012. https://www.cdc.gov/nchs/data/series/sr_02/sr02_163.pdf. Accessed 27 Aug 2018.
Curtin LR, Mohadjer LK, Dohrmann SM, Kruszon-Moran D, Mirel LB, Carroll MD, et al. National Health and Nutrition Examination Survey: sample design, 2007–2010. 2013. https://www.cdc.gov/nchs/data/series/sr_02/sr02_160.pdf.
Johnson C, Burt ViL, Mohadjer LK. National Health and Nutrition Examination Survey: sample design, 2011–2014. 2014. https://www.cdc.gov/nchs/data/series/sr_02/sr02_162.pdf.
Zipf G, Chiappa M, Porter KS, Ostchega Y, Lewis BG, Dostal J. National health and nutrition examination survey: plan and operations, 1999–2010. Vital- Health Stat. 2013;1:1–37.
National Center for Health Statistics. NCHS Research Ethics Review Board (ERB) approval. 2017. https://www.cdc.gov/nchs/nhanes/irba98.htm. Accessed 11 Sep 2018.
National Health and Nutrition Examination Survey Data Documentation. https://wwwn.cdc.gov/Nchs/Nhanes/2013-2014/BPX_H.htm#Eligible_Sample.
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–12.
Goff DC, Lloyd-Jones DM, Bennett G, Coady S, D’Agostino RB, Gibbons R, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25 Pt B):2935–59.
U.S. Department of Health & Human Services. Poverty Guidelines [WWW Document]. 2019. https://aspe.hhs.gov/poverty-guidelines. Accessed 16 Feb 2019.
Maldonado G, Greenland S. Simulation study of confounder-selection strategies. Am J Epidemiol. 1993;138:923–36.
Stata Corporation, College Station, Texas, USA. Stata 14.0. 2015.
Al Kibria GM. Racial/ethnic disparities in prevalence, treatment and control of hypertension among US adults following application of the 2017 American College of Cardiology/American Heart Association guideline. Preventive Medicine Reports. 2019;100850.
Al Kibria GM, Swasey K, Sharmeen A, Day B. Estimated change in prevalence and trends of childhood blood pressure levels in the United States after application of the 2017 AAP guideline. Prev Chronic Dis. 2019;16:180528.
Gudmundsdottir H, Høieggen A, Stenehjem A, Waldum B, Os I. Hypertension in women: latest findings and clinical implications. Ther Adv Chronic Dis. 2012;3:137–46.
Papadakis MA. Current medical diagnosis and treatment. McGraw-Hill Education/Medical; 2016.
Davidson’s principles and practice of medicine. s.l.: Elsevier; 2018.
Riaz H, Khan MS, Siddiqi TJ, Usman MS, Shah N, Goyal A, et al. Association between obesity and cardiovascular outcomes: a systematic review and meta-analysis of mendelian randomization studies. JAMA Netw Open. 2018;1:e183788.
Roger VL, Go AS, Lloyd-Jones DM, Adams RJ, Berry JD, Brown TM, et al. Heart disease and stroke statistics—2011 update: a report from the American Heart Association. Circulation. 2011;123:e18–209.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–72.
Sorof JM, Portman RJ. White coat hypertension in children with elevated casual blood pressure. J Pedia. 2000;137:493–7.
Sharma AK, Metzger DL, Rodd CJ. Prevalence and severity of high blood pressure among children based on the 2017 American Academy of Pediatrics Guidelines. JAMA Pediatr. 2018;172:557.
Acknowledgements
The authors are thankful to the survey participants and staff for their relentless efforts to obtain the NHANES data.
Author information
Authors and Affiliations
Contributions
Conceptualization: Gulam Kibria; formal analysis: Gulam Kibria; writing—original draft preparation: Gulam Kibria, Brendan Day, and Atia Sharmeen; writing—review and editing: Amy Nemirovsky and Brendan Day.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Al Kibria, G.M., Nemirovsky, A., Sharmeen, A. et al. Age-stratified prevalence, treatment status, and associated factors of hypertension among US adults following application of the 2017 ACC/AHA guideline. Hypertens Res 42, 1631–1643 (2019). https://doi.org/10.1038/s41440-019-0275-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-019-0275-x