Abstract
The sympathoinhibitory mechanism of azilsartan was investigated in an adenine-induced chronic renal failure model. Azilsartan exerted an antihypertensive effect, though BP elevation induced by adenine was marginal. The creatinine value was significantly lower in the azilsartan group (AZ) than in the vehicle group (VEH); furthermore, proteinuria was suppressed, and sodium excretion was augmented in the AZ group. The low frequency (LF) of systolic BP was suppressed (VEH: 4.07 ± 2.67 mmHg2 vs. AZ: 3.32 ± 1.93 mmHg2 P < 0.001), and the spontaneous baroreflex gain (sBRG) was augmented (VEH: 1.04 ± 0.62ms/mmHg vs. AZ: 1.38 ± 0.69 ms/mmHg, P < 0.001) in AZ. There were no significant differences in ACE1 and ACE2 expression between the groups, which indicated that the action of azilsartan on these components of the intrarenal renin–angiotensin–aldosterone system was comparatively small. Although NHE3, NKCC, and ENaC expression was similar between the groups, NaCl cotransporter (NCC) expression was markedly suppressed by azilsartan (P < 0.05). Thus, in a mild chronic kidney disease (CKD) model with slight BP elevation, the sympatholytic effect of ARB might be expected, and azilsartan might exert its natriuretic effect by NCC suppression achieved by sympathoinhibitory activity.
Similar content being viewed by others
Introduction
Chronic kidney disease (CKD) is one of the most important health issues worldwide. CKD not only progresses to end-stage renal disease (ESRD) [1] but also becomes a risk factor for cardiovascular disease (CVD) beginning in the early stage [2,3,4]. Hence, intervention or treatment from the early stage of CKD is very important for preventing CVD. Hypertension is a major comorbidity in CKD and has been demonstrated to be a significant risk factor for the development of ESRD; inadequate blood pressure management leads to an early decline in kidney function [4].
Sympathetic nervous system overactivity is an important feature among CKD patients. Muscle sympathetic nerve activity (MSNA) was found to be inversely correlated with the estimated glomerular filtration rate (GFR), and this change in MSNA starts in the early stage of CKD [5]. In CKD patients, increasing MSNA has been proven to be related to all-cause mortality and nonfatal cardiovascular events, independent of GFR and blood pressure [6]. Hence, sympathetic nervous system overactivity may be associated with kidney function deterioration independent of blood pressure.
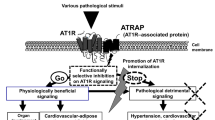
Angiotensin II receptor blockers (ARBs) are proposed to be key drugs in the management of high blood pressure in CKD [7] because they inhibit the progression of ESRD [8]. This beneficial effect is partly independent of their blood pressure-lowering effect [9]. Although the beneficial effect obtained by ARB administration is proposed to be mainly due to the strong antihypertensive effect and reduction in glomerular capillary pressure [10], it is established that ARBs also exert sympatholytic effects in obesity models with sympathetic nervous system overactivity [11]. Although sympathetic nervous system overactivity is an important feature of CKD, this sympatholytic effect of ARBs has not yet been shown to be exerted in CKD patients. Furthermore, we are not certain whether we should use ARBs for renal protection in patients who have established CKD without elevation of blood pressure, since it has been shown that lowering blood pressure below a certain threshold may be rather deleterious in diabetic nephropathy [12].
The adenine-induced chronic renal failure model, one of the models of renal failure, is produced by the mechanism of 2,8-dihydroxyadenine, a metabolic product of adenine that is crystallized in tubular fluid, where it causes tubular obstruction and chronic tubulointerstitial injury [13]. The effect on the hemodynamic status in the glomerulus in this model is expected to be relatively minimal.
Therefore, to clarify the renal protective effects of ARBs, such as natriuresis, that are independent of blood pressure and renal microcirculation, these effects were investigated in an adenine-induced chronic renal failure model, a CKD model with mild blood pressure elevation.
Methods
This study was performed in accordance with the National Institutes of Health guidelines for the use of experimental animals. All animal studies were approved by the Animal Studies Committee of The Jikei University School of Medicine.
Animal preparations
Nine-week-old male Wistar-Kyoto rats (Hoshino Laboratory Animals, Inc., Ibaraki, Japan) were cage-housed in a room with temperature maintained at 22–25 °C and a 12:12-h light–dark cycle, with free access to tap water and standard chow for 2 weeks. Thereafter (week 0), to produce renal failure, adenine was added at a concentration of 0.75% for 4 weeks. Next, a transmitter for monitoring arterial pressure, heart rate (HR), low frequency (LF) power of sBP, and spontaneous baroreceptor reflex gain (sBRG) was inserted. A telemetry system (Data Sciences International, St. Paul, MN, USA) was used as previously described [11, 14]. Briefly, the rats were anesthetized with isoflurane, an abdominal incision was made, and the abdominal aorta was isolated. The transmitter for monitoring arterial pressure (TA11PA-C40; Data Sciences International) was inserted into the abdominal aorta. One week after implantation, arterial pressure, HR, LF of sBP, and sBRG were measured as previously described (week 5) [11, 14, 15]. It has already been shown that LF power in the spectral density of systolic arterial pressure variability reflects vasomotor sympathetic tone [16]. The sBRG is calculated from spontaneous changes in systolic arterial pressure and the pulse interval as an index of time-dependent changes in baroreflex function, and it is used broadly as an index of autonomic nervous system activity [16]. In fact, the LF of sBP and sBRG are regarded as indices of sympathetic nervous system activity [11, 14].
The rats were assigned to three groups: group 1, sham group (n = 6); group 2, adenine-induced chronic renal failure rats (vehicle group (VEH)) (n = 23); and group 3, azilsartan to rats that underwent the same protocol as group 2 (azilsartan group (AZ)) (n = 26). The rats in the AZ group were administered azilsartan (Takeda Co., Ltd., Tokyo, Japan) 2 mg/kg/day orally in the morning [17] for 4 weeks. After administration of azilsartan (week 9), arterial pressure, LF of sBP, and sBRG were again monitored by telemetry. After the measurement at week 9, the animals were decapitated, and their kidneys were harvested for further analysis.
During the study, the rats were housed in metabolic cages, and urine was collected throughout each day (daytime; 12 h) and night (nighttime; 12 h) to measure urinary electrolytes, and protein (SRL, Inc. Tokyo, Japan) at week 0, week 5, and week 9. Blood samples were collected from the caudal vein of each rat to assess various clinical test items at the same time as urine collection at week 0, week 5, and week 9 (SRL, Inc. Japan).
Immunoblotting analysis
Renal cortical tissues were lysed in solubilization buffer. Immunoblotting was performed as described previously [18] using the following specific antibodies: rabbit polyclonal anti-angiotensin converting enzyme 2 (ACE2) antibody (Abcam, Cambridge, UK; ab15348), rabbit polyclonal anti-angiotensin converting enzyme 1 (ACE1) antibody (Abcam; ab28311), rabbit polyclonal anti-Na+/H+ exchanger 3 (NHE3) antibody (StressMarq Bioscience, Victoria, Canada; SPC-400), mouse monoclonal anti-Na+-K+-Cl- cotransporter (NKCC) 1/2 antibody (Millipore, CA, USA; MABS1237), rabbit polyclonal anti-thiazide sensitive NaCl cotransporter (NCC) antibody (Millipore; AB3553), and rabbit polyclonal anti-alpha epithelial Na+ channel (ENaC) antibody (StressMarq Bioscience; SPC-403). The bands were visualized using an ECL detection kit (Amersham Biosciences, Uppsala, Sweden). Images were quantified densitometrically using ImageJ [19].
Immunohistochemistry
Immunohistochemical analysis was performed using antibodies against ACE1 (Abcam) and ACE2 (Abcam). The area of staining of each protein in the glomeruli and tubules was measured using ImageJ, and the percentage of staining was calculated.
Statistical analysis
Data are expressed as the means ± standard deviation. The differences among the three groups were analyzed by analysis of variance (ANOVA) with the post hoc Steel-Dwass test. The differences in time course were analyzed by a paired t-test. P < 0.05 was considered to indicate significance.
Results
Effects of azilsartan on kidney function
Body weight was significantly lower in the VEH group and AZ group than in the sham group (P < 0.001), though the VEH group and AZ group were not different from each other (Fig. 1a). Urinary volume was significantly higher in the VEH and AZ groups than in the sham group (P < 0.001), though there was no difference between the VEH and AZ groups (Fig. 1b).
Body weight, urinary volume, serum creatinine concentration, and urinary protein excretion in the three groups. a Body weight was significantly lower in the VEH and AZ groups (**P < 0.001 sham vs. VEH and AZ). b The urinary volume was significantly higher in the VEH and AZ groups (**P < 0.001 sham vs. VEH and AZ). c The serum creatinine concentration was significantly higher after adenine administration (**P < 0.001 sham vs. VEH and AZ). Although there was no significant difference in the VEH and AZ groups at 5 weeks, the serum creatinine concentration was significantly lower in the AZ group than in the VEH group (†P < 0.05 AZ vs. VEH). d Urinary protein excretion was also significantly higher after adenine administration (**P < 0.001 sham vs. VEH and AZ). Though there was no significant difference between the VEH and AZ groups at 9 weeks, urinary protein excretion tended to be suppressed from 5 to 9 weeks in the AZ group (P = 0.10)
After 4 weeks of adenine administration, the serum creatinine level, blood urea nitrogen (BUN), and urinary protein of both groups were aggravated to the same degree. Although the BUN level after azilsartan treatment was not different between the two groups (VEH group vs. AZ group: 54.4 ± 21.2 mg/dl vs. 48.3 ± 15.7 mg/dl; P = 0.38), the serum creatinine level was significantly lower in the AZ group (VEH group vs. AZ group: 0.81 ± 0.33 mg/dl vs. 0.59 ± 0.22 mg/dl; P < 0.05, Fig. 1c). Urinary protein excretion was significantly higher in the VEH and AZ groups (P < 0.001 Fig. 1d). Although there was no significant difference between the VEH and AZ groups, urinary protein excretion tended to be suppressed from 5 to 9 weeks in the AZ group only, though it was not significant (5 weeks vs 9 weeks: 18.4 ± 7.3 vs.16.7 ± 5.4 mg/day; P = 0.10).
Effects of azilsartan on urinary sodium concentration
Although there was no significant difference in urinary sodium excretion between the two groups after azilsartan administration (Fig. 2a), urinary sodium excretion in the AZ group increased significantly after azilsartan administration (week 5 vs. week 9: 1.56 ± 0.28 mmol/day vs. 1.87 ± 0.25 mmol/day, P < 0.05) (Fig. 2a). Daytime and nighttime were considered separately, and although urinary sodium excretion was significantly enhanced during the daytime, in other words during the nonactive phase, nighttime urinary sodium concentration was unchanged in the AZ group (Fig. 2b, c).
Urinary sodium excretion in the three groups. a Whole-day sodium excretion was significantly increased with azilsartan administration in the AZ group. (†P < 0.05 AZ 5 weeks vs. 9 weeks). b Daytime sodium excretion was also significantly increased by azilsartan administration in the AZ group. (*P < 0.01 sham vs. VEH and AZ, †P < 0.05 AZ 5 weeks vs. 9 weeks). c Nighttime sodium excretion was not significantly different among the three groups
Effects of azilsartan on blood pressure and the sympathetic nervous system
Azilsartan administration significantly reduced mean blood pressure (VEH group vs. AZ group: 100.9 ± 7.1 vs. 76.5 ± 3.8 mmHg; P < 0.001, Fig. 3a, b) and HR (VEH group vs. AZ group: 316.5 ± 44.6 beats/min vs. 290.5 ± 33.4 beats/min; P < 0.001, Fig. 3c, d).
Mean blood pressure and heart rate in the three groups. a Mean blood pressure transition measured by the telemetry system. b Mean blood pressure was significantly higher in the VEH group than in the sham group (**P < 0.001 VEH vs. sham), while it was significantly lower in the AZ group than in the VEH group (††P < 0.001 AZ vs. VEH), and the value was also significantly lower than that in the sham group (P < 0.001). c Heart rate measured by the telemetry system. d The heart rate was significantly higher in the VEH group than in the sham group (**P < 0.001 VEH vs. sham), and it was significantly lower in the AZ group than in the VEH group (††P < 0.001 AZ vs. VEH), though there was no significant difference between the sham and AZ groups
The urinary norepinephrine level was not significantly different after azilsartan administration (VEH group vs. AZ group: 0.76 ± 0.38 vs. 0.98 ± 0.48 μg/day; P = 0.20). The LF of sBP was significantly lower in the AZ group than in the VEH group, and the value in the AZ group was approximately equivalent to the value in sham rats (sham group vs. VEH group vs. AZ group: 3.24 ± 1.69 vs. 4.07 ± 2.67 vs. 3.32 ± 1.93 mmHg2; P < 0.05 between the VEH group and the AZ group, Fig. 4a, b). In addition, sBRG was significantly higher in the AZ group than in the VEH group, but it did not reach the value in the sham group (VEH group vs. AZ group vs. sham group: 1.04 ± 0.62 vs. 1.38 ± 0.69 vs. 1.59 ± 0.46 ms/mmHg; P < 0.001 between the VEH group and the AZ group; P < 0.01 between the AZ group and the sham group, Fig. 4c, d). These data suggest that azilsartan has a sympathoinhibitory effect.
SNS activity measured by the telemetry system. a The transition in the LF of sBP measured by the telemetry system. b T he LF of sBP was significantly higher in the VEH group than in the sham group (**P < 0.001 VEH vs. sham), and it was significantly suppressed by azilsartan administration to a value comparable to that in the sham group (††P < 0.001 AZ vs. VEH). c The transition in sBRG measured by the telemetry system. d The sBRG was significantly lower in the VEH group than in the sham group (**P < 0.001 VEH vs. sham). Although it recovered significantly with azilsartan administration (††P < 0.001 AZ vs. VEH), it was still lower than that in the sham group
ACE1 and ACE2 expression in the kidney
In the glomeruli, ACE2 staining was more intense in the VEH group and AZ group than in the sham group (P < 0.001) (Fig. 5a–c, g). However, ACE1 staining was not significantly different among the three groups (Fig. 5d–f, h). Thus, the ACE1/ACE2 ratio in the glomeruli was significantly lower in the VEH group and AZ group than in the sham group (P < 0.05) (Fig. 5i). Similarly, in the tubules, ACE2 staining was more intense in the VEH group and AZ group than in the sham group (P < 0.01) (Fig. 5a–c, j), although ACE1 was not (Fig. 5d–f, k). The ACE1/ACE2 ratio also tended to be lower in the VEH group and sham group, though it was not significant (Fig. 5l). Immunoblotting showed that the protein expression levels of ACE1 and ACE2 were not different among the three groups (Fig. 6a, b).
Immunostaining of kidney cortical tissue. ACE2 staining in a sham, b VEH, and c AZ. ACE1 staining in d sham, e VEH, and f AZ. g Glomerular ACE2 staining was significantly higher in the VEH and AZ groups (**P < 0.001 VEH vs. sham, ††P < 0.001 AZ vs. sham). There was no significant difference between the VEH and AZ groups. h Glomerular ACE1 was comparable in the three groups. i The glomerular ACE2/ACE1 ratio was significantly suppressed in the VEH and AZ groups (*P < 0.05 VEH vs. sham, †P < 0.05 AZ vs. sham). j Tubular ACE2 staining was also significantly elevated in the VEH and AZ groups (**P < 0.001 VEH vs. sham, ††P < 0.001 AZ vs. sham). There was no significant difference between the VEH and AZ groups. k Tubular ACE1 was comparable in the three groups. l Tubular ACE2/ACE1 tended to be lower in the VEH and AZ groups than in the sham group, though the difference was not significant
NCC is suppressed by azilsartan administration
The expression of each tubular sodium transporter was evaluated to explore the mechanism of natriuresis demonstrated above. Although Na + -H + exchanger-3 (NHE3), NKCC2, and ENaC expression levels were not altered by azilsartan administration (Fig. 7a, b, d), NCC was significantly suppressed by azilsartan (Fig. 7c). Therefore, NCC suppression might be responsible for the natriuretic effect.
Discussion
First, in this study, azilsartan was found to have a renoprotective effect in an adenine-induced chronic renal failure model. In Dahl salt-sensitive rats fed a high-fat, high-salt diet, azilsartan reduced albuminuria significantly, but comparatively the same effect was seen in the group administered chlorthalidone, in which approximately the same antihypertensive effect was observed [20]. Although olmesartan completely abolished elevated urinary albumin excretion in a remnant kidney model, it is difficult to distinguish this effect from the antihypertensive effect since blood pressure is quite elevated in this model [21]. These results suggest that the renoprotective effect of ARBs may be partly due to their strong antihypertensive effect. In the present model, although blood pressure elevation was relatively slight in the nonmedication group, improvement of the serum creatine level was seen with the ARB. Thus, ARBs might be renoprotective when blood pressure elevation is relatively mild.
Second, it was demonstrated that azilsartan administration not only exerted a potent antihypertensive effect but also suppressed the heart rate and LF of sBP, while it enhanced sBRG, which suggests that azilsartan has a sympatholytic effect in this CKD model. It has been postulated that several antihypertensive drugs have sympathoexcitatory effects. For example, the calcium channel blockers amlodipine and nifedipine increased plasma noradrenaline concentration and MSNA, and they increased the ratio of the low- to the high-frequency component of the power spectrum of the electrocardiogram in humans, which means that though calcium channel blockers have a strong antihypertensive effect, they activate sympathetic nervous system activity [22]. Similarly, chlorthalidone increased sympathetic nervous system activity as assessed by microneurography in untreated hypertensive patients [23].
There are many reports of the relationship between ARB administration and sympathetic nervous system activity. Valsartan did not affect HR or MSNA, while amlodipine increased both [24], which suggests that ARB administration at least did not elicit sympathetic counter-regulation. In obesity-prone rats fed a high-fat diet, telmisartan reduced oxidative stress in the rostral ventrolateral medulla and sympathetic nervous system activity in not only vehicle but also losartan-treated rats [25], which indicates that the sympatholytic effect might differ within the ARB subtype. Similarly, in SHR/NDmcr-cp (+/+) rats, a model of metabolic syndrome, azilsartan significantly reduced urinary norepinephrine excretion and the LF of sBP and increased sBRG [11].
In general, the sympathetic nervous system has been proven to be activated via renin–angiotensin–aldosterone system (RAS) activation [26], renal ischemia [27], decreased nitric oxide availability [28], chemoreflex activation [29], and reduced renalase secretion [30] in CKD. Since it has been demonstrated that MSNA is inversely correlated with GFR [5] and it has been proposed that renal nerve stimulation, especially β2 adrenergic receptors, induces kidney fibrosis and inflammation [31], sympathetic nerve overactivity is not only the consequence of kidney damage but also the cause of kidney function loss [6]. In fact, a sympatholytic agent such as moxonidine has been proven to have an antialbuminuric effect independent of its antihypertensive effect [32]; hence, the sympatholytic effect is related to renoprotection in CKD patients. Therefore, the sympatholytic effect observed with azilsartan administration in the present study might be involved in the beneficial effect of azilsartan seen in CKD patients.
Third, in the present study, urinary sodium excretion, especially daytime urinary sodium excretion, was significantly enhanced via administration of azilsartan. There are many reports that ARB has a natriuretic effect in various models [11, 33]. It has been shown that azilsartan increased sodium excretion, and this effect might contribute to decreased blood pressure in SHR/NDmcr-cp( + / + ) rats (SHRcp), a new model of metabolic syndrome [11]. Hatanaka et al. proposed that azilsartan enhanced natriuresis in the dark period in subtotal nephrectomized C57BL/6 mice, and the authors reported that this effect might be partially due to the reduction of NHE3 protein expression in the proximal tubules [33]. Since the enhancement of natriuresis and the consequent antihypertensive effect are considered beneficial for reducing cardiovascular events [34, 35], the increase in sodium excretion observed in the present study might also be beneficial for CKD patients.
Though previous reports proposed that natriuresis in the active phase was enhanced [11, 33], daytime sodium excretion (in other words, sodium excretion in the inactive phase) was instead enhanced in the present study. Unlike other reports, azilsartan was administered in the morning (in other words, at the end of the active phase), and might be the reason for this discrepancy.
The intrarenal RAS is emphasized to be an important and deleterious factor in kidney diseases [36]. Serum angiotensin II is not always suppressed with long-term ARB treatment [37], and conditional deletion of AT1R in the proximal tubules attenuated angiotensin II-induced hypertension [36], which means that the intrarenal RAS is the key player in the injured kidney. Inappropriate activation of the intrarenal RAS is also implicated in a kidney disease model such as 5/6 nephropathy [38]. In angiotensin II-infused mice, sodium reabsorption dependent on NCC is enhanced [39]. Since this effect is also seen in the setting of adrenalectomy, angiotensin II has been proposed to increase the abundance and phosphorylation of NCC independent of aldosterone [40]. NCC is reported to be enhanced through a WNK4-SPAK-dependent pathway, and losartan inhibits this pathway [41]. Although Hatanaka et al. suggested that azilsartan suppressed NHE3 protein and that it had no effect on NCC [33], the present study showed that, at least in the adenine-induced chronic renal failure model, azilsartan suppressed NCC activity but not NHE3 activity. Therefore, in the present model, ARBs might have a natriuretic effect via the suppression of the WNK4-SPAK-NCC pathway.
In the kidney, ACE2 catabolizes Ang II to produce angiotensin 1-7, and the ACE2-angiotensin 1-7-Mas axis counteracts the ACE-angiotensin II-AT1 axis to play a renoprotective role [42]. Therefore, the ACE1/ACE2 ratio is proposed to be one of the indicators of intrarenal RAS. In nephrectomized rats, kidney cortical ACE2 protein expression was significantly decreased, which led to increased albuminuria in an AT1 receptor-dependent manner [43]. In Col4A3(−/−) mice, an Alport syndrome model, the expression and activity of kidney ACE2 decreased, and this alteration coincided with an Ang II increase and Ang1–7 decrease and thus kidney deterioration [44]. Therefore, in a mature rodent CKD model, an increased ACE1/ACE2 ratio might represent the detrimental effect of RAS activation. However, in the kidneys of young db/db mice, ACE2 protein expression is increased, and ACE protein expression is suppressed [45], which might be renoprotective in the early stage of CKD. In the present study, immunostaining showed that ACE1 was not increased by adenine administration, ACE2 was remarkably increased, and, as a consequence, the ACE1/ACE2 ratio was conspicuously downregulated. Presumably, because kidney damage in the adenine-induced chronic renal failure rats used in the present study was comparatively mild, ACE2 was elevated for renoprotection. In db/db mice, candesartan upregulated the renoprotective ACE2/AT2R/Mas axis, which is related to the attenuation of profibrotic processes [46]. In the present study, azilsartan had no effect on ACE1, ACE2, or the ACE1/ACE2 ratio; therefore, these factors did not contribute to the beneficial effects observed in the present study. Since the ACE1/ACE2 ratio was not significantly different between the sham group and the VEH group on immunoblotting, these factors might not be originally changed in this model. Hence, the natriuretic effect induced by azilsartan might not be due to these factors related to RAS. Moreover, sympathetic nervous system activation has also been shown to activate NCC through the β-adrenergic-WNK4 pathway [47]. In the present experiment, telemetry data showed that azilsartan had a sympathoinhibitory effect, and it has been previously shown that sympatholytic agents, for example moxonidine, have a natriuretic effect in a rodent model [48]. Consequently, the suppression of the sympathetic nervous system could be one of the causes of the natriuretic effect of azilsartan.
There are several limitations in the present study. Since the amount of chow ingested by the rats was not measured, the sodium intake from the food could not be accurately evaluated. Moreover, as in a previous report involving subtotal nephrectomized C57BL/6 mice, immunofluorescence and immunoblotting showed suppression of NHE3 protein, but not NCC protein, which differs from the present report [34]. Therefore, one cannot ignore the possibility that this result may not be applicable to other CKD models.
The present study showed that azilsartan, one of the most potent ARBs, has a sympatholytic effect in a CKD model. This role might be in addition to the known favorable actions of ARBs.
References
Iseki K, Ikemiya Y, Iseki C, Takeshita S. Proteinuria and the risk of developing end-stage renal disease. Kidney Int. 2003;63:1468–74.
Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351:1296–305.
Mann JF, Gerstein HC, Pogue J, Bosch J, Yusuf S. Renal insufficiency as a predictor of cardiovascular outcomes and the impact of ramipril: the HOPE randomized trial. Ann Intern Med. 2001;134:629–36.
Vupputuri S, Batuman V, Muntner P, Bazzano LA, Lefante JJ, Whelton PK, et al. Effect of blood pressure on early decline in kidney function among hypertensive men. Hypertension. 2003;42:1144–9.
Grassi G, Quarti-Trevano F, Seravalle G, Arenare F, Volpe M, Furiani S, et al. Early sympathetic activation in the initial clinical stages of chronic renal failure. Hypertension. 2011;57:846–51.
Penne EL, Neumann J, Klein IH, Oey PL, Bots ML, Blankestijn PJ. Sympathetic hyperactivity and clinical outcome in chronic kidney disease patients during standard treatment. J Nephrol. 2009;22:208–15.
Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2014). Hypertens Res. 2014;37:253–390.
Brenner BM, Cooper ME, de Zeeuw D, Keane WF, Mitch WE, Parving HH, et al. RENAAL study investigators. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med. 2001;345:861–9.
Parving HH, Lehnert H, Brochner-Mortensen J, Gomis R, Andersen S, Arner P. The effect of irbesartan on the development of diabetic nephropathy in patients with type 2 diabetes. Ugeskr Laege. 2001;163:5519–24.
Nakamura Y, Ono H, Zhou X, Frohlich ED. Angiotensin type 1 receptor antagonism and ACE inhibition produce similar renoprotection in N(omega)-nitro-L>-arginine methyl ester/spontaneously hypertensive rats. Hypertension. 2001;37:1262–7.
Sueta D, Kataoka K, Koibuchi N, Toyama K, Uekawa K, Katayama T, et al. Novel mechanism for disrupted circadian blood pressure rhythm in a rat model of metabolic syndrome—the critical role of angiotensin II. J Am Heart Assoc. 2013;29:e000035.
Pohl MA, Blumenthal S, Cordonnier DJ, De Alvaro F, Deferrari G, Eisner G, et al. Independent and additive impact of blood pressure control and angiotensin II receptor blockade on renal outcomes in the irbesartan diabetic nephropathy trial: clinical implications and limitations. J Am Soc Nephrol. 2005;16:3027–37.
Yokozawa T, Zheng PD, Oura H, Koizumi F. Animal model of adenine-induced chronic renal failure in rats. Nephron. 1986;44:230–4.
Sueta D, Koibuchi N, Hasegawa Y, Toyama K, Uekawa K, Katayama T, et al. Telmisartan exerts sustained blood pressure control and reduces blood pressure variability in metabolic syndrome by inhibiting s ympathetic activity. Am J Hypertens. 2014;27:1464–71.
Svitok P, Husková Z, Červenková L, Kikerlová S, Vaňourková Z, Sedláková L, et al. The exaggerated salt-sensitive response in hypertensive transgenic rats (TGR mRen-2) fostered by a normotensive female. Hypertens Res. 2019;42:459–68.
Waki H, Kasparov S, Wong LF, Murphy D, Shimizu T, Paton JF. Chronic inhibition of endothelial nitric oxide synthase activity in nucleus tractus solitarii enhances baroreceptor reflex in conscious rats. J Physiol. 2013;546:233–42.
Zhao M, Li Y, Wang J, Ebihara K, Rong X, Hosoda K, et al. Azilsartan treatment improves insulin sensitivity in obese spontaneously hypertensive Koletsky rats. Diabetes Obes Metab. 2011;13:1123–9.
Sugano N, Wakino S, Kanda T, Tatematsu S, Homma K, Yoshioka K, et al. T-type calcium channel blockade as a therapeutic strategy against renal injury in rats with subtotal nephrectomy. Kidney Int. 2008;73:826–34.
Abramoff MD, Magelhaes PJ, Ram SJ. Image Processing with ImageJ. Biophotonics Int. 2014;11:36–42.
Jin C, O’Boyle S, Kleven DT, Pollock JS, Pollock DM, White JJ. Antihypertensive and anti-inflammatory actions of combined azilsartan and chlorthalidone in Dahl salt-sensitive rats on a high-fat, high-salt diet. Clin Exp Pharm Physiol. 2014;41:579–88.
Halleck F, Schroder K, Holleck-Weithmann S, Kossmehl P, Kreutz R, Rothermund L. Cardiorenal protection in experimental hypertension with renal failure: comparison between vasopeptidase inhibition and angiotensin receptor blockade. Clin Exp Hypertens. 2015;37:26–32.
Toal CB, Meredith PA, Elliott HL. Long-acting dihydropyridine calcium-channel blockers and sympathetic nervous system activity in hypertension: a literature review comparing amlodipine and nifedipine GITS. Blood Press. 2012;21(Suppl 1):3–10.
Menon DV, Arbique D, Wang Z, Adams-Huet B, Auchus RJ, Vongpatanasin W. Differential effects of chlorthalidone versus spironolactone on muscle sympathetic nerve activity in hypertensive patients. J Clin Endocrinol Metab. 2009;94:1361–6.
Struck J, Muck P, Trubger D, Handrock R, Weidinger G, Dendorfer A, et al. Effects of selective angiotensin II receptor blockade on sympathetic nerve activity in primary hypertensive subjects. J Hypertens. 2002;20:1143–9.
Konno S, Hirooka Y, Kishi T, Sunagawa K. Sympathoinhibitory effects of telmisartan through the reduction of oxidative stress in the rostral ventrolateral medulla of obesity-induced hypertensive rats. J Hypertens. 2012;30:1992–9.
Matsukawa T, Gotoh E, Minamisawa K, Kihara M, Ueda S, Shionoiri H, et al. Effects of intravenous infusions of angiotensin II on muscle sympathetic nerve activity in humans. Am J Physiol. 1991;261:R690–696.
Katholi RE, Whitlow PL, Hageman GR, Woods WT. Intrarenal adenosine produces hypertension by activating the sympathetic nervous system via the renal nerves in the dog. J Hypertens. 1984;2:349–59.
Aiello S, Noris M, Todeschini M, Zappella S, Foglieni C, Benigni A, et al. Renal and systemic nitric oxide synthesis in rats with renal mass reduction. Kidney Int. 1997;52:171–81.
Hering D, Zdrojewski Z, Król E, Kara T, Kucharska W, Somers VK, et al. Tonic chemoreflex activation contributes to the elevated muscle sympathetic nerve activity in patients with chronic renal failure. J Hypertens. 2007;25:157–61.
Li G, Xu J, Wang P, Velazquez H, Li Y, Wu Y, et al. Catecholamines regulate the actvitiy, secretion, and systhesis of renalase. Circulation. 2008;117:1277–82.
Kim J, Padanilam BJ. Renal nerves drive interstitial fibrogenesis in obstructive nephropathy. J Am Soc Nephrol. 2013;24:229–42.
Strojek K, Grzeszczak W, Gorska J, Leschinger MI, Ritz E. Lowering of microalubuminuria in diabetic patients by a sympathicoplegic agent: novel approach to prevent progression of diabetic nephropathy? J Am Soc Nephrol. 2001;12:602–5.
Hatanaka M, Kaimori JY, Yamamoto S, Matsui I, Hamano T, Takabatake Y, et al. Azilsartan improves salt sensitivity by modulating the proximal tubular Na + H+ exchanger-3 in mice. PLoS One. 2016;11:e0147786.
Fitchett D, Zinman B, Wanner C, Lachin JM, Hantel S, Salsali A, et al. EMPA-REG OUTCOME® trial investigators. Heart failure outcomes with empagliflozin in patients with type 2 diabetes at high cardiovascular risk: results of the EMPA-REG OUTCOME® trial. Eur Heart J. 2016;37:1526–34.
ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs. diuretic: the antihypertensive and lipid-lowering treatment to prevent heart attack trial (ALLHAT). JAMA. 2002;288:2981–97.
Gurley SB, Riquir-Brison ADM, Schnermann J, Sparks MA, Allen AM, Haase VH. et al. AT1A angiotensin receptors in the renal proximal tubule regulate blood pressure. Cell Metab. 2011;13:469–75.
MacFadyen RJ, Lee AF, Morton JJ, Pringle SD, Struthers AD. How often are angiotensin II and aldosterone concentrations raised during chronic ACE inhibitor treatment in cardiac failure? Heart. 1999;82:57–61.
Zhou L, Mo H, Miao J, Zhou D, Tan RJ, Hou FF, et al. Klotho ameliorates kidney injury and fibrosis and normalizes blood pressure by targeting the renin-angiotensin system. Am J Pahtol. 2015;185:3211–23.
Zhao D, Seth DM, Navar LG. Enhanced distal nephron sodium reabsorption in chronic angiotensin II infused mice. Hypertension. 2009;54:120–6.
van der Lubbe N, Lim CH, Fenton RA, Meima ME, Jan Danser AH, Zietse R, et al. Angiotensin II induces phosphorylation of the thiazide-sensitive sodium chloride cotransporter independent of aldosterone. Kidney Int. 2011;79:66–76.
San-Cristobal P, Pacheco-Alverez D, Richardson C, Ring AM, Vazquez N, Rafiqi FH, et al. Angiotensin II signaling increases activity of the renal Na-Cl cotransporter through a WNK4-SPAK-dependent pathway. Proc Natl Acad Sci USA. 2009;106:4384–9.
Mizuiri S, Ohashi Y. ACE and ACE2 in kidney disease. World J Nephrol. 2015;4:74–82.
Dilauro M, Zimpelmann J, Robertson SJ, Genest D, Burns KD. Effect of ACE2 and angiotenin-(1-7) in a mouse model of early chronic kidney disease. Am J Physiol Ren Physiol. 2010;298:F1523–1532.
Bae EH, Konvalinka A, Fang F, Zhou X, Williams V, Maksimowski N, et al. Characterization of the intrarenal renin-angiotensin system in experimental Alport syndrome. Am J Pathol. 2015;185:1423–35.
Ye M, Wysocki J, Naaz P, Salabat MR, LaPointe MS, Batlle D. Increased ACE2 and decreased ACE protein in renal tubules from diabetic mice; a renoprotective combination? Hypertension. 2004;43:1120–5.
Callera GE, Antunes TT, Correa JW, Moorman D, Gutsol A, He Y, et al. Differential renal effects of candesartan at high and ultra-high doses in diabetic mice-potential role of the ACE2/AT2R/Mas axis. Biosci Rep. 2016;36:e00398.
Mu S, Shimosawa T, Ogura S, Wang H, Uetake Y, Kawakami-Mori F, et al. Epigenetic modulation of the renal β-adrenergic-WNK4 pathway in salt-sensitive hypertension. Nat Med. 2011;17:573–80.
Schlatter E, Ankorina-Stark I, Haxelmans S, Hohage H. Moxonidine inhibits Na + /H + exchange in proximal tubule cells and cortical collecting duct. Kidney Int. 1997;52:454–9.
Acknowledgements
The authors would like to thank Takeda Pharmaceutical Co., Ltd., for providing azilsartan for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kidoguchi, S., Sugano, N., Takane, K. et al. Azilsartan causes natriuresis due to its sympatholytic action in kidney disease. Hypertens Res 42, 1507–1517 (2019). https://doi.org/10.1038/s41440-019-0271-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-019-0271-1