Abstract
Based on the obesity paradox, people with a normal body mass index (BMI) may have a higher risk of mortality than those with a BMI that falls within the obese range. Despite the availability of other anthropometric measures, obesity is commonly evaluated based on BMI. A body shape index (ABSI) and body roundness index (BRI) have recently been proposed as new anthropometric measures that are calculated with height, weight, and waist circumference. This study investigated the associations between the traditional and new body composition indices and arterial stiffness using the brachial-ankle pulse wave velocity (baPWV). Overall, 3512 individuals (1228 men and 2284 women) were enrolled and were divided into two groups according to BMI. Multiple regression analysis was performed to assess the relationship between baPWV and body composition. baPWV was significantly associated with ABSI (β = 0.087, p = 0.002), visceral adipose tissue (VAT; β = 0.081, p = 0.002), and the visceral/subcutaneous adipose tissue (VAT/SAT) ratio (β = 0.108, p < 0.001) in non-obese men. In non-obese women, baPWV was significantly associated with several variables but not the VAT/SAT ratio. Similarly, baPWV was significantly associated with BMI (β = 0.103, p = 0.038), BRI (β = 0.104, p = 0.036), VAT (β = 0.167, p = 0.001), and the VAT/SAT ratio (β = 0.106, p = 0.028) in obese women. ABSI can be used with high accuracy to evaluate fat distribution in non-obese men to predict arterial stiffness. However, the BRI should be used in addition to BMI to assess the body composition of women more accurately. ABSI and the BRI can be used to identify predictors of vascular remodeling or organic vascular dysfunction.
Similar content being viewed by others
Introduction
Obesity is an established risk factor for type 2 diabetes, arteriosclerosis, and cardiovascular disease (CVD) [1,2,3]. However, some studies have shown that obesity as defined by body mass index (BMI) has a protective effect on health and reduces all-cause mortality [4,5,6]. This phenomenon in which people with a normal BMI may have a higher risk of mortality than those with a BMI within the obese range is called the “obesity paradox” [6, 7].
New indices, namely, a body shape index (ABSI) and the body roundness index (BRI), have been recently proposed as anthropometric measures. ABSI was proposed as a new anthropometric measure in 2012, and it is calculated with waist circumference (WC), BMI, and height [8, 9]. Several studies have reported that ABSI is more strongly associated with mortality than BMI or WC [9,10,11]. It is also known that ABSI is associated with cardiometabolic risk factors and arterial stiffness [8, 12]. Furthermore, high score of ABSI may be more related to visceral adipose tissue (VAT) than peripheral adipose tissue [9].
The BRI is another composition index that is based on WC and height [13] and is considered a predictor of body fat and VAT. One study showed that ABSI was the best predictor of coronary heart disease in men, whereas the BRI was the best anthropometric index in women [14].
Several studies have indicated that VAT is more strongly associated with metabolic risk and cardiovascular risk than subcutaneous adipose tissue (SAT) [15,16,17]. However, this association is unclear, and conflicting results have been obtained [18, 19]. VAT may also show a U-shaped pattern similar to that of BMI; thus, it may also reflect the “obesity paradox” [18]. The obesity paradox status can be described using several concepts, including “metabolically healthy/unhealthy obesity,” which describes patients with non-obesity/obesity using major metabolic factors instead of BMI [6]. In general, studies have shown that fat distribution, and not fat deposit, is the key factor explaining the obesity paradox [6]. The VAT/SAT ratio is used as a metric index of fat distribution, and some studies have suggested that the VAT/SAT ratio is associated with cardiometabolic risk and mortality [17, 19] and CVD [20].
Despite the availability of other anthropometric measures, obesity is commonly evaluated according to BMI, and people with a normal BMI but at high risk of mortality tend to slip by health examinations based on their normal BMI. ABSI and BRI, to a greater extent than BMI, are useful surrogate biomarkers of CVD that can be used to circumvent the obesity paradox. Arterial stiffness is a known high-risk factor of CVD and other cardiovascular conditions [21]. We selected the brachial-ankle pulse wave velocity (baPWV) to evaluate arterial stiffness since baPWV is a currently used, basic, widely accepted assessment tool. This study aimed to investigate the differences in using traditional and new body composition indices to evaluate arterial stiffness.
Methods
Participants
The Japan Multi-Institutional Collaborative Cohort Study was launched in 2005 to investigate gene–environmental interactions in lifestyle-related diseases [22]. This study included individuals who were enrolled in the Japan Multi-Institutional Collaborative Cohort Study second survey in the Kyoto area from 2013 to 2017. A total of 3913 participants were eligible for the analyses. All subjects underwent a routine health checkup. Among these 3913 participants, 401 were excluded; 353 were excluded due to insufficient laboratory data, and 48 were excluded due to the absence of other data. After these exclusions, 3512 individuals (1228 men and 2284 women) were eligible for the analyses. The participants were divided into four groups by obesity status and sex based on previous studies indicating that differences in BMI and/or sex influenced arterial stiffness [23, 24].
The study was approved by the Institutional Ethics Committee of the Kyoto Prefectural University of Medicine (approval number: RBMR-E-36–8 at 2013) and was conducted in accordance with the principles of the Declaration of Helsinki. All participants provided written informed consent before participation.
Clinical and biochemical analyses
The following lifestyle and medical information obtained through self-administered questionnaires was evaluated: alcohol consumption status (ethanol/day), smoking status (assessed using the Brinkman index (number of cigarettes smoked per day × total number of years smoked)), sleeping time, current medications, and physical activity (assessed as metabolic equivalents (METs) [25] for daily and leisure activities). The alcohol content of each type of beverage (Japanese sake, beer, shochu, whiskey and wine) was calculated; the alcohol consumption was determined by calculating the number of drinks per day, and this amount was converted into 23 g of ethanol. In addition, anthropometric data obtained from the health check-ups were collected. WC was measured at the umbilical level during minimal respiration in a standing position. BMI was calculated as weight divided by the square of the height (kg/m2). ABSI and the BRI were calculated based on previous studies [9, 13].
VAT and SAT were measured using a dual bioelectrical impedance analyzer (DUALSCAN, Omron Healthcare Co. Ltd., Kyoto, Japan). The brachial-ankle pulse wave velocity (baPWV), used to evaluate arterial stiffness, was measured with a volume-plethysmographic apparatus (BP-203RPE II form PWV/ABI, Omron Healthcare Co. Ltd., Kyoto, Japan). We simultaneously measured baPWV on both the right and left sides, and the average values in each individual were subjected to statistical analysis. The cut-off point for obesity was set at a BMI of 25 kg/m2 according to the definition of obesity in Japan [26].
Statistical analysis
Continuous variables were expressed as the means ± standard deviations (SDs) or range. Spearman’s rank correlation analysis was performed to assess the relationship between the baPWV and other variables, including body composition. Multiple regression analysis was performed to assess the combined influence of variables on baPWV. To examine the effects of various factors on baPWV, the following factors were considered as independent variables: age, daily alcohol consumption, Brinkman index, sleeping time, METs, drug treatment for hypertension, dyslipidemia, and diabetes. All statistical analyses were performed using SPSS statistical software version 25 (IBM Japan, Tokyo, Japan), and P < 0.05 was considered statistically significant.
Results
A total of 3512 participants were divided into two groups according to the BMI cut-off of 25 kg/m2. The anthropometric measurements and questionnaires used in this study are shown in Table 1. The mean ABSI was 0.080 in both obese (mean age, 58.4 years; n = 347) and non-obese men (mean age: 58.7 years; n = 881). ABSI was not different among those who were obese. Moreover, the mean ABSI was 0.081 in non-obese women (mean age: 56.9 years; n = 1983) and 0.082 in obese women (mean age: 58.2 years; n = 301). The mean VAT/SAT ratio was 0.543 in non-obese men and 0.560 in obese men. Moreover, the mean VAT/SAT ratio was 0.434 in non-obese women and 0.385 in obese women. The VAT/SAT ratio was not significantly different between non-obese and obese men, whereas it was significantly different between obese and non-obese women.
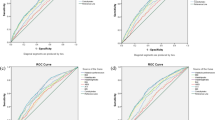
Correlations between baPWV and the anthropometric indices are shown in Table 2. In non-obese men, baPWV was significantly related to all indices: BMI (coefficient = 0.073, p = 0.030), ABSI (coefficient = 0.321, p < 0.001), BRI (coefficient = 0.301, p < 0.001), WC (coefficient = 0.164, p < 0.001), VAT (coefficient = 0.217, p < 0.001), SAT (coefficient = 0.098, p = 0.004), and the VAT/SAT ratio (coefficient = 0.194, p < 0.001). However, baPWV was only associated with ABSI (coefficient = 0.255, p < 0.001), BRI (coefficient = 0.232, p < 0.001), VAT (coefficient = 0.207, p < 0.001), and the VAT/SAT ratio (coefficient = 0.286, p < 0.001) among obese men. Among non-obese women, baPWV was also related to all indices: BMI (coefficient = 0.135, p < 0.001), ABSI (coefficient = 0.342, p < 0.001), BRI (coefficient = 0.346, p < 0.001), WC (coefficient = 0.252, p < 0.001), VAT (coefficient = 0.323, p < 0.001), SAT (coefficient = 0.206, p < 0.001), and the VAT/SAT ratio (coefficient = 0.136, p < 0.001); however, baPWV was only associated with ABSI (coefficient = 0.236, p < 0.001), BRI (coefficient = 0.232, p < 0.001), VAT (coefficient = 0.274, p < 0.001), and the VAT/SAT ratio (coefficient = 0.248, p < 0.001) in obese women.
Multiple regression analysis was then performed to identify the variables that were strongly associated with baPWV (Table 3). When the number of adjustment factors increased from Model I to III, the number of body composition factors that were significantly associated with baPWV tended to decrease. The interaction between baPWV and body composition was influenced by hypertension, dyslipidemia, diabetes, and lifestyle factors in both men and women.
Notably, the results were different between non-obese and obese men. As shown in model III, baPWV was significantly associated with ABSI (β = 0.087, p = 0.002), VAT (β = 0.081, p = 0.002), and the VAT/SAT ratio (β = 0.108, p < 0.001) in non-obese men. However, baPWV was only related to the VAT/SAT ratio in obese men. These results showed that the VAT/SAT ratio was the key factor that was strongly correlated with baPWV.
In non-obese women, baPWV was significantly associated with several variables, with the exception of the VAT/SAT ratio (β = 0.022, p = 0.205), as follows: BMI (β = 0.046, p = 0.007), ABSI (β = 0.090, p < 0.001), BRI (β = 0.099, p < 0.001), WC (β = 0.079, p < 0.001), VAT (β = 0.130, p < 0.001), and SAT (β = 0.096, p < 0.001) in model III. Similarly, baPWV was significantly associated with BMI (β = 0.103, p = 0.038), BRI (β = 0.104, p = 0.036), VAT (β = 0.167, p = 0.001), and the VAT/SAT ratio (β = 0.106, p = 0.028) in obese women.
Discussion
Obesity is an established risk factor for CVD. Currently, obesity is identified based on BMI or WC [6, 23, 27]. However, individuals with a BMI >30 or <18.5 have high mortality rates [6, 28, 29]. In the obesity paradox, obesity has a protective effect on health and reduces the risk of all-cause mortality. This paradox indicates that non-obese metabolically unhealthy people have a higher risk of CVD than those who are obese and metabolically healthy.
Fat distribution should also be categorized differently based on non-obese or obese status because the body composition is different, and the metabolic status cannot be accurately assessed using only one index, such as BMI. Although BMI is widely used, it does not accurately measure fat content, reflect the proportions of muscle and fat, or account for sex and racial differences in fat content and the distribution of visceral and subcutaneous fat [9]. Thus, BMI cannot accurately reflect fat distribution. The relationship between body composition indices and baPWV differs according to obesity and/or sex (Table 2). Furthermore, an analysis adjusted for lifestyle and anamnesis in men showed no relationship between BMI and baPWV (Table 3), indicating that fat distribution influences changes in baPWV. It was very difficult to find non-obese metabolically unhealthy people. BMI or WC is commonly used to determine obesity or non-obesity in the general population. However, other indices can be used to measure body composition. In particular, VAT, SAT, and the VAT/SAT ratio can be used to evaluate fat deposits and distribution. ABSI and the BRI are newer indices that can be calculated easily [9, 13]; therefore, we focused on ABSI and the BRI calculated with WC, BMI, and height. Some studies reported that ABSI and the BRI were associated with CVD [8, 12, 14]. However, whole-body vibration training led to reductions in arterial stiffness, central blood pressure, and wave reflections in young obese women [30]. An effective intervention should be focused on vascular health promotion and obesity prevention in young obese patients. Using cost-effective basic assessment tools, such as ABSI and the BRI anthropometric indices, arterial stiffness can be assessed, thus allowing for early clinical management of patients.
Multiple regression analysis showed that baPWV was correlated with ABSI, VAT, and the VAT/SAT ratio among non-obese men, whereas baPWV was only correlated with the VAT/SAT ratio among obese men. In contrast, baPWV was not correlated with BMI or WC. These results indicate that fat distribution is more important than fat deposits in men. Among non-obese women, baPWV was correlated with all indices except for the VAT/SAT ratio, whereas baPWV was correlated with BMI, BRI, VAT, and the VAT/SAT ratio among obese women. Moreover, baPWV was more strongly correlated with BRI (β = 0.099) than BMI (β = 0.046) among non-obese women. These results indicated that although BMI and WC are widely used, they are insufficient to accurately identify metabolically healthy/unhealthy men and women. Thus, the influence of adipose tissue distribution on health should also be evaluated based on sex differences.
Adipose tissue distribution typically differs between men and women. Men generally have larger amounts of VAT than women, while women have larger amounts of SAT [23, 31]. These sex differences in adipose tissue distribution may contribute to a more insulin-sensitive environment in women, as visceral and hepatic adiposity is associated with increased insulin resistance [31]. The mean value of VAT/SAT in men and women with/without obesity is described in Table 1. These data indicate that due to obesity, men have more VAT than SAT compared with women. Moreover, normal weight evaluated by BMI may mask metabolically healthy or unhealthy conditions because VAT accumulation could not be detected. Some studies have reported that VAT is a more important risk factor than SAT, independent of total accumulation of fat [17, 19]. Increased VAT accumulation causes vascular inflammation and insulin resistance; thus, it is associated with atherosclerosis, diabetes, and CVD [17, 19]. In particular, VAT is related to baPWV among non-obese individuals of both sexes. These differences in fat distribution by sex and obesity status indicate that ABSI is the most reliable index to assess metabolic status in non-obese men, while BRI is the index of choice for assessing metabolic status in women.
This study has some limitations. First, its cross-sectional design and the inclusion of only Japanese participants limits its applicability to the general population. Further studies in other ethnic groups are needed to validate our findings. The strength of the study is that a large number of participants were included, and we implemented a population-based cohort design. Another limitation is that the mean cut-off values for ABSI and BRI have yet to be established; thus, we were not able to categorize the ABSI and BRI of the participants.
ABSI has high accuracy for evaluating fat distribution in non-obese men to predict arterial stiffness. However, the BRI should be used among women in addition to BMI to assess body composition more accurately. ABSI and the BRI can be used to identify metabolically healthy/unhealthy individuals and can act as predictors for vascular remodeling or organic vascular dysfunction.
References
Velasquez-Rodriguez CM, Velasquez-Villa M, Gomez-Ocampo L, Bermudez-Cardona J. Abdominal obesity and low physical activity are associated with insulin resistance in overweight adolescents: a cross-sectional study. BMC Pediatr. 2014;14:258.
Pal S, Radavelli-Bagatini S. Association of arterial stiffness with obesity in Australian women: a pilot study. J Clin Hypertens. 2013;15:118–23.
Abbasi A, Juszczyk D, van Jaarsveld CHM, Gulliford MC. Body mass index and incident type 1 and type 2 diabetes in children and young adults: a retrospective cohort study. J Endocr Soc. 2017;1:524–37.
Sharma A, Lavie CJ, Borer JS, Vallakati A, Goel S, Lopez-Jimenez F, et al. Meta-analysis of the relation of body mass index to all-cause and cardiovascular mortality and hospitalization in patients with chronic heart failure. Am J Cardiol. 2015;115:1428–34.
Vlaras E, Giakoumidakis K, Fotos NV, Chatziefstratiou AA, Brokalaki H. The presence of obesity paradox in Greek patients with chronic heart failure. Pragmatic Obs Res. 2017;8:183–7.
Ahima RS, Lazar MA. Physiology. The health risk of obesity–better metrics imperative. Science. 2013;341:856–8.
Wildman RP, Muntner P, Reynolds K, McGinn AP, Rajpathak S, Wylie-Rosett J, et al. The obese without cardiometabolic risk factor clustering and the normal weight with cardiometabolic risk factor clustering: prevalence and correlates of 2 phenotypes among the US population (NHANES 1999-2004). Arch Intern Med. 2008;168:1617–24.
Bouchi R, Asakawa M, Ohara N, Nakano Y, Takeuchi T, Murakami M, et al. Indirect measure of visceral adiposity ‘A Body Shape Index’ (ABSI) is associated with arterial stiffness in patients with type 2 diabetes. BMJ open diabetes Res care. 2016;4:e000188.
Krakauer NY, Krakauer JC. A new body shape index predicts mortality hazard independently of body mass index. PloS One. 2012;7:e39504.
Krakauer NY, Krakauer JC. Dynamic association of mortality hazard with body shape. PloS One. 2014;9:e88793.
Ji M, Zhang S, An R. Effectiveness of A Body Shape Index (ABSI) in predicting chronic diseases and mortality: a systematic review and meta-analysis. Obes Rev. 2018;19:737–59.
Bertoli S, Leone A, Krakauer NY, Bedogni G, Vanzulli A, Redaelli VI, et al. Association of Body Shape Index (ABSI) with cardio-metabolic risk factors: a cross-sectional study of 6081 Caucasian adults. PloS one. 2017;12:e0185013.
Thomas DM, Bredlau C, Bosy-Westphal A, Mueller M, Shen W, Gallagher D, et al. Relationships between body roundness with body fat and visceral adipose tissue emerging from a new geometrical model. Obesity . 2013;21:2264–71.
Wang F, Chen Y, Chang Y, Sun G, Sun Y. New anthropometric indices or old ones: which perform better in estimating cardiovascular risks in Chinese adults. BMC Cardiovasc Disord. 2018;18:14.
Fox CS, Massaro JM, Hoffmann U, Pou KM, Maurovich-Horvat P, Liu CY, et al. Abdominal visceral and subcutaneous adipose tissue compartments: association with metabolic risk factors in the Framingham Heart Study. Circulation . 2007;116:39–48.
Bouchi R, Takeuchi T, Akihisa M, Ohara N, Nakano Y, Nishitani R, et al. High visceral fat with low subcutaneous fat accumulation as a determinant of atherosclerosis in patients with type 2 diabetes. Cardiovasc Diabetol. 2015;14:136.
Kaess BM, Pedley A, Massaro JM, Murabito J, Hoffmann U, Fox CS. The ratio of visceral to subcutaneous fat, a metric of body fat distribution, is a unique correlate of cardiometabolic risk. Diabetologia. 2012;55:2622–30.
Shil Hong E, Khang AR, Roh E, Jeong Ku E, An Kim Y, Min Kim K, et al. Counterintuitive relationship between visceral fat and all-cause mortality in an elderly Asian population. Obesity . 2015;23:220–7.
Ladeiras-Lopes R, Sampaio F, Bettencourt N, Fontes-Carvalho R, Ferreira N, Leite-Moreira A, et al. The ratio between visceral and subcutaneous abdominal fat assessed by computed tomography is an independent predictor of mortality and cardiac events. Rev Esp de Cardiol (Engl ed). 2017;70:331–7.
Fukuda T, Bouchi R, Takeuchi T, Nakano Y, Murakami M, Minami I, et al. Ratio of visceral-to-subcutaneous fat area predicts cardiovascular events in patients with type 2 diabetes. J diabetes Investig. 2018;9:396–402.
Ohkuma T, Ninomiya T, Tomiyama H, Kario K, Hoshide S, Kita Y, et al. Brachial-ankle pulse wave velocity and the risk prediction of cardiovascular disease: an individual participant data meta-analysis. Hypertension . 2017;69:1045–52.
Wakai K, Hamajima N, Okada R, Naito M, Morita E, Hishida A, et al. Profile of participants and genotype distributions of 108 polymorphisms in a cross-sectional study of associations of genotypes with lifestyle and clinical factors: a project in the Japan Multi-Institutional Collaborative Cohort (J-MICC) Study. J Epidemiol. 2011;21:223–35.
van den Munckhof ICL, Holewijn S, de Graaf J, Rutten JHW. Sex differences in fat distribution influence the association between BMI and arterial stiffness. J Hypertens. 2017;35:1219–25.
Bouchi R, Minami I, Ohara N, Nakano Y, Nishitani R, Murakami M, et al. Impact of increased visceral adiposity with normal weight on the progression of arterial stiffness in Japanese patients with type 2 diabetes. BMJ open diabetes Res care. 2015;3:e000081.
Hara M, Higaki Y, Taguchi N, Shinchi K, Morita E, Naito M, et al. Effect of the PPARG2 Pro12Ala polymorphism and clinical risk factors for diabetes mellitus on HbA1c in the Japanese general population. J Epidemiol. 2012;22:523–31.
Examination Committee of Criteria for ‘Obesity Disease' in Japan; Japan Society for the Study of Obesity. New criteria for ‘obesity disease’ in Japan. Circ J. 2002;66:987–92.
Van Gaal LF, Mertens IL, De Block CE. Mechanisms linking obesity with cardiovascular disease. Nature. 2006;444:875–80.
Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J, Halsey J, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373:1083–96.
Berrington de Gonzalez A, Hartge P, Cerhan JR, Flint AJ, Hannan L, MacInnis RJ, et al. Body-mass index and mortality among 1.46 million white adults. New Engl J Med. 2010;363:2211–9.
Alvarez-Alvarado S, Jaime SJ, Ormsbee MJ, Campbell JC, Post J, Pacilio J, et al. Benefits of whole-body vibration training on arterial function and muscle strength in young overweight/obese women. Hypertens Res. 2017;40:487–92.
Geer EB, Shen W. Gender differences in insulin resistance, body composition, and energy balance. Gend Med. 2009;6 Suppl 1:60–75.
Funding
This study was supported by a Grant-in-Aid for Scientific Research on Priority Areas of Cancer (No. 17015018) and Innovative Areas (No. 221S0001) and by JSPS KAKENHI Grant Number 16H06277 from the Japanese Ministry of Education, Culture, Sports, Science, and Technology.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Haraguchi, N., Koyama, T., Kuriyama, N. et al. Assessment of anthropometric indices other than BMI to evaluate arterial stiffness. Hypertens Res 42, 1599–1605 (2019). https://doi.org/10.1038/s41440-019-0264-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-019-0264-0
Keywords
This article is cited by
-
Association between visceral fat mass and arterial stiffness among community-based screening participants
Hypertension Research (2023)
-
New anthropometric measurement alternatives to BMI and hypertension
Hypertension Research (2023)
-
Association of waist-to-height ratio with hypertension and its subtypes in southern China
Journal of Human Hypertension (2022)
-
Does body mass index or waist-hip ratio correlate with arterial stiffness based on brachial-ankle pulse wave velocity in Chinese rural adults with hypertension?
BMC Cardiovascular Disorders (2021)
-
Blood pressure and adiposity in midlife Singaporean women
Hypertension Research (2021)