Abstract
Peripheral arterial disease (PAD) is substantially prevalent among patients in the end stage of renal disease (ESRD). We considered factors related to peripheral arterial disease in patients undergoing hemodialysis including the important role of monocyte chemoattractant protein-1 (MCP-1) serum concentrations. We studied 150 patients in on-line-predilution hemodiafiltration. Dialysis sufficiency was defined by Kt/V for urea. PAD was defined using clinical criteria, ankle-brachial index and Doppler ultrasound in the lower limbs. MCP-1 serum concentrations were measured using enzyme-linked immunoabsorbed assay (ΕLISA). We performed chi-square tests and logistic regression analysis to investigate risk factors for the prevalence of PAD in these patients including MCP-1 serum concentrations. The patients with manifested PAD had elevated MCP-1, higher BP, higher arterial stiffness markers, higher markers of malnutrition, uncontrolled metabolic acidosis, bone disease and lower obtained dialysis adequacy than the patients without PAD. The association between PAD manifestation and high MCP-1 was found significant (x2 = 9.6, p = 0.001). The built logistic regression analysis showed that the high MCP-1 increased the risk for PAD 3.2 (95% C.I 1.3–8.2) folds after adjustment for confounders. PAD was also significantly associated with non-administration of vitamin D agents during dialysis (x2 = 3.5, p = 0.04).Malnutrition, low-grade inflammation mainly defined by high MCP-1 serum concentrations, metabolic acidosis and bone disease were included in significant predictors for peripheral arterial disease in patients undergoing hemodiafiltration. The obtained dialysis sufficiency and the therapy during dialysis sessions seem to play an additional role in the demonstration of peripheral vascular disease in these patients.
Similar content being viewed by others
Core tips
-
In this study, we observed a significant association between high MCP-1 serum concentrations and manifested PAD in dialysis patients and a such finding was also verified by an adjusted model including traditional and specific covariates for this population of patients. High MCP-1 serum levels could be used as a screening test for the definition of PAD in these patients.
-
The administration of vitamin D during dialysis may play an additional role rather than on the regulation of bone disease in these patients, as we observed a significant association between non-administration of vitamin D and manifested PAD, although the bone disease markers were found to mildly differ between the groups of patients with and without PAD.
Introduction
Peripheral arterial disease (PAD) is a common manifestation of atherosclerosis, which is a systemic disease that affects the vascular system [1]. As a result of the atherosclerotic process, narrowing and occlusions occur not only in coronary and cerebral arteries, but also in the aorta and in its branches [2]. Such a condition is called PAD or peripheral arterial occlusive disease. The arterial stenosis of the lower limbs is generally symmetrical [3]. However, the distal part of leg and foot is less seriously affected by atherosclerosis due to collateral development.
Systemic atherosclerosis including PAD progresses with age, decreases quality of life, life expectancy and causes overall functional disability including restricted lower extremity movements. Moreover, the demonstration of PAD has an important impact on morbidity and mortality, as individuals with PAD have a 2- to 4-fold higher risk of myocardial infarction and vascular death [1, 2].
PAD is substantially prevalent among patients in the end stage of renal disease (ESRD) in comparison to general population and subjects on hemodialysis are more likely to develop systemic atherosclerotic disease than individuals without advanced renal failure [4, 5]. The elevated prevalence of systemic atherosclerosis including PAD in dialysis patients may be attributed to a unique combination of biochemical, endocrine and molecular abnormalities in these patients due to renal disease. Previously, a few studies have been reported in the role of the levels of soluble cell adhesion molecules in order to predict PAD in dialysis patients [6, 7].
In this study, we considered factors related to the existence of PAD in patients undergoing permanent hemodiafiltration including the role of monocyte chemoattractant protein-1 (MCP-1) serum concentrations.
Material and methods
Patients
This is a cross-sectional study of a cohort of 150 patients, who were collected from two Medical Centers, “Laiko, University General Hospital of Athens” and Renal Unit of “Diagnostic and Therapeutic Center of Athens Hygeia SA”.
A number of 93 males and 57 females were enrolled in this study, on median age 63.5 ± interquartile range 50–75 years old.
The hemodialysis modality which was applied was on-line-predilution hemodiafiltration (on-l HDF) in the total enclosed patients. The median time on hemodialysis was 5 ± interquartile range 3–10 years.
We excluded patients with diabetes mellitus as a cause of renal disease, patients <18 years of age at initiation of dialysis and patients who had less than 6 months of follow-up. Patients with dialysis catheter and without regular vascular hemodialysis access and those with infections or malignancy were not included in this study. We also excluded the patients with interdialytic weight gain more than 5% of total body weight, which was calculated as the mean of 12–13 dialysis sessions during a treatment month.
The hemodiafiltration treatment was prescribed 3-times weekly for 4 h per session in the total of participants. Similar dialysis conditions were applied for all enrolled subjects, including a dialysis high-flux filter of 1.5 m2 surface area defined by an ultrafiltration coefficient more than 20 ml/h [8] and by the same material synthetic membrane. The blood flow was equal to 400 ml/min during dialysis and the dialysate flow rate was 500–600 ml/min. The volume of replacement liquids was 20 l per session and the sodium concentration equal to140 mmol/l for all subjects. A bicarbonate-based ultrapure buffer dialysis solution was used with a final concentration of bicarbonate in dialysate equal to 32 mmol/l. The used calcium dialysate concentration was equal to 1.50–1.75 mmol/l. Dialysis sufficiency was defined by spKt/V/session (single pool, K: dialyzer clearance; t: time; V: urea distribution volume) [9]. The patients, whose the calculated spKt/V/session was <1.2, were excluded from the study.
The enrolled patients were in a free regular diet and they did not have interdialytic peripheral edema or interdialytic orthostatic hypotension.
The patients with pre-dialysis blood pressure more than 130/80 mmHg (n = 56, a prevalence of 37.3%) were considered hypertensive and they were regularly receiving anti-hypertensive drugs including calcium channel blockers, beta-blockers or inhibitors of angiotensin II AT1 receptors.
Thirty-eight of the studied patients were current smokers (a prevalence of 25.3%), but no one of them had alcohol intake.
The prevalence of PAD(n = 61, 40.7%) was documented using the measurement of ankle-brachial blood pressure index (ABI), the performance of Doppler ultrasound in the lower limbs and a set of clinical criteria including reduced or loss ankle pulses on physical examination, symptomatic intermittent claudication and by a history of a limb artery revascularization. Cardiac disease was defined as the prevalence of left ventricular hypertrophy (LVH, n = 89, 59.3%), coronary artery disease (CAD, n = 50, 33.3%) and congestive heart failure (CHF). The coronary artery disease was documented by clinical signs of angina pectoris, a history of myocardial infarction and coronary artery angioplasty or bypass surgery. The CHF was defined by systolic (n = 44, 29.3%) and diastolic dysfunction (n = 105, 70%). The first and the current cardiovascular events during the study were recorded as one event.
Thirty-nine of the enrolled patients (26%) were preserving a residual renal function and they excreted an interdialytic urine volume more than 100 ml.
Only calcium-free phosphate binders were prescribed for the regulation of bone disease. Sixty-eight of our subjects (a ratio of 45.3%) were treating by intravenous administration of vitamin D supplementation by using calcitriol or paricalcitol during dialysis session depended mainly on serum calcium and phosphate levels. Nobody of the enrolled patients had received intravenous administration of iron during the last 2 months before the starting of the study. Nobody of our patients was receiving NaHCO3 per os or warfarin therapy. Forty-one of our participants (27.3%) were treating by statin and everybody of the enrolled patients was in erythropoietin-α or –β therapy.
In our data, the renal failure was caused by hypertensive nephrosclerosis at a ratio of 33.3%, chronic glomerulonephritis at a ratio of 29.3%, polycystic disease at a ratio 11.3%, interstitial nephritis at a ratio equal to 9.3% and other causes at a ratio 16.7%.
Blood collection
Blood samples were obtained before the beginning of the mean weekly dialysis session for each one of participants according to his dialysis treatment program in a fasting state from the vascular access and were frozen. Therefore, the blood collection was drawn during Wednesday and/or Thursday for the total of our subjects.
In the end of the dialysis session blood samples were obtained at 2 min post dialysis from the arterial dialysis tubing after the reduction of blood pump speed to <80 ml/min for the calculation of the dose of dialysis session by spKt/V for urea [10]. The mean of 12–13 calculations for spKt/V for urea per dialysis session during a treatment month as exposure period was used for statistical analysis.
In each subject, four sequences of samples (every week within exposure period) were obtained for the serum bicarbonate measurements, and their average was used for statistical analysis. Metabolic acidosis was determined by the combination of low serum bicarbonate level, low arterial pH (acidemia) and decreased PCO2, thus metabolic acidosis to be differentiated from respiratory alkalosis, which is another clinical condition that causes decreased bicarbonate levels, but without acidemia [11].
Laboratory measurements
Albumin, calcium (Ca) corrected for the albumin levels, phosphate (P), the ratio of low density lipoproteins (LDL) to high density lipoproteins (HDL) [LDL/HDL] and sodium (Na+) levels during both in the start and in the end of the treatment session were measured using spectrophotometric technique by Chemistry Analyzer (MINDRAY BSλ200, Diamond Diagnostics, USA). The sodium removal was determined as percent sodium removal (PSR) using the following formula: (Na+pre − Na+ post/Na+pre) × 100 [12]. (Ca × P) products were calculated.
Hematological analyzer (Sysmex, xt-4000i, Roche, Hamburg, Germany) was used for hemoglobin.
Radioimmunoassay was used for measurement of intact-parathormone (i-PTH) (CIS biointernational/France).
High-sensitivity C-reactive protein (hsCRP) and monocyte chemoattractant protein-1 (MCP-1) serum concentrations were measured using enzyme-linked immunoabsorbed assays (ΕLISA, Immundiagnostik AG., Germany and Alpco Diagnostics, Anachem, USA, respectively) according to the manufacturer’s specifications.
Metabolic acidosis was defined by serum bicarbonate concentrations <22.0 mmol/l, which were measured in gas machine (Roche, combas b 121) by an electrode-based method taking care of the blood specimens [13].
Normalized protein catabolic rate (nPCR) was calculated from the urea generation rate [14].Body mass index (BMI) was obtained from height and post-dialysis body weight.
Hemodynamic measurements
Pre-dialysis peripheral systolic and diastolic blood pressures (SBP and DBP, respectively) were calculated as the mean of 12–13 measurements during exposure period using an automatic sphygmomanometer OMRON M4-I (Co Ltd Kyoto Japan). Mean peripheral pre-dialysis BP (MBP) was calculated as: MBP = DBP + 1/3 (SBP − DBP).
Hemodynamic measurements were performed before the mid-week dialysis session and after resting of participants for at least 10 min. Arterial stiffness was measured as carotid-femoral pulse wave velocity (c-f PWV) and carotid augmentation index (Aix) using the SphygmoCor system® (AtCor Medical Pty.Ltd, Sydney, Australia) according to the manufacturer’s specifications [10]. In each subject two sequences of measurements were performed, and their mean was used for statistical analysis. Pulse pressure (PP) was derived.
ABI was also calculated as the ratio of the lower values of ankle systolic pressure (pre or posttibial artery), divided by stabilized arm systolic pressure. ABI values <0.9 were rated as low indicating PAD and values >1.4 were rated as high. Moreover, we obtained the assessment of the vascular stenosis using Doppler ultrasonography in the lower limbs for everybody of our participants and the absence of a stenosis ≥50% excluded the presence of PAD [15].
Echocardiographical assessment
Echocardiographical assessment was conducted by a Hewlett Packard SONOS 2500 device using a 2.25-MHz transducer. Two cardiologists examined our patients with the method of conventional M-mode and two-dimensional echocardiography for left ventricular hypertrophy estimation, systolic cardiac function assessment and consideration of the ischemic findings according to the recommendations of the American Society of Echocardiography [16].The left ventricular hypertrophy was defined by a thickness of interventricular septum >11.5 mm. The systolic function of the left ventricle (LV) was assessed by the measurement of ejection fraction (EF) and the systolic dysfunction was defined as EF <50%. Tissue Doppler imaging and pulsed-wave Doppler techniques were used for the evaluation of LV diastolic function [17]. Transmitral early and late diastolic (E and A waves) velocities were measured and the ratio of E/A was calculated. We also measured the peak early (e′) diastolic mitral annular velocity and E/e′ ratio was calculated [18]. E/e′ ratio ≥ 15 and a ratio of E/A ≤ 1 were used to determine the existence of diastolic dysfunction, even if E/A ratio is greatly influenced by hemodynamic status.
Approval and consent
The study was approved by the ethics committee of the Hospitals “Laiko, University General Hospital of Athens” and Renal Unit of “Diagnostic and Therapeutic Center of Athens Hygeia SA”. All included subjects quoted oral informed consent.
Data analysis
Data were analyzed using SPSS 15.0 statistical package for Windows (SPSS Inc, Chicago, Illinois) and expressed as means ± SD or as median value (interquartile range) for data that showed skewed distribution; differences between mean values were assessed by using unpaired t-test for two groups and with Mann–Whitney U-test and expressed as means ± SD or as means Rank. Correlations between variables were defined by Spearman coefficient and the relationships between categorical variables were defined by chi-square tests. P values <0.05 were considered significant.
ROC curve analysis was used for the determination of MCP-1 cut of point related to PAD. We performed a logistic regression analysis to investigate significant risk factors for the prevalence of PAD considering traditional and specific covariates for dialysis patients including MCP-1 serum concentrations.
Results
We examined the differences between the patients without (n = 89) and with (n = 61) PAD manifestation (Table 1). The patients with PAD had significantly higher SBP, DBP, MBP, c-f PWV, Aix, PP, hsCRP and MCP-1 serum levels, but they had significantly lower serum bicarbonate levels, percent sodium removal, LDL/HDL ratio and protein intake defined by nPCR than the patients without PAD. They also had lower ABI, urine output, serum albumin, spKt/V for urea and i-PTH, but they were elder and had higher serum phosphate levels and Ca × P products in comparison to the patient without PAD.
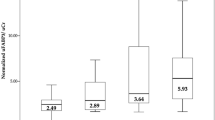
We also divided our patients in two groups according to MCP-1 cut of point value equal to 165.8 ± 1 pg/ml related to peripheral arterial disease (greater, n = 110 or lower, n = 40 than 165.8 ± 1 pg/ml) found by ROC curve analysis (Fig. 1).
Chi-square test showed significant association between PAD manifestation and high MCP-1 serum concentrations (x2 = 9.6, p = 0.001, Fig. 2). Moreover, the built logistic regression analysis for PAD prediction showed that the high MCP-1 serum levels increased the risk for PAD demonstration 3.2 (95% C.I 1.3–8.2) folds after adjustment for confounders including the age, smoking, dialysis vintage, hypertension, dialysis adequacy defined by spKt/V for urea, serum bicarbonate and hsCRP (Table 2).
We also observed that the existence of PAD was significantly associated with coronary artery disease, left ventricular hypertrophy, hypertension and with non-administration of vitamin D agents during dialysis (x2 = 23.2, p = 0.001 Fig. 3, x2 = 5.3, p = 0.01, x2 = 4.5, p = 0.02 and x2 = 3.5, p = 0.04, respectively). The association between PAD demonstration and pharmaceutical therapy by statin was found to be non-significant.
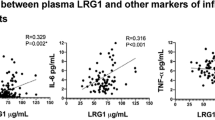
Bivariate correlations showed significant association between MCP-1 levels and both LDL/HDL ratio and percent sodium removal (r = 0.212, p = 0.009 and r = −0.286, p = 0.001, respectively). Particularly, in group of patients with PAD (n = 61) the correlation between MCP-1 levels and LDL/HDL ratio was also found to be significant (r = 0.435, p = 0.001), although the correlation between MCP-1 levels and hsCRP serum concentrations was found to be non-significant in both groups of patients with and without existence of PAD, as well as in total of our subjects.
Discussion
It has been reported that PAD is significantly elevated among patients on hemodialysis in comparison to general population. Using a set of clinical criteria showing signs of limb ischemia including reduced pulses on examination or symptomatic claudication and the determination of ABI as a diagnostic key, the prevalence rate of PAD was reported nearly 35% [19, 20]. Other previous study reported that 46% of all dialysis patients in the United States suffered from PAD [21].
In this study, the prevalence rate of PAD was evaluated in a ratio of 40.7%, using clinical criteria, ABI measurement and determination of vascular stenosis in the lower limbs >50% by Doppler ultrasound.
Despite angiography was considered as the gold standard method for PAD diagnosis, recent guidelines recommended that subjects with claudication should be first screened by using noninvasive Doppler ultrasonography [22]. Clinical criteria of PAD including claudication are usually unreliable signs of PAD especially in aging dialysis patients due to degenerative changes in lumbar and peripheral joints caused by the renal disease and advancing age. Furthermore, the presence or absence of pulses in lower extremities during clinical examination is usually unreliable due to collateral development. On the other hand, the sensitivity of ABI, the major diagnostic key for PAD determination, is limited to outline PAD, when arterial stiffness is present, such as in dialysis patients [23, 24]. As a result, ABI values may be elevated to “falsely normal” or even abnormally high values (>1.4), despite the existence of PAD. In this study, PAD diagnosis was mostly based on the report of Doppler ultrasound examination and less in clinical criteria or ABI values. Indeed, our participants with manifested PAD by Doppler screening had non-significantly lower ABI values than the patients without PAD.
Systemic atherosclerosis and cardiovascular disease including PAD in this population of patients are mainly affected by non-traditional risk factors including persistent low-grade inflammation, metabolic acidosis, volume overload and co-morbidities. Arterial stiffness, oxidative stress, insulin resistance, hyperphosphatemia, hypoalbuminemia are characteristics which may contribute to prevalent PAD among patients on dialysis [11, 21, 25].
In agreement, in this study, we observed that the patients with PAD manifestation were elder and they had elevated hsCRP and MCP-1 serum concentrations as markers of inflammation, higher BP and higher arterial stiffness markers including c-fPWV, Aix, and PP than the patients without PAD. They also had higher markers of malnutrition, such as lower albumin, LDL/HDL and lower nPCR, uncontrolled metabolic acidosis and exciting markers of bone disease including low i-PTH in comparison to the patients without PAD. Despite the group of patients with PAD had lower LDL/HDL levels comparatively to the patients without PAD, the association between using of statin and PAD manifestation was found to be non-significant. The lower LDL/HDL levels in our patients with PAD may be mainly attributed to malnutrition status in this group of patients rather than to other causes including the statin therapy. The obtained adequacy of dialysis treatment was lower in patients with PAD than the patients without PAD, as this is defined by a lower spKt/V for urea and by higher sodium retention in combination to lower urine output.
These findings suggest the co-occurrence of malnutrition, inflammation, and atherosclerosis (MIA syndrome), in comparison to the patients without manifested PAD. Malnutrition has already been reported as specific cardiovascular risk factor for dialysis patients and each of MIA syndrome components worsens the morbidity and survival of these patients [26, 27]. The cause of inflammation is multifactorial and include imbalance between increased production and decreased removal of pro-inflammatory cytokines, oxidative stress, factors linked to dialysis treatment and chronic and recurrent infections related to dialysis access [28]. Malnutrition may also be related to metabolic acidosis due to an increased protein catabolism, decreased protein synthesis, endocrine abnormalities and inflammation among dialysis patients [11, 29]. Metabolic acidosis defined by low serum bicarbonate (<22 mmol/l) results in inflammatory stimulation, lipids oxidation and oxidative stress in ESRD patients [30]. Maintenance dialysis therapies are often unable to completely correct the base deficit.
Regarding with markers of bone disease previously it has been reported that low i-PTH was associated with inflammation and oxidative stress rather than high, as a result of MIA Syndrome in agreement with our results [31]. Interestingly, the most of our subjects, who were receiving vitamin D supplementation during dialysis sessions, did not have manifested PAD. However, the bone disease markers including serum phosphate, Ca × P products and i-PTH were found to mildly differ between the groups of patients with and without PAD. Such findings could suggest that the administration of vitamin D during dialysis may affect the manifestation of PAD in these patients playing an additional role rather than on the regulation of bone disease. Recently, we and others reported that the usage of vitamin D derivatives in chronic kidney disease patients may prevent the elevated production of reactive oxygen species and the cytokines upregulation by serum phosphate resulting in beneficial cardiovascular effects [32, 33].
In combination with the important role of MIA syndrome, it has been established that arterial stiffness and vascular calcification are non-traditional cardiovascular risk factors in chronic kidney disease resulting in coronary arterial disease, heart failure and peripheral vascular disease in agreement with our findings [34].
MCP-1, the main representative of chemokines, may be related to low-grade inflammation in the patients undergoing hemodialysis. However, in both groups of our subjects with and without PAD and in the total of our participants we observed a non-significant correlation between MCP-1 levels and hsCRP serum concentrations, which is the established marker of inflammation. MCP-1 acts as a chemoattractant specific for monocytes and may promote migration of monocytes into the atherosclerotic plaque after their initial adhesion to the endothelium, playing a particular role on the lesions of atherogenesis [35]. In this study, apart from the found higher MCP-1 levels in our participants with PAD than without PAD, we noted significant unadjusted association between manifested PAD and high levels of MCP-1. Moreover, the high MCP-1 serum concentrations were shown to be an important predictor for PAD with an odds ratio of 3.2 (95% C.I 1.3–8.3) adjusting for traditional and specific for these patients confounders.
Previously, it has been reported that serum levels of soluble intracellular cell adhesion molecule-1 (sICAM-1) and soluble vascular cell adhesion molecule-1 (sVCAM) were associated with PAD in dialysis patients, but MCP-1 serum concentrations were not associated controversially to our findings [6].
Furthermore, in this study we observed a significantly positive association between MCP-1 and LDL/HDL. The correlation between MCP-1 and LDL/HDL was noted positive particularly in group of patients with PAD, despite in this group of patients LDL/HDL levels were found to be significantly lower than in non-PAD group of patients, due mainly to excessive malnutrition and inflammation syndrome connected to the existence of PAD. Previous study reported that LDL-apheresis reduced the plasma levels of P-selectin, hsCRP and fibrinogen through anti-inflammatory effects, but serum levels of MCP-1 were not significantly changed suggesting a stable relationship of MCP-1 with LDL, in agreement with our results [7].
On the other hand, in our study the relationship between MCP-1 and sodium removal was found inverse supporting a relation between MCP-1 and fluid overload. In our previous study excluding the diabetic nephropathy, such as in present study, we also observed a significant role of MCP-1 serum concentrations on the left ventricular hypertrophy mainly attributed to the relationship between MCP-1 and sodium retention [36]. It has been reported that frequently volume overloaded hemodialysis patients are at high risk of endothelial dysfunction, hypertension, left ventricular hypertrophy, CHF and vascular disease [37]. Indeed, in our study, in conjunction to the found significant association between PAD manifestation and high MCP-1 levels, we noted significant associations between PAD and both hypertension and left ventricular hypertrophy. Moreover, in our data we notified the established significant relationship between PAD and coronary artery disease [1, 2].
The findings of this study could suggest that MCP-1 levels may be used as screening markers for PAD in dialysis patients. However, more studies should verify such as recommendation.
Conclusion
This study showed that malnutrition, low-grade inflammation mainly defined by high MCP-1 serum concentrations, metabolic acidosis and bone disease were included in significant predictors for PAD in non-diabetic patients undergoing permanent hemodiafiltration. The obtained dialysis sufficiency and the administrated therapy during dialysis sessions including vitamin D supplementation seem to play an additional role in the demonstration of peripheral vascular disease in these patients.
References
Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FG, et al. Inter-society consensus for the management of peripheral arterial disease. Int Angiol. 2007;26:81–157.
Banchs Viña H, Claudio H, Mesa M, López-Candales A. Diagnostic studies for the evaluation of peripheral artery disease. Bol Asoc Med P R. 2015;107:42–5.
Schwartz SM, Heimark RL, Majesky MW. Developmental mechanisms underlying pathology of arteries. Physiol Rev. 1990;70:1177–209.
Sarnak MJ, Levey AS, Schoolwerth AC, Coresh J, Culleton B, Hamm LL, et al. Kidney disease as a risk factor for development of cardiovascular disease: a statement from the American Heart Association Councils on Kidney in Cardiovascular Disease, High Blood Pressure Research, Clinical Cardiology, and Epidemiology and Prevention. Hypertension. 2003;42:1050–65.
O’Hare AM, Glidden DV, Fox CS, Hsu CY. High prevalence of peripheral arterial disease in persons with renal insufficiency: results from the National Health and Nutrition Examination Survey 1999-2000. Circulation. 2004;109:320–3.
Cheng CH, Chen YS, Shu KH, Chang HR, Chou MC. Higher serum levels of soluble intracellular cell adhesion molecule-1 and soluble vascular cell adhesion molecule predict peripheral artery disease in haemodialysis patients. Nephrology. 2012;17:718–24.
Kobayashi S, Oka M, Moriya H, Maesato K, Okamoto K, Ohtake T. LDL-apheresis reduces P-Selectin, CRP and fibrinogen -- possible important implications for improving atherosclerosis. Ther Apher Dial. 2006;10:219–23.
Chauveau P, Nguyen H, Combe C, Chêne G, Azar R, Cano N. et al. Dialyzer membrane permeability and survival in hemodialysis patients. Am J Kidney Dis2005;45:565–71.
Daugirdas JT. Second generation logarithmic estimates of single-pool variable volume Kt/V: an analysis of error. J Am Soc Nephrol. 1993;4:1205–13.
Raikou VD, Kardalinos V, Kyriaki D. The relationship of residual renal function with cardiovascular morbidity in hemodialysis patients and the potential role of monocyte chemoattractant protein-1. Kidney Dis. 2018;4:20–28.
Raikou V, Kyriaki D. Association between low serum bicarbonate concentrations and cardiovascular disease in patients in the end-stage of renal disease. Diseases. 2016;4:36.
Raikou V, Tentolouris N, Despina Kyriaki D, Evaggelatou A, Tzanatou H. β2-Microglobulin, pulse pressure and metabolic alterations in hemodialysis patients. Nephron Clin Pract. 2011;117:c237–c245.
Kirschbaum B. Spuriousmetabolic acidosis in hemodialysis patients. Am J Kidney Dis. 2000;35:1068–71.
Daugirdas JT. Simplified equations for monitoring Kt/V, PCRn, eKt/V, and ePCRn. Adv Ren Replace Ther. 1995;2:295–304.
Verim S, Taşçı I. Doppler ultrasonography in lower extremity peripheral arterial disease. Arch Turk Soc Cardiol. 2013;41:248–55.
Han SS, Cho GY, Park YS, Baek SH, Ahn SY, Kim S, et al. Predictive value of echocardiographic parameters for clinical events in patients starting hemodialysis. J Korean Med Sci. 2015;30:44–53.
Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, Smiseth OA, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. J Am Soc Echocardiogr. 2009;22:107–33.
Sharma R, Pellerin D, Gaze DC, Mehta RL, Gregson H, Streather CP, et al. Mitral peak Doppler E-wave to peak mitral annulus velocity ratio is an accurate estimate of left ventricular filling pressure and predicts mortality in end-stage renal disease. J Am Soc Echocardiogr. 2006;19:266–73.
Tasci I, Verim S, Kabul HK, Aydogdu A. Ankle brachial index as a predictor of subclinical atherosclerosis in the elderly. Int J Cardiol. 2012;160:147.
Rajagopalan S, Dellegrottaglie S, Furniss AL, Gillespie BW, Satayathum S, Lameire N, et al. Peripheral arterial disease in patients with end-stage renal disease: observations from the Dialysis Outcomes and Practice Patterns Study (DOPPS). Circulation. 2006;114:1914–22.
Cooper BA, Penne EL, Bartlett LH, Pollock CA. Protein malnutrition and hypoalbuminemia as predictors of vascular events and mortality in ESRD. Am J Kidney Dis. 2004;43:61–66.
Creager MA, Belkin M, Bluth EI, Casey DE Jr, Chaturvedi S, Dake MD, et al. 2012 ACCF/AHA/ACR/SCAI/SIR/STS/ SVM/SVN/SVS key data elements and definitions for peripheral atherosclerotic vascular disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Clinical Data Standards (Writing Committee to Develop Clinical Data Standards for Peripheral Atherosclerotic Vascular Disease). Circulation. 2012;125:395–467.
Alahdab F, Wang AT, Elraiyah TA, Malgor RD, Rizvi AZ, Lane MA, et al. A systematic review for the screening for peripheral arterial disease in asymptomatic patients. J Vasc Surg. 2015;61(3 Suppl):42S–53S.
Leskinen Y, Salenius JP, Lehtimäki T, Huhtala H, Saha H. The prevalence of peripheral arterial disease and medial arterial calcification in patients with chronic renal failure: requirements for diagnostics. Am J Kidney Dis. 2002;40:472–9.
Boaz M, Weinstein T, Matas Z, Green MS, Smetana S. Peripheral vascular disease and serum phosphorus in hemodialysis: a nested case-control study. Clin Nephrol. 2005;63:98–105.
Jahromi SR, Hosseini S, Razeghi E, Meysamie Ap, Sadrzadeh H. Malnutrition predicting factors in hemodialysis patients. Saudi J Kidney Dis Transpl.2010;21:846–51.
Stenvinkel P. Inflammatory and atherosclerotic interactions in the depleted uremic patient. Blood Purif. 2001;19:53–61.
Dai L, Golembiewska E, Lindholm B, Stenvinkel P. End-stage renal disease, inflammation and cardiovascular outcomes. Contrib Nephrol.. 2017;191:32–43.
de Oliveira CM, Vidal CL, Cristino EF, Pinheiro FM Jr, Kubrusly M. Metabolic acidosis and its association with nutritional status in hemodialysis. J Bras Nefrol. 2015;37:458–66.
Kalantar-Zadeh K, Mehrotra R, Fouque D, Kopple JD. Metabolic acidosis and malnutrition-inflammation complex syndrome in chronic renal failure. Semin Dial. 2004;17:455–65.
Pecoits-Filho R, Lindholm B, Stenvinkel P. The malnutrition, inflammation, and atherosclerosis (MIA) syndrome-the heart of the matter. Nephrol Dial Transplant. 2002;17:28–31.
Martínez-Moreno JM, Herencia C, de Oca AM, Díaz-Tocados JM, Vergara N, Gómez-Luna MJ, et al. High phosphate induces a pro-inflammatory response by vascular smooth muscle cells and modulation by vitamin D derivatives. Clin Sci. 2017;131:1449–63.
Raikou V, Kardalinos V, Kyriaki D. Oxidized low-density lipoprotein serum concentrations and cardiovascular morbidity in end stage of renal disease. J Cardiovasc Dev Dis. 2018;5:35.
Larivière R, Gauthier-Bastien A, Ung RV, St-Hilaire J, Mac-Way F, Richard DE, et al. Endothelin type A receptor blockade reduces vascular calcification and inflammation in rats with chronic kidney disease. J Hypertens. 2017;35:376–84.
Coll B, Alonso-Villaverde C, Joven J. Monocyte chemoattractant protein-1 and atherosclerosis: Is there room for an additional biomarker? Clin Chim Acta. 2007;383:21–9.
Raikou VD, Moisakis J, Kyriaki D. Correlation between MCP-1 (monocyte chemoattractant protein-1) and cardiovascular disease in patients on the end stage of renal disease. Am J Pharmacol Pharmacotherapeut. 2014;1:127–33.
Voroneanu L, Cusai C, Hogas S, Ardeleanu S, Onofriescu M, Nistor I, et al. The relationship between chronic volume overload and elevated blood pressure in hemodialysis patients: use of bioimpedance provides a different perspective from echocardiography and biomarker methodologies. Int Urol Nephrol. 2010;42:789–97.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Institutional review board (IRB)/Ethics Committee with an obtained IRB number E.S.931/5-12-2006 of the Hospitals “Laiko, University General Hospital of Athens” and Renal Unit of “Diagnostic and Therapeutic Center of Athens Hygeia SA”.
Informed consent
Oral informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Raikou, V.D., Kyriaki, D. Factors related to peripheral arterial disease in patients undergoing hemodialysis: the potential role of monocyte chemoattractant protein-1. Hypertens Res 42, 1528–1535 (2019). https://doi.org/10.1038/s41440-019-0259-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-019-0259-x