Abstract
Although beneficial antihypertensive and antialbuminuric effects of steroidal mineralocorticoid receptor (MR) antagonists have been shown, the use of these drugs has been clinically limited in diabetic kidney disease (DKD) because of the high incidence of side effects. Here, we aimed to examine the effect of a novel nonsteroidal selective mineralocorticoid receptor antagonist, esaxerenone, on blood pressure and renal injury in high salt-treated type 2 diabetic KK-Ay mice, a model of human hypertensive DKD. KK-Ay mice were treated with a normal salt diet (NS: 0.3% NaCl, n = 5), high salt diet (HS: 4% NaCl, n = 8), HS + esaxerenone (1 mg/kg/day, p.o., n = 8), or HS + spironolactone, a steroidal non-selective MR antagonist (20 mg/kg/day, p.o., n = 7) for 8 weeks. Renal tissue oxidative stress was evaluated by dihydroethidium florescence intensity. HS-treated diabetic KK-Ay mice showed higher blood pressure and severe albuminuria, glomerular injury, tubulointerstitial fibrosis, renal inflammation, and oxidative stress than NS-treated diabetic KK-Ay mice. Treatment with esaxerenone or spironolactone decreased blood pressure to a similar extent in HS-treated KK-Ay mice. Conversely, esaxerenone elicited a greater attenuation of albuminuria, glomerular injury, tubulointerstitial fibrosis, and renal inflammation than spironolactone, which were associated with reduction in renal oxidative stress. These data indicate for the first time that a nonsteroidal MR antagonist elicits renoprotective effects in DKD mice.
Similar content being viewed by others
Introduction
A growing body of evidence indicates that aldosterone and mineralocorticoid receptor (MR) play an important role in the pathophysiology of renal injury, including renal inflammation, oxidative stress, fibrosis, mesangial cell proliferation and podocyte injury [1,2,3]. Clinical studies have also shown that aldosterone blockade with available steroidal MR antagonists, spironolactone or eplerenone, elicits antiproteinuric effects in patients with chronic kidney disease [4, 5]. However, clinical use of these available steroidal MR antagonists is limited because they increase the risk of hyperkalemia and worsen renal function, especially in patients with diabetic kidney disease (DKD) [6,7,8].
To overcome these limitations, nonsteroidal MR antagonists are currently being developed (NCT02345044, 02345057, 02448628, 02517320, 02540993, 02676401). Compared with steroidal MR antagonists, nonsteroidal MR antagonists have different physicochemical and tissue distribution properties [9,10,11]. Pharmacokinetics studies have also shown that selective nonsteroidal MR antagonists elicit higher selectivity and greater binding affinity against MR than spironolactone and eplerenone, respectively [9, 11]. Moreover, clinical studies have shown that nonsteroidal MR antagonists confer a lower risk of hyperkalemia [9, 12,13,14]. Bakris et al. [15] showed that treatment with the nonsteroidal MR antagonist finerenone significantly decreased albuminuria and blood pressure in patients with DKD (type 2 diabetic nephropathy and albuminuria > 30 mg/g creatinine) who were treated with angiotensin converting enzyme inhibitor or angiotensin receptor antagonist. Similarly, in DKD patients who were treated with inhibitors of renin-angiotensin system, treatment with finerenone [16] significantly decreased albuminuria without adverse effects on serum potassium and renal function. Nevertheless, it is still not clear whether nonsteroidal MR antagonists attenuate renal tissue injury and improve renal outcome during the progression of DKD.
Recent studies in non-diabetic animal models have shown that nonsteroidal MR antagonists are able to prevent the progression of renal tissue injury [17,18,19,20]. However, the renoprotective effect of nonsteroidal MR antagonists has not been examined in DKD animals. One of the experimental difficulties for DKD model studies is that diabetic mice fail to show severe glomerular and tubulointerstitial injuries [21, 22]. In this regard, we have recently demonstrated that high salt (HS)-treated type 2 diabetic KK-Ay mice develop severe hypertension, albuminuria, glomerular injury and tubulointerstitial fibrosis, which mimics human DKD with hypertension [23]. In the present study, we aimed to examine the effects of the novel nonsteroidal MR antagonist esaxerenone [11] on renal injury in HS-treated type 2 diabetic KK-Ay mice.
Materials and methods
Animals
All experimental procedures were performed according to the guidelines for the care and use of animals as established by Kagawa University. The experiments were approved by the Animal Experimentation Ethics Committee at Kagawa University (A84: 18625). Six-week-old male KK-Ay mice, a genetic mouse model of type 2 diabetes with obesity [23, 24], and control non-diabetic C57BL/6 mice were sourced from CLEA Japan Inc. (Tokyo, Japan). Mice were maintained in a pathogen-free facility under controlled temperature (24 ± 2 °C) and humidity (55 ± 5%), with a 12-h light/dark cycle.
Experimental protocols
After 1 week of acclimatization and baseline data collection, C57BL/6 mice were randomly divided into the following four 8-week treatments (n = 6 in each group): (1) normal salt (NS: 0.3% NaCl, Oriental Yeast, Tokyo, Japan) diet and vehicle (carboxymethyl cellulose), C57BL/6 + NS; (2) HS diet (4% NaCl, Oriental Yeast) and vehicle, C57BL/6 + HS; (3) HS diet and esaxerenone (EXR; 1 mg/kg/day by oral gavage (p.o.); Daiichi-Sankyo Co., Ltd., Tokyo, Japan), C57BL/6 + HS + EXR. Likewise, type 2 diabetic KK-Ay mice were divided into the following four 8-week treatments (n = 8 in each group): (1) NS diet and vehicle, KK-Ay + NS; (2) HS diet and vehicle, KK-Ay + HS; (3) HS and esaxerenone (1 mg/kg/day, p.o.), KK-Ay + HS + EXR; (4) HS diet and spironolactone (20 mg/kg/day, p.o.), KK-Ay + HS + SPL. Doses of EXR and SPL were determined on the basis of previous studies [10, 11, 17,18,19,20]. Our preliminary experiments also confirmed that EXR (1 mg/kg/day, p.o.) and SPL (20 mg/kg/day, p.o.) similarly decreased blood pressure in salt-treated KK-Ay mice (data not shown). We also confirmed that SPL (1 mg/kg/day, p.o.) did not change blood pressure in these animals (data not shown).
Systolic blood pressure (SBP) was measured by tail-cuff plethysmography (BP-98A; Softron Co., Tokyo, Japan) at baseline and every alternate week. Twenty-four-hour urine samples were collected at baseline and every alternate week. All mice underwent a 12-h acclimatization period in metabolic cages prior to urine collection. Urinary albumin and creatinine concentrations were measured using assay kits (Code No. AKRAL-120, Shibayagi Co., Shibukawa, Japan, and micro CRE-test; Wako Co., Ltd., Osaka, Japan), respectively [24, 25]. Urinary Na+ and K+ concentrations were determined by flame photometry (EFOX 5053; Eppendorf Co., Burladingen, Germany). Fasting blood glucose (FBG) was measured with a glucometer (Sanwa-Kagaku, Nagoya, Japan).
Sample collection
At the end of the experiment, animals were fasted for 18 hours and anesthetized with isoflurane. Then, blood was collected in EDTA-containing tubes for measuring fasting plasma insulin (AKRIN-011S; Shibayagi Co.). Thereafter, animals were euthanized with an overdose of pentobarbital (250 mg/kg, i.p.) and the kidneys were harvested. The kidney tissues were cut and fixed in 10% buffered paraformaldehyde, embedded in Tissue-Tek OCT compound (Sakura Finetech, Tokyo, Japan), or snap-frozen in liquid nitrogen. Small samples of renal cortical tissue were collected in RNAlater (Thermo Fisher Scientific K.K., Waltham, MA, USA) and kept at 4 °C overnight. RNAlater-treated samples were then snap-frozen in liquid nitrogen and stored at −80 °C until processing for RNA extraction and reverse transcription-polymerase chain reaction (RT-PCR) analysis.
Histopathologic and immunohistochemical examination
Kidney tissues fixed in 10% paraformaldehyde were embedded in paraffin, sectioned into 4-µm-thick slices, and stained with periodic acid-Schiff (PAS) or Azan reagent to evaluate glomerular sclerosis and tubulointerstitial fibrosis, respectively. The percentage of PAS-positive areas in each experimental group was measured using WinROOF image measurement software (Mitani Corp., Tokyo, Japan). A total of 20–25 glomeruli were examined for each mouse and the average percentage of affected lesions was calculated for each mouse. The infiltration of mononuclear cells into the interstitium was quantified by counting mononuclear cells in 10 fields at ×400 magnification and expressed as cells/mm2 [23]. The extent of the interstitial fibrotic area was evaluated quantitatively by automatic image analysis, which determined the area occupied by interstitial tissue positive for Azan-staining as described previously [23], and analyzed using Image-Pro plus software (Media Cybernetics, Bethesda, MD, USA). All morphometric measurements were performed in a blinded manner to avoid any bias.
Dihydroethidium (DHE) staining
To evaluate reactive oxygen species in renal tissues, DHE immunofluorescence staining was performed, as previously described [23]. Fresh kidney tissues embedded in OCT immediately after sacrifice were subsequently cryosectioned (8-µm-thick sections). The sections were incubated with 10 μM DHE (Invitrogen, Carlsbad, CA, USA) in phosphate-buffered saline at 37 °C for 30 min in a light-protected humidified chamber to determine superoxide anion production in the tissues. Once DHE is oxidized to ethidium, it intercalates within DNA, staining the nucleus a fluorescent red. Images were obtained using a confocal laser-scanning fluorescence microscopy system (Radiance2100; Bio-Rad Laboratories, Hercules, CA, USA). All morphometric measurements were performed in a blinded manner to avoid any bias.
Real-time RT-PCR
The mRNA expression of genes in renal cortical tissues was analyzed by RT-PCR using a LightCycler FastStart DNA Master SYBR Green I kit and an ABI Prism 7000 Sequence Detection System (Applied Biosystems, Foster City, CA, USA) as described previously [23, 24]. The oligonucleotide primer sequences for mouse β-actin, gp91phox, p22phox, transforming Growth Factor-β1 (TGF-β), monocyte chemoattractant protein-1 (MCP-1), plasminogen activator inhibitor-1 (PAI-1), α-smooth muscle actin (α-SMA), type 1 collagen, MR, and serum and glucocorticoid-regulated kinase-1 (Sgk-1) are listed in Supplementary Table 1. All data are expressed as the relative difference to the C57BL/6 + NS group, after normalization for β-actin expression.
NADPH oxidase activity in renal tissues
NADPH oxidase-derived superoxide anion (O2−) generation was measured using lucigenin-enhanced chemiluminescence, as described previously [23]. Kidney tissues were placed in chilled phosphate-buffered saline containing protease inhibitors and homogenized at 4 °C using a micro homogenizing system (Micro Smash, TOMY MEDICO., LTD, Tokyo, Japan) to prepare a 10% tissue homogenate. The protein concentration of homogenates was measured using the Bradford protein assay kit (Bio-Rad Laboratories, Hercules, CA, USA). After centrifuging, the supernatant was transferred into a glass test tube containing lucigenin (final concentration 5 μM in Krebs-HEPES buffer). Chemiluminescence was then recorded every 30 s for 10 min with a luminescence reader (BLR-301, Aloka, Tokyo, Japan), and the readings in the last 5 min were averaged. After measurement of background lucigenin chemiluminescence, NADPH was added to a final concentration of 100 μM. Thereafter, chemiluminescence was recorded for another 10 min, and the readings in the last 5 min were averaged. To verify whether the lucigenin signal reflected O2− generation, an NADPH oxidase inhibitor, diphenylene iodonium, was added at the end of measurements (final concentration, 10 μM). In all samples, diphenylene iodonium reduced NADPH-induced increases in chemiluminescence to background levels (data not shown). The difference between the values obtained before and after adding the NADPH was calculated, and the activity of NADPH oxidase was expressed as counts per min per mg of protein.
Statistical analyses
All values in the text and figure are presented as means ± standard error of the mean. Statistical comparisons of differences among groups were performed using one-way repeated-measures analysis of variance (ANOVA), followed by the Bonferroni post hoc test. Values of P < 0.05 were considered statistically significant. Data and statistical analyses were performed using GraphPad Prism version 6 for Windows (Graph Pad Software, San Diego, CA, USA).
Results
Effects of esaxerenone and spironolactone on body weight, blood pressure, blood glucose and plasma insulin
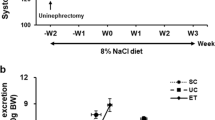
During treatment with the NS or HS diet, type 2 diabetic KK-Ay mice exhibited higher body weight compared with control C57BL/6 mice; however, this difference was not statistically significant (Fig. 1a).
Effects of esaxerenone (EXR) and spironolactone (SPL) on body weight (a), systolic blood pressure (b), fasting blood glucose (c), plasma insulin (d) and albuminuria (e). NS, normal salt diet; HS, high salt diet; UACR, Urinary albumin/creatinine ratio; C57BL/6, C57BL/6 mice; KK-Ay, KK-Ay mice. aP < 0.05 vs. KK-Ay + HS. bP < 0.05, KK-Ay + HS + EXR vs. KK-Ay + HS + SPL
KK-Ay + NS showed elevated SBP compared with age-matched C57BL/6 + NS. KK-Ay + HS exhibited further SBP elevation compared with KK-Ay + NS. Treatment with esaxerenone or spironolactone similarly decreased SBP in KK-Ay + HS (Fig. 1b).
KK-Ay mice exhibited higher FBG levels (Fig. 1c) than C57BL/6 mice. Compared with KK-Ay + NS and KK-Ay + HS, KK-Ay + HS + EXR and KK-Ay + HS + SPL showed a tendency for lower FBG levels, although these differences were not statistically significant (Fig. 1c). Similarly, KK-Ay mice exhibited higher plasma insulin levels than C57BL/6 mice. As compared with KK-Ay + HS, KK-Ay + HS + EXR and KK-Ay + HS + SPL showed a tendency for lower plasma insulin levels, although these differences were not statistically significant (Fig. 1d).
Effects of esaxerenone and spironolactone on albuminuria and the urinary Na+/K+ ratio
KK-Ay mice showed overt albuminuria, which was not further augmented by HS diet feeding. Treatment with either esaxerenone or spironolactone attenuated the development of albuminuria in KK-Ay + HS, though a greater antialbuminuric effect was elicited by esaxerenone (Fig. 1e).
HS treatment elevated the urinary Na+/K+ ratio in both C57BL/6 and KK-Ay mice. Treatment with esaxerenone or spironolactone further increased urinary Na+/K+ excretion in C57BL/6 + HS and KK-Ay + HS, respectively (data not shown).
Effects of esaxerenone and spironolactone on glomerular and tubulointerstitial injuries
At 18 weeks of age, significant glomerular injury (as assessed by an increase in the PAS-positive area in the glomeruli) as well as glomerular hypertrophy were observed in KK-Ay + NS, which were further aggravated by HS diet feeding. Both esaxerenone and spironolactone attenuated glomerular injuries in HS + KK-Ay; though a greater protective efficacy was elicited by esaxerenone (Fig. 2a–c).
Effects of esaxerenone (EXR) and spironolactone (SPL) on glomerular injury. Renal histopathological changes were evaluated by examining periodic acid-Schiff (PAS) staining. a Representative images of PAS-stained renal sections. b The PAS-positive area within total glomerular area (purple color staining). c Mean glomerular diameters expressed as fold changes with C57BL/6 group. NS, normal salt diet; HS, high salt diet; C57BL/6, C57BL/6 mice; KK-Ay, KK-Ay mice. aP < 0.05 vs. KK-Ay + HS
Tubulointerstitial fibrosis, as assessed by the Azan-positive area in the renal interstitium, was significantly increased in KK-Ay + NS (blue staining) as compared with C57BL/6 + NS (Fig. 3a, b). In addition, KK-Ay + NS showed upregulated expression of profibrotic genes such as α-SMA and type 1 collagen in renal cortical tissues (Fig. 3c, d). These detrimental changes were more pronounced following HS diet feeding in KK-Ay mice. Both esaxerenone and spironolactone attenuated tubulointerstitial fibrosis and the upregulation of profibrotic gene expression in KK-Ay + HS; though a greater protective efficacy was elicited by esaxerenone.
Effects of esaxerenone (EXR) and spironolactone (SPL) on tubulointerstitial injuries. Representative micrographs of Azan-stained renal sections (a). Quantitative analysis of Azan-positive area (purple color staining) (b). mRNA expression of α-smooth muscle actin (α-SMA) (c) and type 1 collagen (d) were quantitatively analyzed by real-time reverse transcription-polymerase chain reaction. All mRNA data are expressed as the relative difference to the C57BL/6 + NS group, after normalization for β-actin expression. NS, normal salt diet; HS, high salt diet; C57BL/6, C57BL/6 mice; KK-Ay, KK-Ay mice. aP < 0.05 vs. KK-Ay + HS
Effects of esaxerenone and spironolactone on MR-target gene expression
KK-Ay + HS showed upregulated mRNA levels of MR and MR-target genes, such as Sgk-1, in renal cortical tissues (Fig. 4a, b). Treatment with either esaxerenone or spironolactone significantly attenuated the upregulation of MR and Sgk-1 mRNA levels in renal cortical tissues of KK-Ay + HS; though greater reductions in MR and Sgk-1 gene expression were elicited by esaxerenone.
Effects of esaxerenone (EXR) and spironolactone (SPL) on mineralocorticoid receptor (MR)-target gene expression. Renal cortical tissue MR (a) and glucocorticoid-regulated kinase-1 (Sgk-1, b) mRNA levels were determined by real-time reverse transcription-polymerase chain reaction. All mRNA data are expressed as the relative difference to the C57BL6 + NS group, after normalization for β-actin expression. NS, normal salt diet; HS, high salt diet; C57BL/6, C57BL/6 mice; KK-Ay, KK-Ay mice. aP < 0.05 vs. KK-Ay + HS
Effects of esaxerenone and spironolactone on renal inflammation
KK-Ay + NS showed significant infiltration of mononuclear cells into the renal interstitial space while C57BL/6 + NS did not (Fig. 5a). Cellular infiltration was associated with increases in renal cortical tissue mRNA levels of proinflammatory cytokines, such as TGF-β, MCP-1, and PAI-1 (Fig. 5b–d). Treatment with either esaxerenone or spironolactone significantly attenuated inflammatory cell accumulation and decreased mRNA levels of proinflammatory cytokines in KK-Ay + HS, though a greater attenuation was elicited by esaxerenone.
Effects of esaxerenone (EXR) and spironolactone (SPL) on renal inflammation. The number of mononuclear cells in the interstitial space of the kidney was quantified (a). Renal cortical tissue mRNA levels of transforming Growth Factor-β1 (TGF-β, b), monocyte chemoattractant protein-1 (MCP-1, c), and plasminogen activator inhibitor-1 (PAI-1, d) were determined by real-time reverse transcription-polymerase chain reaction. All mRNA data are expressed as the relative difference to the C57BL/6 + NS group, after normalization for β-actin expression. NS, normal salt diet; HS, high salt diet; C57BL/6, C57BL/6 mice; KK-Ay, KK-Ay mice. aP < 0.05 vs. KK-Ay + HS
Effects of esaxerenone and spironolactone on renal oxidative stress
Renal oxidative stress was evaluated by DHE immunohistochemistry and NADPH oxidase activity. DHE staining was significantly increased in kidneys of KK-Ay + NS as compared with those of C57BL/6 + NS (Fig. 6a, b). Renal DHE staining was further increased by the HS diet in KK-Ay mice. Treatment with either esaxerenone or spironolactone attenuated the increase in DHE staining in KK-Ay + HS, though a greater reduction in DHE staining was elicited by esaxerenone.
Effects of esaxerenone (EXR) and spironolactone (SPL) on renal oxidative stress. Representative images of dihydroethidium (DHE) immunofluorescence staining (original magnification, ×200) (a). DHE fluorescence intensity (b). NADPH oxidase activity in homogenized renal cortical tissues (c). Renal cortical tissue gp91phox (d), and p22phox (e) mRNA levels were determined by real-time reverse transcription-polymerase chain reaction. All mRNA data are expressed as the relative difference to the C57BL/6 + NS group, after normalization for β-actin expression. NS, normal salt diet; HS, high salt diet; C57BL/6, C57BL/6 mice; KK-Ay, KK-Ay mice. aP < 0.05 vs. KK-Ay + HS
Increased DHE staining in renal tissues was associated with increases in NADPH oxidase activity and upregulation of NADPH oxidase components, gp91phox and p22phox expression, in KK-Ay + NS, which were further upregulated by HS feeding (Fig. 6c–e). Treatment with either esaxerenone or spironolactone attenuated the increases in NADPH oxidase activity and mRNA levels of gp91phox and p22phox in KK-Ay + HS. In this group, increased NADPH oxidase activity and NADPH oxidase subunit genes expression were prevented by treatment with esaxerenone, but only partially prevented by spironolactone. These data suggest that the renal protective effects of esaxerenone were associated with an attenuation of oxidative stress in the kidney.
Discussion
Hypertension is often associated with the development of DKD [26]. Although steroidal MR antagonists are frequently used for treatment of resistant hypertension [3, 27]; the use of these drugs has been clinically limited because of the high incidence of side effects particularly in DKD patients [6,7,8]. In the present study, we examined the effect of a novel nonsteroidal selective MR antagonist, esaxerenone [11], on blood pressure and renal injury in HS-treated type 2 diabetic KK-Ay mice, which mimic human DKD with hypertension [23]. The results showed that treatment with esaxerenone markedly attenuated the development of hypertension and albuminuria in HS-treated KK-Ay mice. Furthermore, esaxerenone prevented the progression of renal tissue injury, which was associated with an attenuation of renal inflammation and oxidative stress. These data indicate for the first time that a nonsteroidal MR antagonist elicits beneficial effects on blood pressure control and renal injury in DKD mice.
Effects of nonsteroidal MR antagonists have not been examined in animal models of DKD, probably because of the lack of reliable animal models [21, 22]. Recently, we demonstrated that HS-treated type 2 diabetic KK-Ay mice develop hypertension and albuminuria, as well as severe renal tissue damage including glomerular injury and tubulointerstitial fibrosis, which mimics human DKD with hypertension [23]. Consistent with previous observations [23, 24], the present study showed that obese type 2 diabetic KK-Ay mice had hypertension and albuminuria, as well as significant glomerular and tubulointerstitial damage. The pathological features of renal tissue injury were further aggravated by HS diet treatment. Using this model, the present study demonstrated, for the first time, that a nonsteroidal MR antagonist has beneficial effects on blood pressure control, albuminuria and renal tissue injury in hypertensive DKD mice, which suggests this nonsteroidal MR antagonist may confer a therapeutic advantage for hypertensive patients with DKD.
Oxidative stress is a major contributing factor to the pathophysiology of salt-induced hypertension [28] and renal injury [29], which are associated with increases in renal NADPH activity [30]. We have previously shown that chronic treatment with aldosterone and salt stimulates renal oxidative stress through the activation of MR [30]. However, recent studies have also shown that HS decreases aldosterone production but induces ligand-independent Rac1-mediated MR activation in the kidney, which contributes to the development of salt-induced hypertension and renal injury [31, 32]. Further studies indicated a potential contribution of oxidative stress to activating Rac-1-mediated MR [33]. In agreement with previous studies [23], the present study showed that HS diet-treated KK-Ay mice had marked increases in renal oxidative stress markers, such as renal tissue DHE staining, NADPH oxidase activity and mRNA levels of NADPH oxidase subunits, which were associated with renal tissue injury. We also showed that the renoprotective effects of esaxerenone were accompanied by a reduction in renal oxidative stress. Likewise, recent studies have shown that the nonsteroidal MR antagonist finerenone exerts its renoprotective effects through suppression of oxidative stress in non-diabetic chronic kidney disease mice [17, 18]. Although the present study failed to measure actual MR activity and oxidative stress in each nephron segment, it is possible that the renoprotective effects of MR blockade with esaxerenone are mediated at least in part by its antioxidative properties.
In KK-Ay mice, a HS diet elevated gene expression of proinflammatory cytokines such as MCP-1 and PAI-1. Interestingly, these inflammatory changes were significantly attenuated by treatment with esaxerenone. Studies have shown that activated macrophages secrete profibrotic molecules such as TGF-β1, which play a role in epithelial-mesenchymal transition, resulting in the appearance of interstitial myofibroblasts [34]. These myofibroblasts express α-SMA and synthesize large amounts of extracellular matrix proteins, including collagens [34]. Indeed, renoprotective effects of selective MR blockade with esaxerenone were accompanied by attenuation of renal inflammation and profibrotic changes. In this regard, Huang et al. [35] showed that specific gene deletion of MR in macrophages elicits anti-glomerular basement membrane glomerulonephritis. These data suggest that renal inflammation via macrophage MR activation is a potential therapeutic target of esaxerenone during the progression of renal injury. The finding that these effects of esaxerenone were associated with a reduction in renal oxidative stress suggests the potential contribution of an antioxidative effect to the attenuation of renal inflammation and profibrotic changes induced by esaxerenone treatment. However, the cause and effect relationships among renal inflammation, profibrotic changes, and oxidative stress remain unclear.
The present study showed that spironolactone reduced blood pressure to a similar extent to esaxerenone in HS-fed KK-Ay mice. Furthermore, esaxerenone and spironolactone showed a tendency to lower FBG and plasma insulin levels, although these differences were not statistically significant. Conversely, esaxerenone exhibited greater renoprotective effects compared with spironolactone, suggesting that the renoprotective effects of esaxerenone are independent of changes in blood pressure and glucose metabolism. However, it is unclear why the renoprotective and antioxidative effects of esaxerenone are greater than those of spironolactone. Although differences in their selectivity/binding affinity for MR and/or tissue distribution may play a role [9, 12,13,14], a limitation of this study is that 24-h blood pressure was not measured using a telemetry system. Thus, further studies are needed to examine the effects of esaxerenone and spironolactone on 24-h blood pressure in HS-treated KK-Ay mice. Since recent clinical studies have shown that treatment with a nonsteroidal MR antagonist, finerenone, significantly decreased albuminuria in patients with type 2 DKD who were treated with angiotensin converting enzyme inhibitor or angiotensin receptor antagonist [14,15,16], further studies are also need to examine the effects of the combination of esaxerenone and angiotensin converting enzyme inhibitor or angiotensin receptor antagonist in HS-treated KK-Ay mice.
In conclusion, the present study showed that esaxerenone, a selective nonsteroidal MR antagonist, elicits strong antihypertensive and renoprotective effects through suppression of renal inflammation and oxidative stress in HS-treated KK-Ay mice. These data indicate for the first time that nonsteroidal MR antagonists could be promising agents for blood pressure control and renal protection in hypertensive patients with DKD.
References
Nishiyama A, Hasegawa K, Diah S, Hitomi H. New approaches to blockade of the renin-angiotensin-aldosterone system: mineralocorticoid-receptor blockers exert antihypertensive and renoprotective effects independently of the renin-angiotensin system. J Pharmacol Sci. 2010;113:310–4.
Nishiyama A, Hitomi H, Rahman A, Kiyomoto H. Drug discovery for overcoming chronic kidney disease (CKD): pharmacological effects of mineralocorticoid-receptor blockers. J Pharmacol Sci. 2009;109:1–6.
Shibata S, Ishizawa K, Uchida S. Mineralocorticoid receptor as a therapeutic target in chronic kidney disease and hypertension. Hypertens Res. 2017;40:221–5.
Ando K, Ohtsu H, Uchida S, Kaname S, Arakawa Y, Fujita T, EVALUATE Study Group. Anti-albuminuric effect of the aldosterone blocker eplerenone in non-diabetic hypertensive patients with albuminuria: a double-blind, randomised, placebo-controlled trial. Lancet Diabetes Endocrinol. 2014;2:944–53.
Kato S, Maruyama S, Makino H, Wada J, Ogawa D, Uzu T, et al. Anti-albuminuric effects of spironolactone in patients with type 2 diabetic nephropathy: a multicenter, randomized clinical trial. Clin Exp Nephrol. 2015;19:1098–106.
Van Buren PN, Adams-Huet B, Nguyen M, Molina C, Toto RD. Potassium handling with dual renin-angiotensin system inhibition in diabetic nephropathy. Clin J Am Soc Nephrol. 2014;9:295–301.
Hou J, Xiong W, Cao L, Wen X, Li A. Spironolactone add-on for preventing or slowing the progression of diabetic nephropathy: a meta-analysis. Clin Ther. 2015;37:2086–103.
Mavrakanas TA, Gariani K, Martin PY. Mineralocorticoid receptor blockade in addition to angiotensin converting enzyme inhibitor or angiotensin II receptor blocker treatment: an emerging paradigm in diabetic nephropathy: a systematic review. Eur J Intern Med. 2014;25:173–6.
Dojki FK, Bakris G. Nonsteroidal mineralocorticoid antagonists in diabetic kidney disease. Curr Opin Nephrol Hypertens. 2017;26:368–74.
Arai K, Homma T, Morikawa Y, Ubukata N, Tsuruoka H, Aoki K, et al. Pharmacological profile of CS-3150, a novel, highly potent and selective non-steroidal mineralocorticoid receptor antagonist. Eur J Pharmacol. 2015;761:226–34.
Yamada M, Takei M, Suzuki E, Takakusa H, Kotsuma M, Washio T, et al. Pharmacokinetics, distribution, and disposition of esaxerenone, a novel, highly potent and selective non-steroidal mineralocorticoid receptor antagonist, in rats and monkeys. Xenobiotica. 2017;47:1090–103.
Kato M, Furuie H, Shimizu T, Miyazaki A, Kobayashi F, Ishizuka H. Single- and multiple-dose escalation study to assess pharmacokinetics, pharmacodynamics and safety of oral esaxerenone in healthy Japanese subjects. Br J Clin Pharmacol. 2018;84:1821–9.
Pei H, Wang W, Zhao D, Wang L, Su GH, Zhao Z. The use of a novel non-steroidal mineralocorticoid receptor antagonist finerenone for the treatment of chronic heart failure: a systematic review and meta-analysis. Med (Baltim). 2018;97:e0254.
Pitt B, Kober L, Ponikowski P, Gheorghiade M, Filippatos G, Krum H, et al. Safety and tolerability of the novel non-steroidal mineralocorticoid receptor antagonist BAY 94-8862 in patients with chronic heart failure and mild or moderate chronic kidney disease: a randomized, double-blind trial. Eur Heart J. 2013;34:2453–63.
Bakris GL, Agarwal R, Chan JC, Cooper ME, Gansevoort RT, Haller H, et al, Mineralocorticoid Receptor Antagonist Tolerability Study–Diabetic Nephropathy (ARTS-DN) Study Group. Effect of finerenone on albuminuria in patients with diabetic nephropathy: a randomized clinical trial. JAMA. 2015;314:884–94.
Katayama S, Yamada D, Nakayama M, Yamada T, Myoishi M, Kato M, ARTS-DN Japan study group. et al. A randomized controlled study of finerenone versus placebo in Japanese patients with type 2 diabetes mellitus and diabetic nephropathy. J Diabetes Complicat. 2017;31:758–65.
Lachaux M, Barrera-Chimal J, Nicol L, Rémy-Jouet I, Renet S, Dumesnil A, et al. Short- and long-term administration of the non-steroidal mineralocorticoid receptor antagonist finerenone opposes metabolic syndrome-related cardio-renal dysfunction. Diabetes Obes Metab. 2018;20:2399–407.
Lattenist L, Lechner SM, Messaoudi S, Le Mercier A, El Moghrabi S, Prince S, et al. Nonsteroidal mineralocorticoid receptor antagonist finerenone protects against acute kidney injury-mediated chronic kidney disease: role of oxidative stress. Hypertension. 2017;69:870–8.
Kolkhof P, Delbeck M, Kretschmer A, Steinke W, Hartmann E, Bärfacker L, et al. Finerenone, a novel selective nonsteroidal mineralocorticoid receptor antagonist protects from rat cardiorenal injury. J Cardiovasc Pharmacol. 2014;64:69–78.
Arai K, Tsuruoka H, Homma T. CS-3150, a novel non-steroidal mineralocorticoid receptor antagonist, prevents hypertension and cardiorenal injury in Dahl salt-sensitive hypertensive rats. Eur J Pharmacol. 2015;769:266–73.
Brosius FC 3rd, Alpers CE, Bottinger EP, Breyer MD, Coffman TM, Gurley SB, Animal Models of Diabetic Complications Consortium et al. Mouse models of diabetic nephropathy. J Am Soc Nephrol. 2009;20:2503–12.
Azushima K, Gurley SB, Coffman TM. Modelling diabetic nephropathy in mice. Nat Rev Nephrol. 2018;14:48–56.
Rafiq K, Sherajee SJ, Hitomi H, Nakano D, Kobori H, Ohmori K, et al. Calcium channel blocker enhances beneficial effects of an angiotensin II AT1 receptor blocker against cerebrovascular-renal injury in type 2 diabetic mice. PLoS One. 2013;8:e82082.
Lei B, Nakano D, Fan YY, Kitada K, Hitomi H, Kobori H, et al. Add-on aliskiren elicits stronger renoprotection than high-dose valsartan in type 2 diabetic KKAy mice that do not respond to low-dose valsartan. J Pharmacol Sci. 2012;119:131–8.
Rafiq K, Noma T, Fujisawa Y, Ishihara Y, Arai Y, Nabi AH, et al. Renal sympathetic denervation suppresses de novo podocyte injury and albuminuria in rats with aortic regurgitation. Circulation. 2012;125:1402–13.
Yamazaki D, Hitomi H, Nishiyama A. Hypertension with diabetes mellitus complications. Hypertens Res. 2018;41:147–56.
Nehme A, Zibara K. Efficiency and specificity of RAAS inhibitors in cardiovascular diseases: how to achieve better end-organ protection? Hypertens Res. 2017;40:903–9.
Dekleva M, Lazic JS, Arandjelovic A, Mazic S. Beneficial and harmful effects of exercise in hypertensive patients: the role of oxidative stress. Hypertens Res. 2017;40:15–20.
Kitada K, Nakano D, Liu Y, Fujisawa Y, Hitomi H, Shibayama Y, et al. Oxidative stress-induced glomerular mineralocorticoid receptor activation limits the benefit of salt reduction in Dahl salt-sensitive rats. PLoS One. 2012;7:e41896.
Nishiyama A, Yao L, Nagai Y, Miyata K, Yoshizumi M, Kagami S, et al. Possible contributions of reactive `oxygen species and mitogen-activated protein kinase to renal injury in aldosterone/salt-induced hypertensive rats. Hypertension. 2004;43:841–8.
Shibata S, Mu S, Kawarazaki H, Muraoka K, Ishizawa K, Yoshida S, et al. Rac1 GTPase in rodent kidneys is essential for salt-sensitive hypertension via a mineralocorticoid receptor-dependent pathway. J Clin Invest. 2011;121:3233–43.
Shibata S, Nagase M, Yoshida S, Kawarazaki W, Kurihara H, Tanaka H, et al. Modification of mineralocorticoid receptor function by Rac1 GTPase: implication in proteinuric kidney disease. Nat Med. 2008;14:1370–6.
Kawarazaki H, Ando K, Shibata S, Muraoka K, Fujita M, Kawarasaki C, et al. Mineralocorticoid receptor–Rac1 activation and oxidative stress play major roles in salt-induced hypertension and kidney injury in prepubertal rats. J Hypertens. 2012;30:1977–85.
Kalluri R, Neilson EG. Epithelial-mesenchymal transition and its implications for fibrosis. J Clin Invest. 2003;112:1776–84.
Huang LL, Nikolic-Paterson DJ, Han Y, Ozols E, Ma FY, Young MJ, et al. Myeloid mineralocorticoid receptor activation contributes to progressive kidney disease. J Am Soc Nephrol. 2014;25:2231–40.
Acknowledgements
We thank Alice Tait, PhD, from Edanz Group (www.edanzediting.com/ac) for editing a draft of this manuscript.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
This was in part a collaborative study with Daiichi-Sankyo Co., Ltd. (to A.N.). The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. This study was also supported in part by the Salt Sciences Foundation (to A.N.).
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Bhuiyan, A.S., Rafiq, K., Kobara, H. et al. Effect of a novel nonsteroidal selective mineralocorticoid receptor antagonist, esaxerenone (CS-3150), on blood pressure and renal injury in high salt-treated type 2 diabetic mice. Hypertens Res 42, 892–902 (2019). https://doi.org/10.1038/s41440-019-0211-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-019-0211-0
Keywords
This article is cited by
-
Exploratory study on the relationship between urinary sodium/potassium ratio, salt intake, and the antihypertensive effect of esaxerenone: the ENaK Study
Hypertension Research (2024)
-
Mineralocorticoid receptor antagonists in diabetic kidney disease — mechanistic and therapeutic effects
Nature Reviews Nephrology (2022)
-
Antihypertensive Effect of Long-Term Monotherapy with Esaxerenone in Patients with Essential Hypertension: Relationship Between Baseline Urinary Sodium Excretion and Its Antihypertensive Effect
Advances in Therapy (2022)
-
Clinical Pharmacokinetics and Pharmacodynamics of Esaxerenone, a Novel Mineralocorticoid Receptor Antagonist: A Review
European Journal of Drug Metabolism and Pharmacokinetics (2022)
-
Antihypertensive effects and safety of esaxerenone in patients with moderate kidney dysfunction
Hypertension Research (2021)