Abstract
The purpose of this study was to identify the effects of various obesity phenotypes and metabolic abnormalities on cardio-cerebrovascular disease. We performed a large-scale, cross-sectional study including 10,089 participants aged ≥18 years in the National High-Technology district of Suzhou, China, from March 2016 to April 2016. Cardio-cerebrovascular disease included stroke and coronary heart disease. The prevalence rates of cardio-cerebrovascular disease among people with normal weight, overweight, and obesity in the unhealthy metabolism subgroup were higher than those among the three BMI groups in the healthy metabolism subgroup. Multivariate logistic regression analyses showed that after adjustment, the odds ratio (OR) of metabolically healthy obesity (MHO) with cardio-cerebrovascular disease was not statistically significant and that metabolically unhealthy obesity (MUO) was statistically associated with cardio-cerebrovascular disease, with an OR of 2.106 (1.294–3.429) in Model 1 and 3.043 (1.510–6.133) in Model 2. This study also found that regardless of whether in Model 1 or Model 2, the number of participants with MHO was much lower than that of those with MUO. Therefore, the obese population usually had metabolic abnormalities. Although MHO was not statistically associated with cardio-cerebrovascular disease, obesity should be controlled along with metabolic abnormalities to reduce the risk of cardio-cerebrovascular disease.
Similar content being viewed by others
Introduction
Obesity is highly related to the incidence of various chronic diseases, such as cardio-cerebrovascular disease and type 2 diabetes mellitus [1,2,3,4,5], which has become a huge public health problem worldwide and caused a considerable burden on global health. Moreover, obesity is usually accompanied by metabolic abnormalities, namely, metabolically unhealthy obesity (MUO). People with MUO are more likely to suffer from diseases such as cardio-cerebrovascular disease than the general population [6]. However, some investigators believe that there is a subset of obesity called metabolically healthy obesity (MHO), which is not accompanied by or is rarely associated with metabolic abnormalities [7, 8].
Whether MHO is associated with cardio-cerebrovascular disease is controversial. Some previous studies have shown that, compared with MUO, the mortality and occurrence of cardiovascular disease in the MHO group was lower [9,10,11,12,13]. A study that included 5314 elderly individuals showed that MHO did not confer a higher cardiovascular disease (CVD) risk [9]. Deng L’s study of 2764 subjects showed that there was no association between the MHO phenotype and the incidence of CVD [11], while some conflicting evidence suggested that MHO had a significant association with heart failure and cardiovascular disease risk [4, 14, 15]. A cohort study of 389,321 individuals in South Korea showed that MHO individuals had an increased risk for atrial fibrillation development [14]. In view of this, it is of great significance to explore the association between MHO and cardio-cerebrovascular disease in large-scale studies. Therefore, this study aimed to identify the effects of various obesity phenotypes and metabolic abnormalities on cardio-cerebrovascular disease.
Methods
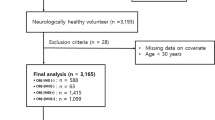
Study population
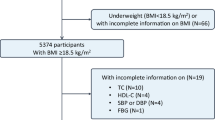
A cross-sectional study was conducted in the National High-Technology district of Suzhou, China, from March 2016 to April 2016. The study adopted a method of random cluster sampling; approximately 1/20 buildings were sampled from 42 communities, and all the residents aged ≥18 years living in the selected buildings were invited to participate in the study. A total of 10,089 participants were investigated; of these, 105 with missing data and 210 with underweight (BMI < 18.5 kg/m2) were excluded, and 9774 with complete data were included in the analysis. Written informed content was obtained from all participants. This study was approved by the Soochow University Ethics Committee and all the performed procedures of the study met ethical requirements.
Data collection and measures
The data were collected by trained staff who conducted face-to-face interviews using a standardized questionnaire that included demographic characteristics, smoking, drinking and physical exercise status, history of disease and medical history. Marital status was divided into married (including married and cohabitation) and single (including unmarried, widowed, divorced, and separated). Education was classified into three categories: illiteracy, primary or middle school, and high school education or above. Cigarette smoking was defined as having at least one cigarette per day for at least six months, and alcohol consumption was defined as any type of alcoholic beverage intake at least one time per week for 12 months or more. Smoking status and drinking status were categorized as current or not current (former or never). Physical exercise was defined as performing more than 30 min of continuous exercise at least three times per week.
All participants underwent a physical examination performed by a qualified doctor, which included measurements of height, weight, waist circumference, and blood pressure. Height and weight were measured with participants wearing light clothing and without shoes, and they were accurate to 0.1 kg and 0.1 cm, respectively, in measurement. Waist circumference was measured at the midpoint of the line between the anterior superior iliac crest and the 12th costal margin and was accurate to 0.1 cm. All participants were asked to stand with their feet ~25–30 cm apart and arms folded across the chest for the measurement of waist circumference, so that body weight would be distributed evenly. Each individual’s blood pressure was measured three times using a mercury sphygmomanometer after a rest period of at least 10 min, and the interval between each measurement was ~2 min. Furthermore, participants could not exercise before blood pressure measurement for at least 30 min. The average of the three measurements was used in the analysis.
Overnight fasting blood samples (at least 8 h) were obtained in the morning and plasma was separated to detect fasting blood glucose (FBG), low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), triglycerides (TG), and total cholesterol (TC). All the biochemical indexes were determined enzymatically on a Hitachi 7020 automatic biochemical analyzer using commercial reagents (KANGXIANG MEDICAL APPLIANCE, Shanghai, P. R. China).
In this study, cardio-cerebrovascular disease included stroke and coronary heart disease (CHD). Stroke was defined as a sudden onset of neurological symptoms lasting 24 h due to hemorrhage or ischemic and positive findings on cranial computed tomography or magnetic resonance imaging. Coronary heart disease was diagnosed based on symptoms, electrocardiographic changes, cardiac enzymes, and autopsy findings, according to the criteria of the World Health Organization MONICA project. Previously diagnosed stroke and CHD were determined on the basis of self-report, and these self-reported cases were verified via hospital records, including admission or outpatient records.
Definitions of MUO and MHO
The body mass index (BMI) was calculated as weight in kilograms divided by the square of height in meters. According to the international criteria for overweight and obesity, BMI was divided into four categories: (1) underweight (BMI < 18.5 kg/m2), (2) normal weight (18.5 kg/m2≤BMI < 25 kg/m2), (3) overweight (25 kg/m2≤BMI < 30 kg/m2), and (4) obesity (BMI > 30 kg/m2). In the analysis, we removed the category of underweight (n = 210), mainly to investigate the association between normal weight, overweight and obesity and cardio-cerebrovascular disease.
We evaluated metabolic status according to the International Diabetes Federation (IDF) definition [16, 17]. In this study, five components were considered to determine an abnormal metabolic status for participants: (1) low HDL level (≤1.04 mmol/L for men or ≤1.29 mmol/L for women), (2) high triglycerides (≥1.7 mmol/L or currently under treatment with lipid-lowering drugs), (3) abnormal blood pressure (SBP ≥130 mmHg or DBP ≥85 mmHg or currently under treatment for hypertension), (4) high fasting blood glucose (≥5.6 mmol/L or currently under treatment for diabetes), and (5) waist circumference > 90 cm for male and > 80 cm for female. The presence of two or more of the five components was determined to be an unhealthy metabolism.
In this study, a healthy metabolism was defined in two different ways: (1) Model 1: participants with one or none of the above five components, (2) Model 2: participants with none of the components (3047 participants with one of five components were excluded, and 7217 participants were included in Model 2). We divided the participants into six phenotypes according to BMI and metabolic status: metabolically healthy normal weight, metabolically healthy overweight, metabolically healthy obesity (MHO), metabolically unhealthy normal weight, metabolically unhealthy overweight, and metabolically unhealthy obesity (MUO).
Statistical analysis
We used mean and standard deviation or median and interquartile range to describe continuous variables, and an analysis of variance or Kruskal–Wallis test to compare the differences across six groups by BMI and metabolic status. For categorical variables, we used frequencies and percentages to describe and Pearson’s chi-square test to compare the differences among six groups by BMI and metabolic status. A logistic regression model was applied to analyze the relationship between cardio-cerebrovascular disease and MUO and MHO before and after adjusting for age, gender, smoking, drinking alcohol, physical exercise, marital status and education, and the odds ratios (ORs) and 95% confidence intervals (CIs) were calculated. All P values were based on two-sided tests and the statistically significant level was 0.05. All statistical analyses were performed using SAS (version 9.4) statistical software.
Results
When we defined healthy metabolism as in Model 1, there were 9774 participants in the study, including 3923 males (40.14%) and 5851 females (59.86%), and the mean age of the subjects was 54.84 ± 16.85 years old. Based on the categories of BMI and metabolic status, 3433 (35.12%) subjects were metabolically healthy normal weight, 952 (9.74%) were metabolically healthy overweight, 70 (0.72%) were MHO, 1957 (20.02%) were metabolically unhealthy normal weight, 2791 (28.56%) were metabolically unhealthy overweight, and 571 (5.84%) were MUO. There were 392 patients with cardio-cerebrovascular disease, comprising 216 patients with isolated coronary heart disease events, 151 patients with isolated stroke events, and 25 patients with coronary heart disease combined with stroke events.
Table 1 shows the baseline characteristics of the participants. According to BMI and metabolic status, we divided the total number of participants into six groups. The differences among the six groups were statistically significant in regard to gender, age, marital status, education, waist circumference, LDL-C, HDL-C, TG, TC, fasting blood glucose, and systolic and diastolic blood pressure. However, there were not statistically significant differences in regard to physical exercise. According to the metabolic status, the participants were divided into two subgroups: a metabolically healthy subgroup and a metabolically unhealthy subgroup. In the metabolically healthy subgroup, obese and overweight participants were more likely to be older, have higher proportions of married and illiterate, have higher levels of waist circumference, BMI, TG, TC, LDL-C, FBG, SBP, and DBP and have lower HDL-C levels than normal weight participants. In the metabolically unhealthy subgroup, the difference in proportion of the prevalence of smoking and drinking alcohol was not statistically significant among the three BMI groups. Compared to normal weight individuals, the obese population was more likely to be younger, have more females and illiterate, have higher levels of waist circumference, BMI, TG, TC, LDL-C, FBG, SBP, and DBP and have lower HDL-C levels. Furthermore, within the BMI category subpopulations, the metabolically unhealthy subgroups had significantly greater waist circumferences and BMI, higher TG, TC, LDL-C, FBG, SBP, and DBP levels and lower plasma levels of HDL-C than the metabolically healthy subgroups. In particular, triglycerides, fasting blood glucose and blood pressure in the MUO group were significantly higher than those in the MHO group.
The prevalence of cardio-cerebrovascular disease among different categories of BMI and metabolic status is presented in Fig. 1. Figure 1a shows the results analyzed according to Model 1; the prevalence rates of cardio-cerebrovascular disease were 1.40%, 1.58%, and 2.86% among normal weight, overweight, and obese participants, respectively, in the healthy metabolism subgroup, and 5.62%, 6.77%, and 4.90%, respectively, in the unhealthy metabolism subgroup. Within the same BMI status, the prevalence of cardio-cerebrovascular disease in the unhealthy metabolism subgroup was significantly higher than in the healthy metabolism subgroup. Figure 1b shows the results analyzed according to Model 2; the prevalence rates of cardio-cerebrovascular disease were 0.74%, 0.00%, and 0.00% among normal weight, overweight, and obese participants, respectively, in the healthy metabolism subgroup, and 5.62%, 6.77%, and 4.90%, respectively, in the unhealthy metabolism subgroup. In the metabolically healthy normal weight subgroup, the prevalence of cardio-cerebrovascular disease among the three BMI groups in Model 2 was lower than those in Model 1.
Prevalence rate of cardio-cerebrovascular disease by BMI and metabolic status categories in two different models. Note Prevalence rate of cardio-cerebrovascular disease by BMI and metabolic status categories in two different ways. Normal weight: 18.5 kg/m2 ≤ BMI < 25 kg/m2, overweight: 25 kg/m2 ≤ BMI < 30 kg/m2, obesity: BMI ≥ 30 kg/m2. a The results analyzed according to Model 1, in which participants had one or none of the five components of an abnormal metabolic status. b The results analyzed according to Model 2, in which participants had none of the components
Table 2 lists the OR values and 95% CIs of cardio-cerebrovascular disease associated with BMI and metabolic status. In Model 1, compared to the metabolically healthy normal weight group, the metabolically healthy overweight and MHO groups were not found to be significantly associated with cardio-cerebrovascular disease after adjusting for age, gender, and other factors associated with cardio-cerebrovascular disease, and the ORs (95% CIs) were 0.928 (0.514–1.677), and 2.062 (0.478–8.896), respectively. However, metabolically unhealthy normal weight, overweight and obese were strongly associated with cardio-cerebrovascular disease, and the ORs (95% CIs) were 2.154 (1.508–3.078), 2.909 (2.090–4.050), and 2.106 (1.294–3.429), respectively. In contrast to Model 1, except for the metabolically healthy overweight and MHO groups, a similar trend was observed between the categories of BMI and metabolic status and cardio-cerebrovascular disease in Model 2: the metabolically unhealthy normal weight, metabolically unhealthy overweight and MUO groups had a greater risk of cardio-cerebrovascular disease than the metabolically healthy normal weight group, with ORs (95% CIs) of 3.143 (1.690–5.843), 4.201 (2.298–7.681), and 3.043 (1.510–6.133), respectively, after adjustment.
Discussion
The purpose of our study was to reveal the relationship between BMI along with metabolic status and cardio-cerebrovascular disease under two different definitions of healthy metabolism. In Model 1, the unhealthy metabolism group had a higher prevalence of cardio-cerebrovascular disease than the healthy metabolism group under the same BMI condition. In Model 2, the difference in the prevalence of cardio-cerebrovascular disease in the unhealthy metabolism group was similar to that of Model 1. Moreover, our study manifested that the prevalence of cardio-cerebrovascular disease in Model 2 was far lower than that in Model 1 in the healthy metabolism group, when healthy metabolism was defined as none of the components of an abnormal metabolic status in Model 2 and one component in Model 1. Furthermore, although the relationship between cardio-cerebrovascular disease and MUO was significant, the risk was not higher than in the metabolically unhealthy normal weight group. This result suggests that the role of obesity was not particularly significant in the development of cardio-cerebrovascular disease. Therefore, we believe that the metabolic abnormalities had a more important influence on cardio-cerebrovascular disease [18,19,20,21]. It was reported that being metabolically unhealthy increased the risk of atrial fibrillation to a greater degree than obesity [14]. However, some studies suggested that obesity was more likely to lead to cardiovascular disease than were metabolic abnormalities [8, 22].
According to our data, we found a point different from previous studies [5, 19, 23,24,25,26]. In Model 1, compared to the metabolically healthy normal weight group, the OR of the MHO group was not statistically significant, although the point estimation was more than 2.0. In Model 2, the prevalence of cardio-cerebrovascular disease was 0.00% in the metabolically healthy overweight and MHO groups; namely, overweight and obesity alone had little impact on cardio-cerebrovascular disease. Our results suggest that in metabolically healthy participants, overweight and obese individuals may not have a higher risk of cardio-cerebrovascular disease than normal weight individuals. A study from European populations showed that metabolically healthy overweight might be related to the occurrence of incident CVD and stroke [19], and a study from South Korea showed that metabolically healthy overweight might also be linked to coronary artery calcium (CAC) [23]. A cohort study of 6453 men suggested that overweight alone had an obvious correlation with subclinical atherosclerosis [24]. A population-based study among Mexican-Americans and non-Hispanic whites, in which MHO was defined as individuals with obesity and no more than one metabolic abnormality, showed that the risk of developing CVD was increased in MHO individuals [25]. In addition, physically inactive MHO participants had a significantly increased risk of CVD compared to metabolically healthy normal weight and physically active MHO participants, and physically active MHO participants might have an increased risk of CVD over that of physically active metabolically healthy normal weight participants [26]. Remarkably, a study reported that not only was the MHO phenotype associated with a significantly higher risk of developing CVD in a Korean population but also that a large number of MHO individuals would develop a metabolically unhealthy phenotype over time during follow-up; namely, MHO is simply a transitional state [5]. However, Thomas et al. from France reported that overweight did not increase the risk of CVD mortality, in the absence of associated metabolic abnormalities such as hypertension, hypercholesterolemia, and diabetes [27], which was consistent with our results.
Under Models 1 and 2, we also found a noteworthy result that the number of participants with MHO was the lowest of all the groups and was far fewer than the number of participants in the MUO group. This finding suggests that obesity by itself is infrequent in the population. In other words, obese populations usually have metabolic abnormalities.
The biggest advantage of our article is that the population with healthy metabolism was defined in two different ways, which is helpful to compare the differences of the effects of BMI and metabolism on cardio-cerebrovascular disease. However, there are still some limitations in our study. First, since this was a cross-sectional study based on communities, the causal link between BMI, metabolism and cardio-cerebrovascular disease needs to be elucidated by a cohort study. Second, in recent years, some researchers have considered insulin resistance as a component of metabolic disorders [28, 29], but our study did not take this into account. Third, as in most epidemiological studies, residual confounding is of concern. Although our analysis controlled for some factors of CVD, some effects of unmeasured confounders, such as family economic status and medication for CVD, may exist.
Conclusion
Our study shows that metabolic abnormalities are a more important risk factor than obesity for cardio-cerebrovascular disease. In the absence of metabolic abnormalities, obesity alone may not increase the incidence of cardio-cerebrovascular disease. However, the number of people with obesity alone is very few in the population, as obese populations usually have metabolic abnormalities. Therefore, metabolic abnormalities and obesity should be controlled simultaneously to reduce the risk of cardio-cerebrovascular disease.
References
Appleton SL, Seaborn CJ, Visvanathan R, Hill CL, Gill TK, Taylor AW. et al. Diabetes and cardiovascular disease outcomes in the metabolically healthy obese phenotype: a cohort study. Diabetes Care. 2013;36:2388–94.
Sung KC, Ryu S, Cheong ES, Kim BS, Kim YB, Chung PW. et al. All-cause and cardiovascular mortality among Koreans: effects of obesity and metabolic health. Am J Prev Med. 2015;49:62
Boateng D, Agyemang C, Beune E, Meeks K, Smeeth L, Schulze M, et al. Migration and cardiovascular disease risk among Ghanaian populations in Europe: the RODAM study (research on obesity and diabetes among African migrants). Circ Cardiovasc Qual Outcomes. 2017;10:e004013.
Hinnouho GM, Czernichow S, Dugravot A, Nabi H, Brunner EJ, Kivimaki M, et al. Metabolically healthy obesity and the risk of cardiovascular disease and type 2 diabetes: the Whitehall II cohort study. Eur Heart J. 2015;36:551–9.
Kim NH, Seo JA, Cho H, Seo JH, Yu JH, Yoo HJ, et al. Risk of the development of diabetes and cardiovascular disease in metabolically healthy obese people: the Korean Genome and epidemiology study. Medicine. 2016;95:e3384.
Grundy SM. Obesity, metabolic syndrome, and cardiovascular disease. J Clin Endocrinol Metab. 2004;89:2595–2600.
Ri BA, Seungwon K, Wha LS, Won SK, Soo LH. Metabolic health is more closely associated with prevalence of cardiovascular diseases or stroke than obesity: a cross-sectional study in Korean populations. Medicine. 2016;95:e3902.
Roberson LL, Aneni EC, Maziak W, Agatston A, Feldman T, Rouseff M, et al. Beyond BMI: the “Metabolically healthy obese” phenotype & its association with clinical/subclinical cardiovascular disease and all-cause mortality—a systematic review. BMC Public Health. 2014;14:14.
Dhana K, Koolhaas CM, EFCV Rossum, Ikram MA, Hofman A, Kavousi M, et al. Metabolically healthy obesity and the risk of cardiovascular disease in the elderly population. PLoS ONE 2016;11:e0154273.
Hamer M, Stamatakis E. Metabolically healthy obesity and risk of all-cause and cardiovascular disease mortality. J Clin Endocrinol & Metab. 2012;97:2482.
Deng L, Fang L, Li X, Yin D, Lin Z, Hui L, et al. Comparison of the effect of ‘metabolically healthy but obese’ and ‘metabolically abnormal but not obese’ phenotypes on development of diabetes and cardiovascular disease in Chinese. Endocrine. 2015;49:130–8.
Guo F, Garvey WT. Cardiometabolic disease risk in metabolically healthy and unhealthy obesity: stability of metabolic health status in adults. Obesity. 2015;24:516–25.
De LA, Glerian L, Amaral AC, Reis TB, Lima RS. “Metabolically healthy” obesity: prevalence, clinical features and association with myocardial ischaemia. Obes Res Clin. 2017;11:315–23.
Lee H, Choi EK, Lee SH, Han KD, Rhee TM, Park CS, et al. Atrial fibrillation risk in metabolically healthy obesity: A nationwide population-based study. Int J Cardiol. 2017;240:221–7.
Fan J, Song Y, Chen Y, Hui R, Zhang W. Combined effect of obesity and cardio-metabolic abnormality on the risk of cardiovascular disease: a meta-analysis of prospective cohort studies. Int J Cardiol. 2013;168:4761–8.
Saklayen MG. The global epidemic of the metabolic syndrome. Curr Hypertens Rep. 2018;20:12.
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International A. Circulation. 2009;120:1640–5.
Zhao L, Guo X, Liu Y, Zhang N, Ye C, Chen Y, et al. Metabolism rather than obesity is associated with ischemic stroke: a cross-sectional study in rural Northeastern China. +. 2016;5:1419.
Lassale C, Tzoulaki I, Moons K, Sweeting M, Boer J, Johnson L, et al. Separate and combined associations of obesity and metabolic health with coronary heart disease: a pan-European case-cohort analysis. Eur Heart J. 2018;39:397–406.
Ju SY, Lee JY, Kim DH. Association of metabolic syndrome and its components with all-cause and cardiovascular mortality in the elderly: a meta-analysis of prospective cohort studies. Medicine. 2017;96:e8491.
Zhang N, Chen Y, Guo X, Sun G, Dai D, Sun Y. Metabolic abnormalities, but not metabolically healthy obesity, are associated with left ventricular hypertrophy. Heart Lung Circ. 2016;26:251–7.
Kramer CK, Zinman B, Retnakaran R. Are metabolically healthy overweight and obesity benign conditions?: A systematic review and meta-analysis. Ann Intern Med. 2013;159:758–69.
Chang Y, Kim BK, Yun KE, Cho J, Zhang Y, Rampal S, et al. Metabolically-healthy obesity and coronary artery calcification. J Am Coll Cardiol. 2014;63:2679–86.
Kim TJ, Shin HY, Chang Y, Kang M, Jee J, Choi YH, et al. Metabolically healthy obesity and the risk for subclinical atherosclerosis. Atherosclerosis. 2017;262:191–7.
Aung K, Lorenzo C, Hinojosa MA, Haffner SM. Risk of developing diabetes and cardiovascular disease in metabolically unhealthy normal-weight and metabolically healthy obese individuals. J Clin Endocrinol Metab. 2014;99:462–8.
Moon S, Oh CM, Choi MK, Park YK, Chun S, Choi M, et al. The influence of physical activity on risk of cardiovascular disease in people who are obese but metabolically healthy. PLoS ONE 2017;12:e0185127.
Thomas F, Bean K, Pannier B, Oppert JM, Guize L, Benetos A. Cardiovascular mortality in overweight subjects. Hypertension. 2005;46:654–9.
Calori G, Lattuada G, Piemonti L, Garancini MP, Ragogna F, Villa M, et al. Prevalence, metabolic features, and prognosis of metabolically healthy obese Italian individuals: the Cremona Study. Diabetes Care. 2011;34:210.
Ferrannini E, Natali A, Bell P, Cavalloperin P, Lalic N, Mingrone G. Insulin resistance and hypersecretion in obesity. European Group for the Study of Insulin Resistance (EGIR). J Clin Investig. 1997;100:1166–73.
Acknowledgements
We are deeply appreciative of the participants and community doctors involved in the study and thank the Suzhou National High-Technology District Center for Disease Prevention and Control for their support and assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Chen, X., Gui, G., Ji, W. et al. The relationship between obesity subtypes based on BMI and cardio-cerebrovascular disease. Hypertens Res 42, 912–919 (2019). https://doi.org/10.1038/s41440-018-0184-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-018-0184-4
Keywords
This article is cited by
-
Association between CCN1 gene polymorphism and acute coronary syndrome in Chinese Han and Uygur populations
Hereditas (2021)
-
Analysis of lifetime death probability for major causes of death among residents in China
BMC Public Health (2020)
-
Improving obesity and blood pressure
Hypertension Research (2020)