Abstract
Autosomal dominant polycystic kidney disease (ADPKD) is commonly caused by PKD1, and mosaic PKD1 variants result in milder phenotypes. We present the case of a 32 year-old male with chronic active Epstein–Barr virus who underwent bone marrow transplantation with chemoradiotherapy at age 9. Despite a low-frequency mosaic splicing PKD1 variant, he developed severe renal cysts and end-stage renal disease in his 30 s. This case highlights how environmental factors may contribute to the genetic predisposition to ADPKD.
Similar content being viewed by others
Cystic kidneys frequently lead to end-stage renal disease (ESRD). Autosomal dominant polycystic kidney disease (ADPKD) is the most common form of PKD1. Genetic variants of PKD1 or PKD2, which encode polycystins (PCs) 1 and 2, respectively, are the most common variants associated with ADPKD1. Mosaic variants of PKD1 are also involved in cases of PKD, and these patients reportedly exhibit milder phenotypes2.
Chronic active Epstein–Barr virus (EBV) disease (CAEBV) is a lethal syndrome caused by persistent EBV infection. Current treatments for CAEBV include chemoradiotherapy (CRT) and hematopoietic stem cell transplantation3. CRT during childhood can cause various future complications, such as secondary cancers, especially in tissues with slow turnover, such as the brain and kidneys4.
Herein, we report the case of a 32 year-old male who was referred to our department for genetic testing. The patient was born to nonconsanguineous parents via vaginal delivery without complications at 39 weeks of gestation. The patient had no significant family history. The patient was healthy until he was diagnosed with CAEBV at 5 years of age. The patient was treated with interferon, interleukin, and high-dose steroid therapy for 2 years. When the patient was 9 years old, he underwent total body radiation (12 Gy), high-dose chemotherapy/myeloablative conditioning and bone marrow transplantation (BMT) with his father as a donor. Clusters of clonic seizures occurred 25 days after BMT, and the patient was diagnosed with epilepsy. Subsequently, he developed refractory epilepsy and was prescribed multiple antiseizure medications, and a vagus nerve stimulator was implanted. He also had significant medical problems, such as chronic kidney disease (blood test results revealed a blood urea nitrogen level of 36.6 mg/dL, creatinine level of 2.66 mg/dL, and estimated glomerular filtration rate of 26.3%), high blood pressure, hypothyroidism, retinochoroidal atrophy, bilateral cataracts, and parkinsonism. Recent brain magnetic resonance imaging (MRI) analysis revealed hyperintensity in both basal ganglia on T1-weighted imaging (T1WI) (Fig. 1a). Additionally, a ring-shaped angioma with hyperintensity on T1WI (Fig. 1b) and hypointensity on T2WI was observed in the left frontal lobe (Fig. 1c). Computed tomography (CT) of the head revealed calcifications in the bilateral basal ganglia and cerebral lesions (Fig. 1d). Abdominal CT revealed severe bilateral PKD (Fig. 1e). The patient is now waiting for a kidney transplant while undergoing peritoneal dialysis.
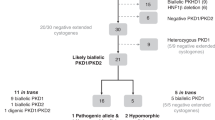
The patient and his parents requested genetic testing and provided informed consent. A gene panel test and whole-exome sequencing (WES) were performed. Customized panel analysis revealed a novel mosaic splice site variant of PKD1 [NC_000016.10 (NM_001009944.3):c.3295+2 T > A] in genomic DNA derived from both hair and urine samples. Detailed information about the analysis and pathological evaluation of each variant is described in the Supplementary Methods. The identified variant is not registered in population databases, such as gnomAD and jMorp, and was evaluated as likely pathogenic (PVS1 + PM2) according to the ACMG–AMP guidelines. The variant allele frequencies in genomic DNA derived from hair and urine samples were 16.5% (17/107) and 10.6% (11/104), respectively (Fig. 2a). Customized panel analysis of genomic DNA from urine-derived cells did not reveal other pathogenic or likely pathogenic variants with allele frequencies >10%, indicating that no second hit of the other PKD1 allele occurred. Direct sequencing analysis revealed the same variants that were detected using next-generation sequencing of genomic DNA from hair- and urine-derived cell samples, and the peaks of the variants were lower than those of the wild-type alleles (Fig. 2b). WES analysis revealed no pathogenic germline variants in other genes.
a The allele frequency of the variant [NC_000016.10(NM_001009944.3):c.3295+2 T > A] was 16.5% (17/107) for genomic DNA from hair samples and 10.6% (11/104) for genomic DNA from urine samples. b The variant [NC_000016.10(NM_001009944.3):c.3295+2 T > A] was identified in genomic DNA from hair and urine samples. The peaks of the variant are low, suggesting somatic mosaicism.
Despite a low variant allele frequency of 10.6% in urine-derived cells, the patient developed severe bilateral PKD in his early 30 s and needed dialysis and renal transplantation. Hopp et al. noted that patients with PKD1 mosaic variants exhibited milder symptoms2. In this patient, the variant allele frequency was low (~10%); however, the renal symptoms were severe at 33 years of age. The reported median renal survival of individuals with end-stage kidney disease carrying PKD1 truncating variants was 55.6 years of age5.
The loss of function of the receptor/channel complex formed by the proteins encoded by PKD genes below an undetermined threshold triggers cyst development, which leads to the dysregulation of multiple metabolic processes and cyst growth6. Disease severity is determined by the effect of the primary variant on the activity of PC1 and PC2, in addition to the presence of other variants and environmental factors such as renal injury7. In the present case, the allele frequency of the PKD1 variant was ~10%; therefore, it did not strongly decrease PC1 activity, and no other variants in inherited renal disease genes, including PKD1, were found in urine-derived genomic DNA.
Our case suggests that, even in a patient with PKD1 with a very low-frequency mosaic variant, CRT may exacerbate PKD. Radiotherapy causes DNA breaks and subsequent cell death, and an increasing number of patients who undergo chemotherapy experience side effects4. Chemotherapy also increases the risk of late effects8.
CRT for CAEBV is potentially associated with late adverse effects. In the present case, the patient developed several symptoms in addition to severe PKD and ESRD. He presented with a cavernous hemangioma and calcifications in the brain and developed epilepsy and parkinsonism in his early 30 s. Although co-occurrence of cerebral cavernous malformations and ADPKD is often observed, cerebral cavernous malformations can also occur after cerebral radiation9. Refractory epilepsy has also been reported as a late effect of chemoradiation10. There are also reports of intracranial calcification in the basal ganglia and parkinsonism caused by radiation therapy11. Furthermore, hypothyroidism and retinochoroidal atrophy have been reported as late adverse effects of CRT12.
This case emphasizes the potential influence of environmental factors on genetic predisposition in ADPKD patients. Furthermore, it highlights that late adverse effects of childhood CRT are a serious clinical concern, particularly in patients with a genetic predisposition for PKD, which necessitates long-term follow-up in these patients.
HGV Database
The relevant data from this Data Report are hosted at the Human Genome Variation Database at https://doi.org/10.6084/m9.figshare.hgv.3397.
References
Bergmann, C. et al. Polycystic kidney disease. Nat. Rev. Dis. Prim. 4, 50 (2018).
Hopp, K. et al. Detection and characterization of mosaicism in autosomal dominant polycystic kidney disease. Kidney Int. 97, 370–382 (2020).
Lv, K. et al. Treatment advances in EBV related lymphoproliferative diseases. Front. Oncol. 12, 838817 (2022).
Majeed, H. & Gupta, V. Adverse Effects of Radiation Therapy (StatPearls Publishing: Treasure Island (FL), 2023).
Koptides, M. & Deltas, C. C. Autosomal dominant polycystic kidney disease: molecular genetics and molecular pathogenesis. Hum. Genet 107, 115–126 (2000).
Qiu, J., Germino, G. G. & Menezes, L. F. Mechanisms of cyst development in polycystic kidney disease. Adv. Kidney Dis. Health 30, 209–219 (2023).
Ong, A. C. & Harris, P. C. A polycystin-centric view of cyst formation and disease: the polycystins revisited. Kidney Int. 88, 699–710 (2015).
Ishida, Y. et al. Secondary cancer after a childhood cancer diagnosis: viewpoints considering primary cancer. Int. J. Clin. Oncol. 23, 1178–1188 (2018).
Kim, M. S., Kim, S. H., Chang, J. H., Park, M. & Cha, Y. J. Clinicopathological differences in radiation-induced organizing hematomas of the brain based on type of radiation treatment and primary lesions. J. Pathol. Transl. Med. 56, 16–21 (2022).
Wong, J. N., Lenzen, A. C., Stockman, J. & Garcia Sosa, R. M. Refractory epilepsy as a late effect of chemoradiation in childhood cancer: a case series. Pediatr. Neurol. 127, 56–59 (2022).
Shimada, T. et al. Radiation-induced brain calcification leads to L-dopa-resistant parkinsonism and cerebellar ataxia. Intern. Med. 61, 3723–3727 (2022).
Ghezzaz, A., Idlefqih, W., Chahed, S. & Mahdjoubi, A. Choroidal neovascularization in torpedo maculopathy treated by aflibercept: long-term follow-up using optical coherence tomography and optical coherence tomography angiography. Retin Cases Brief. Rep. 17, 433–437 (2023).
Acknowledgements
The authors are grateful to the patient and his parents for participating in this study and to the doctors of the Department of Pediatrics at Kobe University for their advice on this report.
Author information
Authors and Affiliations
Contributions
H.H. and H.Y. designed and conceptualized the study, analyzed the data, and drafted the manuscript for intellectual content. N.M. and M.J.Y. acquired, analyzed, and interpreted the data and revised the manuscript for intellectual content. R.M. and H.N. analyzed and interpreted the data and revised the manuscript for intellectual content. K.N. designed and conceptualized the study, analyzed and interpreted the data, and revised the manuscript for intellectual content.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study was approved by the Ethics Committee of Kobe University (2022-86). All experiments were performed in accordance with the relevant guidelines and regulations of the institutions and the Code of Ethics of the World Medical Association (Declaration of Helsinki [2013]). Informed consent was obtained from the patient and his parents.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hanafusa, H., Yamaguchi, H., Morisada, N. et al. End-stage ADPKD with a low-frequency PKD1 mosaic variant accelerated by chemoradiotherapy. Hum Genome Var 11, 17 (2024). https://doi.org/10.1038/s41439-024-00273-0
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41439-024-00273-0