Abstract
Purpose
The LZTR1 gene has been associated with schwannomatosis tumor predisposition and is located in a region that is deleted in the great majority (89%) of patients with 22q11.2 deletion syndrome (22q11.2DS). Since it is known that approximately 1 in 500 people in the general population will develop a sporadic schwannoma and there are no reports of the occurrence of schwannoma in 22q11.2DS, we investigated whether whole-gene deletion of LZTR1 occurs in schwannomatosis and assessed the risk of schwannoma in 22q11.2DS.
Methods
We assessed the genetic testing results for LZTR1-associated schwannomatosis and the clinical phenotypes of patients with 22q11.2DS.
Results
There were no reports of schwannoma in over 1,500 patients with 22q11.2DS. In addition, no patients meeting clinical diagnostic criteria for schwannomatosis had a whole-gene deletion in LZTR1. Only 1 patient in 110 with an apparently sporadic vestibular schwannoma had a constitutional whole-gene deletion of LZTR1.
Conclusion
People with a large 22q11.2 deletion may have a reduced risk of developing a schwannoma compared to the general population.
Similar content being viewed by others
INTRODUCTION
Heterozygous loss-of-function pathogenic variants in LZTR1 are a known cause of schwannoma predisposition1 and account for around 30% of both inherited and sporadic cases of schwannomatosis.2 The mechanism of schwannoma formation resulting from a germline pathogenic variant in LZTR1 on chromosome 22 is more complex than the traditional two-hit hypothesis3 and is thought to require biallelic loss of NF2 as well as LZTR1.4,5 Following the predisposing germline event (hit 1), a subsequent, acquired loss of the unaffected copy of 22q deletes the remaining copy of LZTR1 and also one copy of NF2 (a second event including two genetic hits). The final (third) event is the additional acquisition of a loss-of-function variant (usually of a single nucleotide) in NF2.5 This three-event, four-hit mechanism is now well established as the cause of schwannomas both through the SMARCB1 and LZTR1 pathways. Whole-gene deletion and other copy-number variants in SMARCB1 are typically linked to rhabdoid tumor predisposition syndrome (RTPS) and have not been reported to cause schwannomas.6 Typically, schwannomatosis-associated SMARCB1 variants that cause around 40% of hereditary and 10% of sporadic schwannomatosis are “hypomorphic” with some presumed preserved function of the affected allele.6 This preserved function appears to be sufficient to prevent development of rhabdoid tumors in the critical first few years of life. Typical LZTR1 variants that cause schwannomatosis are more likely to be truncating variants, such as frameshift deletions and nonsense variants that are predicted to lead to complete loss of protein, while nontruncating variants are less common.2 However, whole-gene deletions have not been reported in schwannomatosis.
The LZTR1 gene is located within chromosome 22q11.2. This region is known to be deleted in the majority of people with 22q11.2 deletion syndrome (22q11.2DS), which occurs in approximately 1 in 3–6,000 live births.7 The 22q11.2 deletions occur between four low copy repeat regions, LCR22A, LCR22B, LCR22C, and LCR22D, varying in size from approximately 700 kilobases to three megabases. The LZTR1 gene is located within the LCR22C–LCR22D region. The most common deletion is three megabases, caused by nonallelic homologous recombination (NAHR) between LCR22A and LCR22D. The major features of 22q11.2DS are immunodeficiency, palatal anomalies, hypoparathyroidism, and congenital heart disease (CHD). There are many other possible associated features of this condition, such as skeletal, renal, and gastrointestinal differences, autoimmune disease, cognitive deficits, behavioral differences, and psychiatric illness. However, schwannomas have not been reported in people with this deletion and whole-gene deletions have not been reported in LZTR1-associated schwannomatosis. We sought to investigate the risk of schwannomas in 22q11.2 deletion syndrome and the association with whole-gene deletion in LZTR1-associated schwannomatosis.
MATERIALS AND METHODS
Two large genetic testing databases were interrogated to identify LZTR1 variants in individuals who presented with schwannomas. A total of 247 individuals were identified with an LZTR1 variant. Of these, 124 were identified through the Manchester Centre for Genomic Medicine and 123 were identified through the genetic testing service at Birmingham, Alabama. This excluded class 3 variants with low likelihood of reclassification to likely pathogenic. These samples were analyzed using a combination of Sanger sequencing, and in-house next-generation panel sequencing (including the NF2, SMARCB1, and LZTR1 genes). Copy number was assessed by multiple ligation-dependent probe amplification (MLPA), using probe sets P043-NF2, P258-B1, and P455 LZTR1, respectively (MRC-Holland, Amsterdam, the Netherlands), or by microarray analysis using the OGT CytoSure Constitutional v3 8x60k array or Illumina Infinium CytoSNP-850K array.
To determine the number of schwannomas found in people with 22q11.2 deletion syndrome, 1,556 patients with known 22q11.2 deletion syndrome were identified through the 22q and You Center at the Children’s Hospital of Philadelphia. Loss of 22q11.2 was assessed in the majority by microarray analysis and hospital records were assessed for associated conditions. Of these patients, 322 were assessed by clinical brain magnetic resonance image (MRI) due to a history of seizures/abnormal neurologic exam and another 94 were assessed by brain MRI as part of a research study. In addition, 94 were assessed by spine MRI due to a suspicion of a tethered cord. Furthermore, a survey of the UK database of 22q11.2DS self-reported cases was conducted through social media and by email through the Max Appeal charity.
RESULTS
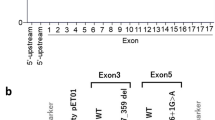
We reviewed the genetic testing results for schwannoma predisposition in over 1,000 cases from unrelated families in two large genomic testing laboratories. In a total of 247 identified LZTR1 variants, there were no single or multiple exon deletions, and no whole-gene deletions, identified in patients fulfilling schwannomatosis criteria. A denominator for schwannomatosis was not known in Birmingham, Alabama. However, 116/425 (27.3%) of those meeting schwannomatosis criteria in Manchester (100/400 unrelated families [25%]) had a variant in LZTR1 (excluding class 3 variants of uncertain significance). A further 8 individuals with an isolated schwannoma in Manchester had an LZTR1 variant. This included 4/110 patients who presented with sporadic vestibular schwannoma who were screened for LZTR1 variants. In this group, one of the four LZTR1 pathogenic variant positive cases had a germline whole-gene deletion. Microarray analysis indicated that the deletion extended to 942 kilobases, between LCR22B-D domains (Fig. 1). The patient, who was in her early 20s, had no features of 22q11.2DS. She had not had her tumor removed, so further investigation of the mechanism of schwannoma formation was not possible (it is normal procedure to watch and wait and rescan a small vestibular schwannoma as they may not need surgery or other treatment for many years).
Solid gray bars indicate (a) the common 3-mb deletion region seen in 22q11.2DS (upper bar), (b) the deleted region in the LZTR1-associated vestibular schwannoma patient with a whole-gene deletion (middle bar), and (c) the approximate breakpoints in tumors from two unrelated LZTR1-associated schwannomatosis patients (lower bar).
Age of onset of first schwannoma was available on 122 patients (range 3–78) and confirmed a median of 38 years (mean = 39.6) with 24 aged <29 years.
We next assessed the known incidence of schwannoma in 22q11.2 deletion syndrome. It is known that the typical three megabase deletion that accounts for 85% of cases includes complete deletion of LZTR1.8 Yet no single case of schwannoma appears in 3,054 reports of Di George syndrome on PubMed (searches using the terms: Di George syndrome AND “schwannoma” and 22q11.2 deletion syndrome AND “schwannoma” were carried out at https://pubmed.ncbi.nlm.nih.gov/?term=Di+George+syndrome+&sort=date, 22 September 2020), nor in 3,031 reports of 22q11.2 deletion syndrome. We also assessed known incidence in over 1,556 patients with known 22q11.2 deletion syndrome evaluated in the 22q and You Center at the Children’s Hospital of Philadelphia. Of those with microarray analysis, 1,046/1,151 (89%) patients had a deletion involving LZTR1 (Table 1). A further 405 individuals had only fluorescence in situ hybridization (FISH) analysis. No cases of schwannoma have been observed in this cohort, despite over 51% of these patients being adults. In addition, a total of 418 of these patients were assessed by brain MRI and 94 were assessed by spine MRI and no schwannomas were detected.
A survey of 1,695 UK self-reported individuals with 22q11.2DS and their families through the family support organization, Max Appeal, did not identify any cases of schwannoma or nerve sheath tumor, although several likely schwannomas were identified in siblings and parents without known 22q11.2DS.
We also assessed the rate of probable LZTR1 loss-of-function variants in gnomAD data (https://gnomad.broadinstitute.org/transcript/ENST00000215739?dataset=gnomad_r2_1; 20 January 2021). There were 465 from a mean of 112,096 individuals (~1 in 241) with a nonsense, frameshift, or canonical splice region variant (excluding low confidence calls). This means that if the effect of a whole-gene deletion were the same as a loss-of-function point variant, then, due to the 1 in 3–6,000 frequency of 22q11.2DS, we should expect to find one 22q11.2 deletion for every 12 to 25 LZTR1-associated schwannomatosis diagnoses. Therefore, in our cohort of 247 LZTR1-associated schwannomatosis patients, we should have found a minimum of ten 22q11.2 deletions, but none were found.
DISCUSSION
In the general population, 1 in 500 people will develop a sporadic schwannoma (1 in 1,000 will develop a vestibular schwannoma and 1 in 1,000 will develop a nonvestibular schwannoma).9 While the majority of heritable predisposition to schwannomas is known to be associated with NF2 germline variants, a proportion of these have also been associated with LZTR1 variants.1,2 In our review of 1,556 people with proven 22q11.2DS (89% with LZTR1 deletion) none had a schwannoma. This finding was confirmed by brain MRI in 418 people, and by spine MRI in 94 people, in this group. Assuming a similar proportion in the self-reported unconfirmed UK based survey of 22q11.2DS, a further 1,508 are likely also to have had an LZTR1 deletion. This would mean that close to 3,000 people with LZTR1-deleted 22q11.2DS were included in our analysis. Although many of these patients are still young, a large number would have been expected to have developed schwannomas if the risks were similar to typical LZTR1 loss-of-function variants, since the median age at onset in people with a pathogenic LZTR1 variant is 38 years in our cohort and 20% developed symptomatic tumors below the age of 29 (~85% of the 22q11.2DS cohort is below this age). It would also be reasonable to expect to have seen at least one by chance, i.e., population risk. However, life expectancy is reduced in 22q11.2DS and the presence of acute and life-threatening complications (such as CHD, hypoparathyroidism, psychosis, cervical spine anomaly) limits our current assessment.
The absence of reported schwannoma in the literature and in two large series of patients with 22q11.2DS suggests that the typical large deletion at 22q11.2, including LZTR1, is not a risk factor for schwannoma. While whole-gene deletions and single and multiple exon deletions occur as a relatively frequent pathogenic variant type in tumor predisposition syndromes, whole-gene deletions are not normally associated with loss of heterozygosity (LOH) as the second loss-of-function event for that gene.10 This does not negate the potential for biallelic loss of function; however, the second hit is nearly always a single-nucleotide pathogenic variant in the wild type allele. In the case of LZTR1, a single-nucleotide pathogenic variant as a second hit would not lead to loss of NF2 on the same allele and would almost certainly not advance schwannoma formation. Alu repeats in the deleted region lead to limited mechanisms of loss by recombination on that allele, leaving only the option of biallelic NF2 single-nucleotide pathogenic variants, which occur as the cause in <30% of sporadic vestibular schwannomas with both hits identified.11 It is possible that this could have occurred in the single case we observed with a large 22q11.2 deletion and a schwannoma, or the tumor could have occurred as a chance association through biallelic single-nucleotide pathogenic variants within the NF2 gene.
Assuming that somatic loss of the normal copy of 22q is mechanistically still possible in patients with 22q11.2DS, it is indeed possible that homozygous deletion of such a large region, involving multiple genes, might be cell lethal, thus preventing tumor development. Some support for this theory comes from analysis of copy-number alterations found in cancer cell lines, e.g., using the copy-number analysis (CONAN) database (http://www.sanger.ac.uk/cgi-bin/genetics/CGP/conan/search.cgi) available through the Wellcome Trust Sanger Institute Cancer Genome Project (accessed 11 June 2020).11 It also remains possible that a complete absence of LZTR1 protein due to deletion does not provide the same pathogenic effect as a partially functional protein.12 In addition, the normal mechanism of sporadic schwannoma formation with a point variant and LOH of NF2 would only be possible if the single-nucleotide pathogenic variant occurred in trans with the 22q11.2 deletion, further reducing the chances of even a sporadic schwannoma. It is therefore possible that if loss of both copies of the whole wild type 22q11.2 allele is cell lethal, then 22q11.2 deletion syndrome patients may have a reduced risk of schwannoma as well as other 22q mediated tumors such as meningioma. However, only further follow up of an even larger series of patients with a proven chromosome 22q11.2 deletion inclusive of LZTR1 into older age will assess the validity of this possibility.
Data availability
Anonymized research data are available upon request.
References
Piotrowski, A. et al. Germline loss-of-function mutations in LZTR1 predispose to an inherited disorder of multiple schwannomas. Nat. Genet. 46, 182–187 (2014).
Smith, M. J. et al. Mutations in LZTR1 add to the complex heterogeneity of schwannomatosis. Neurology. 84, 141–147 (2015).
Knudson, A. G. Jr. Mutation and cancer: statistical study of retinoblastoma. Proc. Natl. Acad. Sci. U. S. A. 68, 820–823 (1971).
Sestini, R., Bacci, C., Provenzano, A., Genuardi, M. & Papi, L. Evidence of a four-hit mechanism involving SMARCB1 and NF2 in schwannomatosis-associated schwannomas. Hum. Mutat. 29, 227–231 (2008).
Kehrer-Sawatzki, H., Farschtschi, S., Mautner, V. F. & Cooper, D. N. The molecular pathogenesis of schwannomatosis, a paradigm for the co-involvement of multiple tumour suppressor genes in tumorigenesis. Hum. Genet. 136, 129–148 (2017).
Smith, M. J., Wallace, A. J., Bowers, N. L., Eaton, H. & Evans, D. G. SMARCB1 mutations in schwannomatosis and genotype correlations with rhabdoid tumors. Cancer Genet. 207, 373–378 (2014).
McDonald-McGinn, D. M. et al. 22q11.2 deletion syndrome. Nat. Rev. Dis. Primers 1, 15071 (2015).
Campbell, I. M. et al. What is new with 22q? An update from the 22q and You Center at the Children’s Hospital of Philadelphia. Am. J. Med. Genet. 176, 2058–2069 (2018).
Evans, D. G. et al. Incidence of vestibular schwannoma and neurofibromatosis 2 in the North West of England over a 10-year period: higher incidence than previously thought. Otol. Neurotol. 26, 93–97 (2005).
Smith, M. J. et al. The contribution of whole-gene deletions and large rearrangements to the mutation spectrum in inherited tumor predisposing syndromes. Hum. Mutat. 37, 250–256 (2016).
Tate, J. G. et al. COSMIC: the Catalogue Of Somatic Mutations In Cancer. Nucleic Acids Res. 47, D941–D947 (2019).
Frattini, V. et al. The integrated landscape of driver genomic alterations in glioblastoma. Nat. Genet. 45, 1141–1149 (2013).
Acknowledgements
D.G.E. and M.J.S. are supported by the all Manchester NIHR Biomedical Research Centre (IS-BRC-1215-20007). This work was also supported by a USAMRAA CDMRP Neurofibromatosis Research Program, Investigator-Initiated Research Award (W81XWH1910334) to M.J.S. We thank Julie Wootton and Max Appeal for surveying their membership.
Author information
Authors and Affiliations
Contributions
Conceptualization: D.G.E., W.D.F. Data curation: D.G.E., L.M.M., D.M.M.-M., J.W. Formal analysis: D.G.E., M.J.S., C.P.-B. Resources: D.G.E., L.M.M., W.D.F., R.E.A.I., A.J.M., D.A.S., B.R. Writing original draft: D.G.E., M.J.S. Reviewing and editing the manuscript: All authors.
Corresponding author
Ethics declarations
Competing interests
D.G.E. has received travel grants from AstraZeneca. The other authors declare no competing interests.
Ethics declaration
Research elements of the analysis were carried out under ethics approval (reference 10/H1008/74) obtained from the North West 7–Greater Manchester Central Research Ethics Committee. Patient data from large clinical databases was anonymized for this study. Written consent was received for the use of patient information from the individual with a whole LZTR1 gene deletion detailed in the manuscript.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Evans, D.G., Messiaen, L.M., Foulkes, W.D. et al. Typical 22q11.2 deletion syndrome appears to confer a reduced risk of schwannoma. Genet Med 23, 1779–1782 (2021). https://doi.org/10.1038/s41436-021-01175-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41436-021-01175-0
This article is cited by
-
DGCR8 and the six hit, three-step model of schwannomatosis
Acta Neuropathologica (2022)