Abstract
Objectives
To estimate global and regional trends from 2000 to 2020 of the number of persons visually impaired by glaucoma and their proportion of the total number of vision-impaired individuals.
Methods
A systematic review and meta-analysis of published population studies and grey literature from 2000 to 2020 was carried out to estimate global and regional trends in number of people with vision loss due to glaucoma. Moderate or severe vision loss (MSVI) was defined as visual acuity of 6/60 or better but <6/18 (moderate) and visual acuity of 3/60 or better but <6/60 (severe vision loss). Blindness was defined as presenting visual acuity <3/60.
Results
Globally, in 2020, 3.61 million people were blind and nearly 4.14 million were visually impaired by glaucoma. Glaucoma accounted for 8.39% (95% uncertainty intervals [UIs]: 6.54, 10.29) of all blindness and 1.41% (95% UI: 1.10, 1.75) of all MSVI. Regionally, the highest proportion of blindness relating to glaucoma was found in high-income countries (26.12% [95% UI: 20.72, 32.09]), while the region with the highest age-standardized prevalence of glaucoma-related blindness and MSVI was Sub-Saharan Africa. Between 2000 and 2020, global age-standardized prevalence of glaucoma-related blindness among adults ≥50 years decreased by 26.06% among males (95% UI: 25.87, 26.24), and by 21.75% among females (95% UI: 21.54, 21.96), while MSVI due to glaucoma increased by 3.7% among males (95% UI: 3.42, 3.98), and by 7.3% in females (95% UI: 7.01, 7.59).
Conclusions
Within the last two decades, glaucoma has remained a major cause of blindness globally and regionally.
Similar content being viewed by others
Introduction
Glaucoma refers to a group of ocular conditions united by a clinically characteristic optic neuropathy [1]. Although treatment by lowering intraocular pressure (IOP) can arrest or slow its deterioration in most cases, glaucoma remains the most common cause of irreversible blindness worldwide [2]. The more common chronic forms of glaucoma are usually asymptomatic until later stages of the disease, when individuals may present with advanced visual field loss and can progress to complete loss of vision. Primary open-angle glaucoma (POAG), is the most common subtype and risk factors include age, elevated IOP, sub-Saharan African ethnic origin, positive family history, and high myopia. Primary angle-closure glaucoma (PACG), is a visually devastating form characterised by an ocular anatomical predisposition particularly prevalent in East Asians.
A meta-analysis by Tham et al. in 2013, using data from 50 population-based studies that used case definitions based on specific structural or functional evidence of glaucomatous optic neuropathy, estimated the number of people (aged 40-80 years) with glaucoma worldwide to be 64.3 million, increasing to 76.0 million in 2020 and 111.8 million in 2040 [3]. A more recent meta-analysis estimated that POAG affected 68.56 million (95% confidence interval (95% CI), 59.99–79.98), 2.4% (95% CI, 2.0–2.8) of the global population older than 40 years [4]. However, for individuals and society, the burden of a disease is more important than just the presence of a disease including its early subjectively asymptomatic stages. Often population-based glaucoma studies did not report on the number of people blind or visually impaired due to glaucoma; however, over the last few decades, many more population-based eye surveys have been conducted with improved methods of glaucoma case detection and reporting of glaucoma-related vision loss. Using data from population-based studies conducted between 1980-2012 and collated within the Global Vision Database, the Vision Loss Expert Group (VLEG; an international ophthalmic epidemiology reference group) working with the Global Burden of Disease Study reported on the number of individuals visually impaired or blind due to glaucoma, examined regional differences and for the first time reported the temporal changes for the period from 1990 to 2012. Using an ongoing systematic literature review, VLEG has continued to update the Global Vision Database with more population-based datasets. In this current meta-analysis, we (VLEG) report the number of people affected by glaucoma-related blindness and MSVI in 2020, the change between 2000 and 2020, and differences by region and sex.
Methods
The first stage of data preparation included a systematic review of published (between Jan 1, 1980, and Oct 1, 2018) population-based studies of vision impairment and blindness by the VLEG that also included grey literature sources. Eligible studies from this review were combined with data from Rapid Assessment of Avoidable Blindness (RAAB) studies. Data from the US National Health and Nutrition Examination Survey and the World Health Organization (WHO) Study on Global Ageing and Adult Health were provided by the GBD team. More detailed methods are published elsewhere [5, 6] and briefly discussed as follows.
In total, the VLEG identified 137 studies and extracted data from 70 studies in their 2010 review, and an additional 67 studies in their 2014–18 review. Studies were primarily national and subnational cross-sectional surveys. Additionally, the VLEG commissioned the preparation of 5-year age-disaggregated RAAB data from the RAAB repository [7]. Studies were included if they met the following criteria: visual acuity measured using a test chart that could be mapped to the Snellen scale, and a sample that was representative of the population. Self-report of vision loss was excluded. We used the International Classification of Diseases 11th edition criteria for vision loss, as applied by the WHO, which categorizes people according to vision in the better eye on presentation [8]. Moderate vision loss is defined as a visual acuity of 6/60 or better but less than 6/18, severe vision loss as a visual acuity of 3/60 or better but less than 6/60, and blindness as a visual acuity of less than 3/60 or less than 10° visual field around central fixation; however, in practice, visual field data from population-based eye surveys are scarce.
First, we separated raw data into vision-loss envelopes for all-cause moderate, and severe vision loss, and blindness. Data were input into a mixed-effects meta-regression tool developed by the Institute for Health Metrics and Evaluation (IHME) called MR-BRT (meta-regression; Bayesian; regularised; trimmed) [9]. Presenting vision impairment was the reference definition for each level of severity. Undercorrected refractive error data were extracted directly from data sources where available and otherwise calculated by subtracting best-corrected vision impairment from presenting vision impairment prevalence for each level of severity in studies that reported both measures for a given location, sex, age group, and year. All other causes were quantified as part of the best-corrected estimates of vision impairment at each level of severity.
We modelled distance vision impairment and blindness due to the following causes: cataracts, undercorrected refractive error, age-related macular degeneration, myopic macular degeneration, glaucoma, diabetic retinopathy, and other causes of vision impairment (in aggregate). The minimum age for inclusion of data for these causes was set at 20 years for cataract and diabetic retinopathy, and 45 years for glaucoma and age-related macular degeneration. Other vision impairment estimates were combined with less prevalent causes of vision impairment to create a residual category (e.g., retinopathy of prematurity, vitamin A deficiency, trachoma).
We produced location, year, age, and sex-specific estimates of MSVI and blindness using Disease Modelling Meta-Regression (Dismod-MR) 2.1 [10]. The data processing steps are described elsewhere [6]. Briefly, Dismod-MR 2.1 models were run for all vision impairment by severity (moderate, severe, blindness) regardless of cause and, separately, for MSVI and blindness due to each modelled cause of vision impairment (e.g., MSVI due to cataract and blindness due to cataract). Then, models of MSVI due to specific causes were split into moderate and severe estimates using the ratio of overall prevalence in the all-cause moderate presenting vision impairment and severe presenting vision impairment models. Next, prevalence estimates for all causes by severity were scaled to the models of all-cause prevalence by severity. This produced final estimates by age, sex, year, and location for each individual cause of vision impairment by severity. We age-standardized our estimates using the GBD standard population [11].
Results
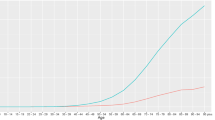
According to our estimates from 2020, approximately 3.61 million (95% uncertainty intervals (UIs): 2.81, 4.42) people were blind and 4.14 million (95% UI: 3.24, 5.18) were visually impaired (MSVI) globally because of glaucoma (Table 1). An estimated 1.89 million males and 1.72 million females of all ages, and 1.89 million males and 1.71 million females aged ≥50 years were blind due to glaucoma in 2020 (Table 2). The number of males and females (all ages) with glaucoma-related MSVI in 2020 was 2.00 million and 2.14 million, respectively, whereas an estimated 2.00 million and 2.14 million people were aged 50 years and over (Table 3).
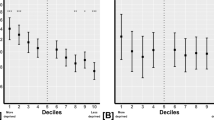
Glaucoma caused 8.39% (95% UI: 6.54, 10.29) of all blindness in 2020 worldwide. Regionally, the highest proportion of blindness attributed to glaucoma was found in high-income countries (26.12% [95% UI: 20.72, 32.09]) and North Africa and Middle East (14.98% [95% UI: 11.47, 18.72]) (Table 1). The regions with the lowest proportion of glaucoma-related blindness of all blind individuals were South Asia (4.85% [UI: 3.69, 6.10]), and Southeast Asia, East Asia, and Oceania (5.02% [95% UI: 3.83, 6.37]). Glaucoma caused 1.41% (95% UI: 1.10, 1.75) of all cases with MSVI in 2020 worldwide. Latin America and Caribbean (2.04% [95% UI: 1.60, 2.55]), high-income countries (1.92% [95% UI: 1.51, 2.46]) and Sub-Saharan Africa (1.92% [95% UI: 1.51, 2.42]) were regions with the highest percentage of glaucoma-related MSVI of all individuals with MSVI (Table 1).
In 2020, the global age-standardized prevalence of glaucoma-related blindness in those aged ≥50 years was 0.20% (95% UI: 0.16, 0.25) and for glaucoma-related MSVI was 0.23% (95% UI: 0.18, 0.29) (Table 1). The region with the highest age-standardized prevalence of glaucoma-related blindness was Sub-Saharan Africa (0.66% [95% UI: 0.52, 0.81]). The lowest age-standardized prevalence of glaucoma blindness in 2020 was in the regions of Central Europe, Eastern Europe, and Central Asia (0.12% (95% UI: 0.10, 0.15). The regions with the highest age-standardized prevalence of glaucoma-related MSVI in 2020 were Sub-Saharan Africa (0.46% [95% UI: 0.36, 0.57]), and Latin America and the Caribbean (0.39% [95% UI: 0.30, 0.48]). The lowest figures were found in high-income countries (0.11% [95% UI: 0.09, 0.14]) and Central Europe, Eastern Europe, and Central Asia (0.15% [95% UI: 0.12, 0.19]) (Table 1).
Between 2000 and 2020, the global percentage change in age-standardized prevalence of glaucoma-related blindness among adults ≥50 years improved by 26.06% (95% UI: 25.87, 26.24) among males and by 21.75% in females (95% UI: 21.54, 21.96) (Table 4). A large reduction (26-39%) in the age-standardized prevalence of glaucoma-related blindness amongst adults aged ≥50 years (both sexes) was found in Southeast Asia, East Asia and Oceania (−38.99% [95% UI: −39.16, −38.82]), South Asia (−35.75% [95% UI: −35.93, −35.57]), North Africa and Middle East (−30.04% [95% UI: −30.23, −29.84]), and Central Europe, Eastern Europe, and Central Asia (−26.62% [95% UI: −26.81, −26.43]) with more modest reductions in Latin America and the Caribbean (−14.47% [95% UI: −14.71, −14.24]), Sub-Saharan Africa (−16.85% [95% UI: −17.06, −16.64]) and high-income countries (-8.71% [95% UI: -8.95, -8.48]) (Table 4). There were minimal differences between males and females in respect of the reduction in age-standardized prevalence of glaucoma blindness across regions (Table 4).
Between 2000 and 2020, the global percentage change in age-standardized prevalence of glaucoma MSVI among adults (≥50 years) increased among males (3.7% [95% UI: 3.42, 3.98]) and females (7.3% [95% UI: 7.01, 7.59]) (Table 5). Southeast Asia, East Asia and Oceania were the only world regions where a substantial increase in the age-standardized prevalence of glaucoma MSVI was observed for both sexes (18.43%, [95% UI: 18.11, 18.75]) with more modest increases in Sub-Saharan Africa (1.71% [95% UI: 1.44, 1.98]) and high-income countries (1.65% [95% UI: 1.36, 1.95]). Reductions in glaucoma MSVI were noted in the other regions where the reduction was slightly greater among females than males. In Sub-Saharan Africa, the increase in the age-standardized prevalence of glaucoma-related MSVI was much greater among females (3.24% [95% UI:2.96, 3.52]) than among males (0.75% [95% UI:0.48, 1.02]).
Discussion
Glaucoma was the cause for blindness in 3.61 million people or 8.4% of the 43.3 million blind people globally in 2020, and glaucoma was the cause for MSVI in 4.14 million people or 1.4% of the 295 million people visually impaired in 2020 [6]. Our previous publication on vision loss due to glaucoma in 2010 reported lower numbers affected by blindness (2.1 million) and similar numbers with MSVI (4.2 million) [12]. In this most recent analysis, glaucoma was ranked as the second leading cause of blindness (after cataract) and fourth leading cause of MSVI, and therefore the most common cause of irreversible blindness, and the second most common cause of irreversible MSVI [6]. These figures highlight the importance of glaucoma as a public health concern, and it should be noted that these are almost certainly underestimations due to methodological issues where blindness prevalence surveys (in particular those of rapid design) often assign the most “treatable” disease as the primary cause of blindness assuming that cataract is more treatable than glaucoma. Furthermore, in advanced glaucoma, individuals may meet WHO perimetric-based definitions of blindness (<10 degrees of central field in the better eye) whilst retaining normal visual acuity. Hence, as visual field data is rarely collected in population-based surveys, a potentially large but unknown number of individuals are misclassified as visually unimpaired when they may be, in fact, glaucoma blind. Additionally, the definition of MSVI does not include perimetric criteria, though non-blinding visual field loss certainly results in vision impairment.
There is increasing global pressure on health-care resources due to the changing demographics of the population. The number of people aged 65 years and older is expected to increase from 700 million to 1.5 billion in the next 30 years, with the largest increases in low- and middle-income countries (LMICs). This will result in populations undergoing “epidemiological transition” and experiencing a higher prevalence of diseases associated with higher development and aging, including glaucoma [3, 13, 14]. Glaucoma disproportionately accounted for a greater proportion of blindness than it did for MSVI. The percentage of blindness caused by glaucoma showed regional variations, with relatively low figures in regions with relatively young populations such as South Asia, South-East Asia and Oceania, and Latin America and the Caribbean, and with relatively high figures in regions with relatively old populations such as the high-income regions (Table 1). Bucking this trend were the regions of North Africa and Middle East and Sub-Saharan Africa, both with younger populations than the median global age but with a relatively high contribution of glaucoma to blindness, most probably on account of these regions having the highest age-standardized prevalence of glaucoma-related blindness. Glaucoma causes a particular challenge as many LMICs experience these demographic changes. Due to the typically lengthy asymptomatic phase, it is well documented that in high-income countries, less than half of glaucoma is diagnosed [15, 16]. In LMICs, this proportion increases to over 90% and approximately 35% of patients are estimated to be blind at diagnosis [17,18,19,20]. Furthermore, the higher prevalences on the African continent are almost certainly due in part to lack of or insufficient access to treatment.
It is encouraging to note that between 2000 and 2020, the global percentage change in age-standardized prevalence of glaucoma-related blindness among adults ≥50 years has decreased (-26.06% [95% UI: -26.24, -25.87] among males and females (-21.75% [95% UI: -21.96, -21.54] (Table 4). We identified only two studies that have reported reductions in glaucoma-related blindness incidence, both from high-income countries. A recent analysis of the Finnish Register of Vision Impairment and a social insurance register found that the incidence of reported vision impairment in those with treated glaucoma had reduced by a third over 40 years, from 32/100,000 in the 1980s to 21/100,000 in the 2010-19 decade, with no sex differences [21]. This Finnish study reported that the proportion of overall vision impairment had increased in recent decades to approximately 50% suggesting better glaucoma care and earlier diagnosis, and this may be reflected in their finding that the age of onset of reported glaucoma-related vision impairment increased in more recent decades [21]. The Olmsted County (Minnesota, USA) population-based study reported that the 20-year probability of progression to glaucoma-related blindness in at least one eye had decreased from 26% for subjects diagnosed in 1965-1980 to 13% for those diagnosed in 1981-2000 [22]. In our analysis, reductions in age-standardized prevalence of glaucoma-related blindness between 2000-2020 in Latin America and Caribbean and Sub-Saharan Africa were not as marked as that for other LMIC regions. These data highlight the urgent need for improved eye health care in these regions, including a sustainable capacity to diagnose and treat glaucoma at earlier stages.
In all regions, in 2020, the age-standardized prevalence of glaucoma-related blindness was higher in males than in females. In Central Asia and high-income countries, the age-standardized prevalence of MSVI-related blindness was higher in females than in males, while in other regions there was no sex difference. Male gender has been found to be a significant risk factor for POAG in several studies [4, 23]. Women are well documented to be at a higher risk of PACG, the less prevalent but more blinding form of glaucoma [24]. The underlying reasons for the different gender-related predispositions are unclear but will be multifactorial, such as differential access to health systems.
Less encouraging than the temporal change in glaucoma blindness, was the finding that between 2000 and 2020, the mean global age-standardized prevalence of glaucoma-related MSVI among adults (≥50 years) had increased among males (3.70% [95% UI: 3.42, 3.98]) and females (7.30% [95% UI: 7.01, 7.59]) (Table 5). These increases took place mainly in Southeast Asia, East Asia and Oceania, Sub-Saharan Africa, and high-income countries. These data suggest a triaging phenomenon: although efforts to contain glaucoma blindness have had some success, the availability of current resources is not meeting the demands at visually significant but lower thresholds of visual impairment. The observed increase in glaucoma-related MSVI may be interpreted as an improvement if more cases are detected at an earlier stage before the onset of blindness.
The design of our study had potential limitations. First, as we discussed in our report of the global prevalence of vision loss, a significant limitation was that many countries lacked data across the time period, or that there was only sub-national data available [5]. Second, the majority of population-based studies within the database that reported on vision loss due to glaucoma did not disaggregate their reported findings into glaucoma diagnostic subtypes such as POAG and PACG; therefore, we could not differentiate between glaucoma subtypes in our analysis. Third, as mentioned above, protocol dictated that population-based studies will report one cause as the principal cause for an individual examined in that individual study so that causal prevalence can be calculated. In situations where multiple disorders contribute equally to visual loss, only the “most easily preventable” or the “most readily curable” cause is usually recorded [25] which underestimates the impact of diseases such as glaucoma and diabetic retinopathy. It may hold true in particular for patients with cataracts in which the ophthalmoscopical examination of the optic nerve is obscured leading to underdetection of glaucomatous optic nerve damage. Strengths of this study included a large amount of population-based data accessed and utilized and the trend analysis of causes of vision impairment and blindness, usage of non-linear age trends and modelling of data that were not reported by age, systematic quantitative analysis and reporting of uncertainty intervals. The large size of the network of ophthalmic researchers involved in first identification and then evaluation of data sources allowed access to unpublished materials and permitted us to obtain additional unpublished data from study investigators who had only published summary data, to evaluate all the major vision impairment studies, and to include only studies that met specific inclusion criteria regarding population representativeness and clear description and definition of visual acuity procedures.
Given the high prevalence of glaucoma and vision impairment secondary to glaucoma, the economic and social burden of the condition is substantial. Diagnosed individuals often require lifelong treatment and monitoring, which requires significant individual-level patient and carer support, for example, with adherence to treatment, and training of ophthalmologists and allied health professionals. Solutions to these challenges of diagnosis and ongoing monitoring may arrive through the innovative use of new community care models, availability of home monitoring of both intraocular pressure (IOP) and visual field function, and implementation of screening programs [26,27,28]. Early detection, both opportunistic and with targeted screening of those with higher genetic risk, is also important as is improved awareness of glaucoma. In addition to government systems, permissive regulations in some countries may be required to allow various models of health care delivery to function as well as possible. The recently published ‘Package of Eye Care Interventions’ by the World Health Organization provides a useful set of recommended, evidenced-based glaucoma care interventions with material resources required for implementation, health promotion and prevention, screening, diagnosis and monitoring, treatment, and rehabilitation [29]. These and other resources are necessary to facilitate policy-makers and technical decision-makers across countries to integrate glaucoma care into the packages and policies of their national health services.
Summary
What was known before
-
Globally, in 2020, 3.61 million people were blind and nearly 4.14 million were visually impaired by glaucoma.
What this study adds
-
The contribution of glaucoma to blindness and moderate and severe vision impairment (MSVI) by region and the change in this contribution between 2000-2020 The change in global age-standardized prevalence of glaucoma-related blindness and MSVI between 2000 and 2020 and the differences by sex and region.
Data availability
Data sources for the Global Vision Database are listed at the following weblink http://www.anglia.ac.uk/verigbd. Fully disaggregated data is not available publicly due to data sharing agreements with some principal investigators yet requests for summary data can be made to the corresponding author.
References
Casson RJ, Chidlow G, Wood JP, Crowston JG, Goldberg I. Definition of glaucoma: clinical and experimental concepts. Clin Exp Ophthalmol. 2012;40:341–9.
Flaxman SR, Bourne RRA, Resnikoff S, Ackland P, Braithwaite T, Cicinelli MV, et al. Global causes of blindness and distance vision impairment 1990-2020: a systematic review and meta-analysis. Lancet Glob Health. 2017;5:e1221–e1234.
Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology. 2014;121:2081–90.
Zhang N, Wang J, Li Y, Jiang B. Prevalence of primary open angle glaucoma in the last 20 years: a meta-analysis and systematic review. Sci Rep. 2021;11:13762.
Bourne RRA, Steinmetz JD, Flaxman S, Briant PS, Taylor HR, Resnikoff S, et al. Trends in prevalence of blindness and distance and near vision impairment over 30 years: an analysis for the Global Burden of Disease Study. Lancet Global Health. 2021;9:e130–e143.
Steinmetz JD, Bourne RRA, Briant PS, Flaxman SR, Taylor HRB, Jonas JB, et al. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: the Right to Sight: an analysis for the Global Burden of Disease Study. Lancet Global Health. 2021;9:e144–e160.
RAAB Repository. http://raabdata.info (accessed 1 February 2023).
International Classification of Diseases. Icd.who.int (accessed 1 February 2023).
GBD 2019 Diseases, Injuries, and Impairments Collaborators. Global burden of 359 diseases, injuries, and impairments, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–22.
GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1789–858.
Vollset SE, Goren E, Yuan C-W, Cao J, Smith AE, Hsiao T, et al. Fertility, mortality, migration, and population scenarios for 195 countries and territories from 2017 to 2100: a forecasting analysis for the Global Burden of Disease Study. Lancet. 2020;396:1285–306.
Bourne RR, Taylor HR, Flaxman SR, Keeffe J, Leasher J, Naidoo K, et al. Number of people blind or visually impaired by glaucoma worldwide and in world regions 1990–2010: a meta-analysis. PLoS One. 2016;11:e0162229.
Burton MJ, Ramke J, Marques AP, Bourne RRA, Congdon N, Jones I, et al. The Lancet Global Health Commission on Global Eye Health: vision beyond 2020. Lancet Glob Health. 2021;9:e489–e551. https://doi.org/10.1016/s2214-109x(20)30488-5.
Omran AR. The epidemiologic transition. A theory of the epidemiology of population change. Milbank Mem Fund Q. 1971;49:509–38.
Topouzis F, Coleman AL, Harris A, Koskosas A, Founti P, Gong G, et al. Factors associated with undiagnosed open-angle glaucoma: the Thessaloniki Eye Study. Am J Ophthalmol. 2008;145:327–35.
Shaikh Y, Yu F, Coleman AL. Burden of undetected and untreated glaucoma in the United States. Am J Ophthalmol. 2014;158:1121–9.
Abdull MM, Gilbert CC, Evans J. Primary open angle glaucoma in northern Nigeria: stage at presentation and acceptance of treatment. BMC Ophthalmol. 2015;15:111. https://doi.org/10.1186/s12886-015-0097-9.
Buhrmann RR, Quigley HA, Barron Y, West SK, Oliva MS, Mmbaga BB. Prevalence of glaucoma in a rural East African population. Invest Ophthalmol Vis Sci. 2000;41:40–8.
Kyari F, Entekume G, Rabiu M, Spry P, Wormald R, Nolan W, et al. A Population-based survey of the prevalence and types of glaucoma in Nigeria: results from the Nigeria National Blindness and Visual Impairment Survey. BMC Ophthalmol. 2015;15:176. https://doi.org/10.1186/s12886-015-0160-6.
Ramakrishnan R, Nirmalan PK, Krishnadas R, Thuasiraj RD, Tielsch JM, Katz J, et al. Glaucoma in a rural population of southern India: the Aravind comprehensive eye survey. Ophthalmology. 2003;110:1484–90. https://doi.org/10.1016/s0161-6420(03)00564-5.
Vaajanen A, Purola P, Ojamo M, Gissler M, Uusitalo H. Changes in incidence and severity of visual impairment due to glaucoma during 40 years - a register-based study in Finland. Acta Ophthalmol. 2022;100:534–40.
Malihi M, Moura Filho ER, Hodge DO, Sit AJ. Long-term trends in glaucoma-related blindness in Olmsted County, Minnesota. Ophthalmology. 2014;121:134–41.
Rudnicka AR, Mt-Isa S, Owen CG, Cook DG, Ashby D. Variations in primary open-angle glaucoma prevalence by age, gender, and race: A Bayesian meta-analysis. Invest Ophthalmol Vis Sci. 2006;47:4254–61.
George R, Panda S, Vijaya L. Blindness in glaucoma: primary open-angle glaucoma versus primary angle-closure glaucoma-a meta-analysis. Eye. 2022;36:2099–105.
World Health Organization. Coding instructions for the WHO/PBL eye examination record (version III). PBL/88.1. Available: http://www.who.int/ncd/vision2020_actionplan/documents/pbl_88_1.pdf.
Che Hamzah J, Daka Q, Azuara-Blanco A. Home monitoring for glaucoma. Eye (Lond). 2020;34:155–60. https://doi.org/10.1038/s41433-019-0669-7.
Li Z, He Y, Keel S, Meng W, Chang RT, He M. Efficacy of a deep learning system for detecting glaucomatous optic neuropathy based on color fundus photographs. Ophthalmology. 2018;125:1199–206.
Aspberg J, Heijl A, Bengtsson B. Screening for open-angle glaucoma and its effect on blindness. Am J Ophthalmol. 2021;228:106–16.
Keel S, Lingham G, Misra N, Block S, Bourne R, Calonge M, et al. Toward universal eye health coverage-key outcomes of the World Health Organization package of eye care interventions: a systematic review. JAMA Ophthalmol. 2022;140:1229–38.
Funding
This study was funded by Brien Holden Vision Institute, Fondation Thea, Fred Hollows Foundation, Bill & Melinda Gates Foundation, Lions Clubs International Foundation (LCIF), Sightsavers International, and University of Heidelberg.
Author information
Authors and Affiliations
Consortia
Contributions
Please see Appendix for more detailed information about individual author contributions to the research, divided into the following categories: managing the overall research enterprise; writing the first draft of the manuscript; primary responsibility for applying analytical methods to produce estimates; primary responsibility for seeking, cataloguing, extracting, or cleaning data; designing or coding figures and tables; providing data or critical feedback on data sources; developing methods or computational machinery; providing critical feedback on methods or results; drafting the manuscript or revising it critically for important intellectual content; and managing the estimation or publications process.
Corresponding authors
Ethics declarations
Competing interests
O C Baltatu reports support for the present manuscript from the National Council for Scientific and Technological Development (CNPq, 304224/2022-7) and Anima Institute (AI) research professor fellowship; leadership or fiduciary roles in board, society, committee or advocacy groups, paid or unpaid as an advisory member of the Health and Biotechnology Board at Sao Jose dos Campos Technology Park, and as an academic ambassador for Afya (UNINOVAFAPI); outside the submitted work. A Bron reports payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing or educational events from Thea; outside the submitted work. M Cenderadewi reports grants or contracts from James Cook University for the International Research Training Program Scholarship for their doctoral study; support for attending the Research Training Program Minimum Resource Funds to fun conference related travel from James Cook University; all outside the submitted work. X Dai reports support for the present manuscript from the Institute for Health Metrics and Evaluation (University of Washington) for their salary. A Dastiridou reports support for attending meetings/travel from Thea Laboratories and Abbvie; outside the submitted work. D S Friedman reports grants or contracts to their institution for research from Genentech; consulting fees from Abbvie, Kaliyope, Life Biosciences, Bausch and Lomb; payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing or educational events from Thea Pharmaceuticals; support for attending meetings and travels from Thea Pharmaceuticals; leadership or fiduciary roles in board, society, committee or advocacy groups, paid or unpaid with Orbis International as a Member of the Board of Governors; outside the submitted work. V B Gupta reports grants or contracts from National Health and Medical Research Council (NHMRC) provided to Deakin University; outside the submitted work. V K Gupta reports grants or contracts from National Health and Medical Research Council (NHMRC) provided to Macquarie University; outside the submitted work. I Ilic reports support for the present manuscript from the Ministry of Education, Science and Technological development, Republic of Serbia (project No 175042, 2011-2023). J H Kempen reports stock or stock options with Betaliq and Tarsier; outside the submitted work. K Krishan reports non-financial support from the UGC Centre of Advanced Study, CAS II, awarded to the Department of Anthropology, Panjab University (Chandigarh, India); outside the submitted work. J L Leasher reports leadership or fiduciary roles in board, society, committee or advocacy groups, unpaid as a member of the National Eye Institute National Eye Health Education Program planning committee; outside the submitted work. J A Singh reports consulting fees from AstraZeneca, Crealta/Horizon, Medisys, Fidia, PK Med, Two labs Inc., Adept Field Solutions, Clinical Care options, Clearview healthcare partners, Putnam associates, Focus forward, Navigant consulting, Spherix, MedIQ, Jupiter Life Science, UBM LLC, Trio Health, Medscape, WebMD, Practice Point communications, and the National Institutes of Health and the American College of Rheumatology; payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing or educational events from the speaker’s bureau of Simply Speaking; support for attending meetings from OMERACT as a member of the steering committee; participation on an Advisory Committee with the FDA Arthritis Advisory Committee; leadership or fiduciary roles in board, society, committee or advocacy groups, paid or unpaid as a past steering committee member of the OMERACT, an international organization that develops measures for clinical trials and receives arms length funding from 12 pharmaceutical companies, Co-Chair of the Veterans Affairs Rheumatology Field Advisory Committee, and the editor and Director of the UAB Cochrane Musculoskeletal Group Satellite Center on Network Meta-analysis; stock or stock options in Atai Life Sciences, Kintara Therapeutics, Intelligent Biosolutions, Acumen Pharmaceutical, TPT Global Tech, Vaxart Pharmaceuticals, Atyu Biopharma, Adaptimmune Therapeutics, GeoVax Labs, Pieris Pharmaceuticals, Enzolytics Inc., Seres Therapeutics, Tonix Pharmaceuticals Holding Corp., and Charlotte’s Web Holdings, Inc, as well as previously owned stock options in Amarin, Viking and Moderna Pharmaceuticals; outside the submitted work. J D Steinmetz reports support for the present manuscript from the Bill and Melinda Gates Foundation IHME funding for GBD analyses. J H V Ticoalu reports other financial or non-financial interests as a co-founder of Benang Merah Research Center; outside the submitted work. A Bron reports payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing or educational events from Théa. M A Del Monte reports support for attending meetings and/or travel from the University of Michigan, and leadership or fiduciary roles in board, society, committee or advocacy groups, paid or unpaid as past president of Costenbader Society. D Friedman reports grants or contracts from any entity from Genentech (to the institution for research); consulting fees from Abbvie, Kaliyope, Life Biosciences and Bausch and Lomb; payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing or educational events from Thea Pharmaceuticals; support for attending meetings and/or travel from Thea Pharmaceuticals; and leadership or fiduciary role in other board, society, committee or advocacy group, paid or unpaid, from Orbis International as member of board of governors. J M Furtado reports consulting fees from Pan American Health Organization and from Lions Club International Foundation. G Gazzard reports consulting fees from Alcon Laboratories, Inc; Allergan, Inc; BELKIN Vision LTD; Carl Zeiss Meditec; Elios; Genentech/Roche; Reichert; Théa and ViaLase; payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing or educational events from Alcon Laboratories, Inc; BELKIN Vision Ltd; Carl Zeiss Meditec; Elios and Ellex; participation on a Data Safety Monitoring Board or Advisory Board with Alcon Laboratories, Inc; Allergan, Inc; BELKIN Vision Ltd; Carl Zeiss Meditec; Elios and Visufarma; and leadership or fiduciary role in other board, society, committee or advocacy group, paid or unpaid with Glaucoma UK Medical Advisory Board and UK&Eire Glaucoma Society as president. M E Hartnett reports support for the present manuscript (e.g., funding, provision of study materials, medical writing, article processing charges, etc.) from Michael F. Marmor, M.D. Professor of Retinal Science and Disease as endowment to support salary; grants or contracts from any entity (from National Eye Institute R01 EY017011 and National Eye Institute R01 EY015130) as partial salary support; patents planned, issued or pending (WO2015123561A2 and WO2021062169A1); and leadership or fiduciary role in other board, society, committee or advocacy group, paid or unpaid with Jack McGovern Coats’ Disease Foundation and as director of Women’s Eye Health and Macular Society Grant Review Chair. J H Kempen reports stock or stock options with Betaliq ($25,000 buy in, starup company developing IOP-lowering eyedrop) and Tarsier ($50,000 buy in, startup company developing anti-inflammatory eyedrop). J E Kim reports consulting fees from Genentech/Roche, DORC, Notal Vision and Outlook Therapeutics (all as payment to J E Kim); participation on a Data Safety Monitoring Board or Advisory Board with Allergan, Amgen, Apellis, Bausch&Lomb, Clearside, Coherus, Novartis and Regeneron (all as participation on advisory board); leadership or fiduciary role in other borad, society, committee or advocacy group, paid or unpaid, with AAO, APRIS, ASRS, Macular Society and NAEVR/AEVR (all unpaid); and receipt of equipment, materials, drugs, medical writing, gifts or other services from Clearside and Genentech/Roche (both for medical writing). V C Lansingh reports consulting fees from HelpMeSee (as an employee); and support for attending meetings and/or travel from HelpMeSee (pay airfare and hotel). J Leasher reports leadership or fiduciary role in other board, society, committee or advocacy group, paid or unpaid with National Eye Institute (as a member) and National Eye Health Education Program planning committee (unpaid). M Nowak reports participation on a Data Safety Monitoring Board or Advisory Board with Vision Express Co. Poland as the chairman of medical advisory board of Vision Express Co. Poland. P Ramulu reports grants or contracts from National Institute of Health and Perfuse Therapeutics; and consulting fees from Alcon and W. L. Gore. F Topouzis reports grants or contracts from Théa, Omikron, Pfizer, Alcon, Abbvie and Bayer (all paid to Institution); consulting fees from Omikron, Théa and Bausch & Lomb (all paid to Topouzis); payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing or educational events from Omikron (paid to Topouzis), Abbvie and Roche (both paid to Institute); and leadership or fiduciary role in other board, society, committee or advocacy group, paid or unpaid with European Glaucoma Society (as president), Greek Glaucoma Society (as president) and Board of Governors, World Glaucoma Association (all unpaid).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Vision Loss Expert Group of the Global Burden of Disease Study., the GBD 2019 Blindness and Vision Impairment Collaborators. Global estimates on the number of people blind or visually impaired by glaucoma: A meta-analysis from 2000 to 2020. Eye (2024). https://doi.org/10.1038/s41433-024-02995-5
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41433-024-02995-5