Abstract
Background
To estimate global and regional trends from 2000 to 2020 of the number of persons visually impaired by cataract and their proportion of the total number of vision-impaired individuals.
Methods
A systematic review and meta-analysis of published population studies and gray literature from 2000 to 2020 was carried out to estimate global and regional trends. We developed prevalence estimates based on modeled distance visual impairment and blindness due to cataract, producing location-, year-, age-, and sex-specific estimates of moderate to severe vision impairment (MSVI presenting visual acuity <6/18, ≥3/60) and blindness (presenting visual acuity <3/60). Estimates are age-standardized using the GBD standard population.
Results
In 2020, among overall (all ages) 43.3 million blind and 295 million with MSVI, 17.0 million (39.6%) people were blind and 83.5 million (28.3%) had MSVI due to cataract blind 60% female, MSVI 59% female. From 1990 to 2020, the count of persons blind (MSVI) due to cataract increased by 29.7%(93.1%) whereas the age-standardized global prevalence of cataract-related blindness improved by −27.5% and MSVI increased by 7.2%. The contribution of cataract to the age-standardized prevalence of blindness exceeded the global figure only in South Asia (62.9%) and Southeast Asia and Oceania (47.9%).
Conclusions
The number of people blind and with MSVI due to cataract has risen over the past 30 years, despite a decrease in the age-standardized prevalence of cataract. This indicates that cataract treatment programs have been beneficial, but population growth and aging have outpaced their impact. Growing numbers of cataract blind indicate that more, better-directed, resources are needed to increase global capacity for cataract surgery.
Similar content being viewed by others
Introduction
For 2020, the Global Burden of Disease (GBD) Study reported that cataract remained the leading cause of blindness, with approximately 15.2 million cases [95% Uncertainty Interval (UI): 12.7–18.0) that comprised 45% of global blindness [1]. Cataract also remained the second leading cause of moderate and severe vision impairment (MSVI), with 78.8 million (95% UI: 67.2–91.4) people, which comprised 39% of global MSVI. In spite of global advocacy efforts, such as the VISION 2020 Right to Sight program undertaken by the World Health Organization and International Agency of the Prevention Blindness, and an increase in cataract surgical rates (the number of cataract surgeries per million population) reported across the world, the progress made against cataract has revealed substantial inequality and inequity, with lower-to-middle income countries (LMICs) shouldering the greater burden and having poorer visual outcomes than high-income countries [2,3,4].
The majority of cataracts are age-related nuclear cataracts, which typically cause vision loss in the sixth decade or later [5,6,7]. Cataracts, part of the spectrum of diabetic eye disease, are also increasing due to a global epidemic of diabetes, with diabetics more likely to develop cataracts and more quickly lose their vision to cataract compared to people without diabetes [5, 8, 9].
Surgery is the only treatment for cataract, during which an artificial intraocular lens replaces the damaged lens. Cataract surgery is extremely efficacious in terms of restoring sight, and multiple studies have demonstrated its cost-effectiveness, which appears to increase over time [10,11,12]. In 2015, the International Council of Ophthalmology estimated that globally, there were 14 ophthalmologists performing cataract surgery per million population, but that ranges from less than 1 cataract surgeon per million in low-income countries to as high as 32 in high-income countries, further revealing the global inequity in access to eye care [13]. Age-related cataract exposes another persistent inequity in universal eye health coverage–– men are 1.7 times more likely to undergo cataract surgery than women, and even in high-income countries, women are more likely to wait longer for surgery and experience poorer outcomes [14]. This gender inequity is partially due to the fact that women live longer than men, although sociocultural barriers are also at play. Based on the 2015 GBD Vision Loss Expert Group data, if women had the same access to cataract surgery as men, the blindness burden of cataract could decrease by 11%. However, women, in fact, need more access to surgery than men, to address the gender inequity [14]. Gender differences in cataract burden for 2020 have yet to be analyzed.
With the publication of 2020 GBD vision loss data, there is a need to explore further the global and regional trends in cataract burden since 1990 and better understand the regional and gender inequities of cataract burden. The objective of this article is to provide updated estimates of the global burden of vision loss due to cataract, disaggregated by sex and region, for the period from 2000 to 2020 covered by Global Vision 2020. This is done using the best available ophthalmic epidemiological database, the Global Vision Database which is a comprehensive, continuously updated, online database of ophthalmic epidemiological data curated by the Vision Loss Expert Group (VLEG) [15,16,17]. Additionally, we assess progress against the goals set out in ‘Towards universal eye health: global action plan 2014–2019 of the World 60 Health Assembly (2013) [18]. This Global Action Plan set a target to reduce the prevalence of avoidable blindness by 25% from 2010 to 2019.
Methods
The VLEG have maintained, and progressively updated a systematic review of population-based studies of vision impairment and blindness published between Jan 1, 1980, and Oct 1, 2018, including gray literature sources. Data from this systematic review were combined with data from the repository of Rapid Assessment of Avoidable Blindness (RAAB) studies, and data contributed by the GBD obtained from the US National Health and Nutrition Examination survey and the WHO Study on Global Ageing and Adult Health. Detailed methods are published elsewhere [17, 19], and briefly described herein.
In total, the systematic review identified 137 studies, and the VLEG extracted data from 70 studies in 2010, and a further 67 studies in 2014–18 [16]. Studies were primarily national and subnational cross-sectional surveys. The VLEG commissioned the preparation of 5-year age-disaggregated data from the RAAB repository [20]. Studies were included if they met these criteria: population-representative and visual acuity measured using a test chart that could be mapped to Snellen fractions. Studies using self-reported vision loss were excluded. We used the International Classification of Diseases 11th edition criteria for vision loss, as recommended by the WHO, which categorizes people according to presenting better-eye visual acuity. The classification defines moderate vision loss as better eye visual acuity of 6/60 or better but worse than 6/18, severe vision loss as a visual acuity of 3/60 or better but worse than 6/60, and blindness as visual acuity of worse than 3/60 or less than 10° visual field around central fixation.
Data were stratified into datasets including so-called vision-loss envelopes (as per Flaxman et al. [16]) for all-cause mild, moderate, and severe vision loss, and blindness. Data were input into a mixed-effects meta-regression tool developed by the Institute for Health Metrics and Evaluation (IHME) called MR-BRT (meta regression; Bayesian; regularized; trimmed) [21]. Presenting vision impairment defined each level of severity. Prevalence data for under-corrected refractive error were extracted where available, and otherwise calculated by subtracting best-corrected vision impairment from presenting vision impairment for each level of severity in studies that reported both measures for a given location, sex, age group, and year. Other causes were quantified as part of the best-corrected estimates of vision impairment at each level of severity. Minimum age for inclusion of data was defined as 20 years for cataract.
We generated location, year, age, and sex-specific estimates of MSVI and blindness using Disease Modeling Meta-Regression (Dismod-MR) 2.1; [19] the data processing steps are described elsewhere [17]. In brief, Dismod-MR 2.1 models were run for all vision impairment strata (moderate, severe, blindness) regardless of cause and, separately, for MSVI and blindness for each modeled cause of vision impairment. Then, models of MSVI due to cataract were split into moderate and severe estimates using the ratio of overall prevalence in the all-cause moderate presenting vision impairment and severe presenting vision impairment models. Next, prevalence estimates for cataract were stratified by severity were scaled to the models of all-cause prevalence by severity. This produced final estimates by age, sex, year, and location for cataract vision impairment stratified by severity. We age-standardized our estimates using the GBD standard population [22]. Data on blindness and MSVI due to AMD were presented by seven super-regions (Southeast Asia/East Asia/Oceania, Central Europe/Eastern Europe/Central Asia, High-income, Latin America and Caribbean, North Africa and Middle East, South Asia, and Sub-Saharan Africa) and globally. Data on other causes of vision impairment and blindness will be presented in separate publications.
The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
In 2020, 17.01 million (all ages, 95% uncertainty interval (UI) 14.40–19.93) people were blind due to cataract (Table 1). This breaks down by gender as 6.78 million (95% UI 5.73–7.98) men and 10.22 million (95% UI 8.76–11.96) women blind from cataract (Table 2). The majority of these are over 50 years of age with 15.17 million (95% UI 12.70–18.00) so affected (Table 1). Of these, 5.96 million (95% UI 4.98–7.11) men and 9.22 million (95% UI 7.73–10.88) women are blind from cataract (Table 2).
Overall, 83.48 million (95% UI 71.76–96.98) people are estimated to have MSVI from cataract (Table 1). Of these 34.59 million (95% UI 29.69–39.95) are men, and 48.89 million (95% UI 42.05–56.06) are women (Table 3). Again, the majority are over 50 years of age, 78.79 million (95% UI 67.20–91.40) people, 32.41 million (95% UI 27.55–37.74) men and 46.38 million (95% UI 39.66–53.66) women suffer from MSVI due to cataract (Tables 1 and 3).
Cataract caused 39.55% (95% UI: 33.48, 46.34%) of all blindness in 2020 worldwide. Regionally, the highest proportion of cataract-related blindness was found in South Asia (53.20 [95% UI: 45.00, 62.11%]) and Southeast Asia, East Asia, and Oceania (41.82% [95% UI: 35.30, 49.38]) (Table 1). The regions with the lowest proportion of all cataract-related blindness of all blind individuals were High Income Countries (16.82% [UI: 13.66, 20.60]), and Central Europe, Eastern Europe, and Central Asia (20.53% [95% UI: 16.50, 25.15]). Cataract caused 28.30% (95% UI: 24.32, 32.54) of all cases with MSVI in 2020 worldwide. Southeast Asia, East Asia, and Oceania (34.00 (29.32-39.00)% [95% UI: 29.32, 39.00]), and South Asia (29.87% [95% UI: 25.64, 34.83]) were regions with the highest percentage of cataract-related MSVI of all visually impaired individuals (Table 1).
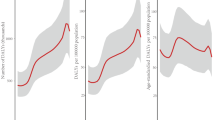
In 2020, the global age-standardized prevalence of cataract-related blindness in those aged ≥50 years was 0.84% (95% UI: 0.70, 0.99) and for cataract-related MSVI was 1.01% (95% UI: 0.87, 1.15) (Table 1). The variation of crude prevalence with age is shown in Fig. 1. The regions with the highest age-standardized prevalence of cataract-related blindness were South Asia (2.23% [95% UI: 1.89, 2.61]) and Sub-Saharan Africa (1.49% [95% UI: 1.24, 1.78]). The lowest age-standardized prevalence of cataract blindness in 2020 was in the regions of High Income Countries (0.09% [95% UI: 0.07, 0.11]) and Central Europe, Eastern Europe, and Central Asia (0.19% [95% UI: 0.15, 0.23]). The regions with the highest age-standardized prevalence of cataract-related MSVI in 2020 were South Asia (2.15% [95% UI: 1.85, 2.49]), and North Africa and the Middle East (1.33% [95% UI: 1.13, 1.55]). The lowest figures were found in high-income countries (0.35% [95% UI: 0.30, 0.40]) and Central Europe, Eastern Europe, and Central Asia (0.49% [95% UI: 0.41, 0.58]) (Table 1). The variation in these results by gender across the regions are shown in Tables 2 and 3.
Between 2000 and 2020, the global percentage change in age-standardized prevalence of cataract-related blindness among adults ≥50 years decreased by 27.54% (95% UI: −27.68, −27.39), among males by −31.78% (95%UI −31.91, −31.64) and by 24.82% in females (95% UI: −24.97, −24.68) (Table 4). However, the absolute number of cases (unadjusted for age) increased by 29.72% (95% UI: 29.46, 29.98), in males 25.65% (95% CI 25.39, 25.92) and in females 32.49% (95% CI: 32.23, 32.75). An especially large reduction in the age-standardized prevalence of cataract-related blindness amongst adults aged ≥50 years (both sexes) was found in Southeast Asia, East Asia and Oceania (−42.99% [95% UI: −43.10, −42.88]), North Africa and Middle East (−39.97% [95% UI: −40.13, −39.81]) and South Asia (−36.53% [95% UI: −36.65, −36.41]), with a modest reduction in high-income countries (−6.86% [95% UI: −7.10, −6.62]) (Table 4). The greatest percentage increases in absolute number of cases were in Latin America and the Caribbean 71.25% (95% UI 70.86, 71.64) and in high income countries 49.30 (95% UI 48.92, 49.69). Only Central Europe, Eastern Europe, and Central Asia showed a reduction in the caseload (−4.40% [95% UI −4.66, −4.14].
Between 2000 and 2020, the global percentage change in age-standardized prevalence of cataract MSVI among adults ( ≥ 50 years) increased (7.17% [95% UI: 6.98, 7.36]), among males (4.70% [95% UI 4.52, 4.89]) and females (8.94% [95% UI: 8.75, 9.13]) (Table 5). However, the absolute number of cases increased by 93.11% (95% UI: 92.75, 93.46), in males 93.69% (95% CI 93.32, 94.05) and in females 92.70% (95% CI: 92.36, 93.04). Sub-Saharan Africa (2.29% [95%UI 2.12, 2.47]) and Southeast Asia, East Asia and Oceania 1.96% [95%UI 1.78, 2.13]) were the only world regions where a substantial increase in the age-standardized prevalence of cataract MSVI was observed with notable decreases in South Asia (-5.53 [95% UI: -5.69, -5.37]) and Latin America and Caribbean (-4.83% [95% UI: -5.01, -4.65]). The increase in the absolute number of cataract MSVI cases was greatest in Southeast Asia, East Asia, and Oceania (115.21% [95%UI 114.83, 115.58]), and least in Central Europe, Eastern Europe, and Central Asia (38.18% [95%UI 37.87, 38.49]) (Table 5).
Discussion
Cataract, the world’s leading cause of blindness, remains one of the greatest opportunities in global health to make impactful and cost-effective contributions. Cataract surgery is safe and highly effective with both higher and lower technology approaches (e.g., phacoemulsification or extracapsular techniques respectively), and can be provided relatively inexpensively [23]. As a surgical condition, it requires a system able to provide one-at-a-time clinical care, like most causes of blindness and visual impairment. There are various eye service delivery models that can be used to address the cataract burden. However, it makes sense to combine it in a system with other ophthalmic services, ethically addressing other issues that will come to the attention of the service as well as providing a more professional-friendly work environment to retain capable eye care professionals (ophthalmologists, optometrists, eye nurses and others).
As an endemic condition, the ideal approach to the problem is to develop sufficient capacity and health system functionality to make ophthalmic surgery widely available worldwide. Given the relatively low level of infrastructure and consumables required for quality surgery, government health systems are well positioned to address this issue for the economically poorest persons. While funding limitations may constrain their systems’ scale [24], cataract surgery has considerable economic and quality of life benefits compared to its cost [10], which can offset the investment. Moreover, several health systems in different locations have demonstrated that self-sustaining services can be provided at costs most patients are willing to pay while also generating surpluses to provide service to the very poor [25, 26]. Such “cross-subsidizing” systems have made a large contribution to alleviating cataract blindness in much of the world, although these require a dominant service provider e.g. Aravind Eye Care System in South India. Systems for eye care should contemplate the value of ”patient financial contribution” for cataract surgery as much as possible; offering universal free or highly subsidized surgery may unnecessarily leave that health care financing resource at the table. In addition, surgical campaigns have been used extensively to deal with “backlogs” in cataract blindness; these are ideal for unreached/remote areas where development is unlikely to reach the cataract blind on a reasonable time scale without interfering with the ultimate solution of local capacity development. Our data demonstrate that these sorts of efforts have been fruitful in reducing the per capita levels of cataract blindness over the last 20 years over much of the world. Indeed, the World Health Assembly Global Action Plan target of a 25% reduction from 2010 to 2019 in avoidable vision impairment (WHA 66.3 24/5/2013) was met for cataract blindness (from an age-adjusted prevalence perspective) [18].
However, the successes have not kept pace with the impact of population growth and aging, with the result that the number of cataract blind is substantially increasing. Cataract also remains the leading cause of blindness despite these improvements and its favorable treatability. Thus, further investment in sustainable health systems able to provide quality cataract surgeries is likely to provide very substantial societal and economic net benefits. Because development is a long-term proposition, sustained commitment will be needed, whether through committed funders (e.g., government or charity programs) or self-sustaining organizations (private non-profit or social enterprise systems, or government systems allowing cost recovery).
While our data demonstrate a notable improvement in blindness (worse than 20/400 visual acuity), we did not see a similar decrease in MSVI (worse than 20/60 to 20/400) which also is associated with substantial disability/economic impact [27, 28]. Indeed, MSVI became more prevalent and nearly doubled in the number of cases. This pattern suggests successful targeting of the most severely impaired cases, albeit at the neglect of the less severely impaired. However, MSVI also needs to be targeted to alleviate visual disability and its socioeconomic impacts [27, 28]. Indeed, research into willingness to pay for cataract surgery suggests that people in the MSVI range (e.g., younger people otherwise capable of employment) may be more willing to pay for cataract surgery than more severe “blind” persons [26]. Expansion of the indications for cataract surgery may be needed to accomplish improvements in cataract MSVI also [29].
The WHO criteria score blindness and visual impairment based on the vision in the better eye. Following this logic, it would seem sensible in an economically constrained environment to focus on operating one eye. However, second eye surgeries also have important benefits to vision, visual ability and well-being [30, 31], and has been shown to have very high cost-effectiveness (cost per quality-adjusted life year gained) and a favorable cost-effectiveness in an evidence-based review [32, 33]. In addition, second eye surgery provides insurance that vision could continue in the event something happened to the first eye for persons in locations with poor service access. Binocular vision is important for activities requiring depth perception, falls prevention, increases contrast sensitivity and provides better binocular visual acuity than single eye surgery alone [31]. Because case finding of second eye cataracts and second eye operations have less marginal cost for bilateral cases than first eye cataracts [34], it is desirable to operate second eyes as well. Persons also may be more willing to pay for a cataract surgery after seeing the result of first eye cataract surgery [33]. Second eye cataract surgeries generally should be made available to patients in cataract programs, especially if patients are willing to pay some or all of the cost.
While improvements in cataract blindness were observed over the last 20 years, huge disparities in the prevalence remain between low- and high-income regions. South Asia has the highest number of cataract blind and by far the highest prevalence, a significant focus in this super region has the greatest potential for improvement. However, other poor regions (e.g., Sub-Saharan Africa) which are expected to see a growth in the elderly population in coming years and have a very high prevalence of cataract blindness amongst the elderly needing aggressive efforts to develop an eye care system capable of handling the volume of cataract surgery and other eye care services which can be forecast to be needed. Given the very low number of ophthalmologists and other eye care professionals in these areas, the time is now to strengthen and expand both training and systems for eye care delivery [34].
Our results demonstrated again that women are disproportionately represented amongst the cataract blind and visually impaired, and that the inequity is widening. The extent of this difference varies across the globe, but is generally consistent. The difference might reflect differences in family willingness to pay for male and female surgery [35]. Differences in acceptance of surgery between males and females could be another explanation. However, acceptance of clinical services tends to be higher among women than men in high income settings. Notably, female survival is generally longer than male survival which might be associated with a higher burden of age-related cataract even if service utilization were equal. Baruwa et al found that five years’ access to free cataract screening and low-cost high quality cataract surgery was associated with equalization in willingness to pay for cataract surgery across males and females [36]. Improving cataract surgery quality, community knowledge of the benefits of cataract surgery, and reducing barriers to surgical access likely are among the core strategies that need to be implemented in order to overcome the male-female gap in cataract surgery utilization. Without foregoing the promotion of cataract surgery among males, who also need to increase cataract surgery utilization, female surgery promoters and other strategies to increase female use of cataract surgery also could be helpful to reduce the disproportionately higher female cataract blindness and visual impairment burden.
The impact of the COVID-19 pandemic on cataract blindness is unclear at this time. Emerging evidence that service delivery was adversely affected during the emergency phase of the pandemic may drive the cataract burden up [37]. This may be offset by global decreases in life expectance from the disease and its sequelae [37]. These impacts may not be visible for several years, but are likely to be overwhelmed by existing trajectories of population growth and ageing.
In summary, as the population grows and ages while coverage of cataract surgery remains incomplete, immense numbers of people remain blind and vision impaired from cataract. These numbers are expected to continue growing markedly as the population increases and ages worldwide, especially in the least developed countries with young but rapidly aging populations and high cataract blindness/MSVI prevalence. While much has been achieved by initiatives to tackle cataract blindness, much more needs to be done to provide cataract surgery to those in need. Programs for delivering cataract to the vision impaired should not only target the blind, but also those with MSVI who also substantially benefit from treatment and appear to be under-targeted. High quality service provision is essential for inciting demand for cataract surgery, and thus is a key issue along with increasing the number of surgeries. Ophthalmologist training, which takes a long time, needs to be developed urgently in areas of insufficient coverage. Eye care systems in which ophthalmologists can operate successfully and other eye care professionals can work successful also are very important. While all regions with substantial numbers of cataract blind need increased services, females especially need to access cataract surgery more. Culturally appropriate efforts to promote female cataract surgery are an important piece of what needs to be done. Globally, immense increases in resource mobilization for treating cataract are required. All sources of healthcare financing need to be tapped to develop sustainable eye care systems able to tackle the cataract problem with high quality surgery.
Summary
What was known before
-
Globally, in 2020, 17.0 million people were blind and nearly 83.5 million were visually impaired by cataract.
What this study adds
-
The contribution of cataract to blindness and moderate and severe vision impairment (MSVI) by region and the change in this contribution between 2000 and 2020. The change in global age-standardized prevalence of cataract-related blindness and MSVI between 2000 and 2020 and the differences by sex and region.
References
GBD 2019 Blindness and Vision Impairment Collaborators; Vision Loss Expert Group of the Global Burden of Disease Study. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: the Right to Sight: an analysis for the Global Burden of Disease Study. Lancet Glob Health. 2021;9:e144–e160.
Wang W, Yan W, Fotis K, Prasad NM, Lansingh VC, Taylor HR, et al. Cataract surgical rate and socioeconomics: a global study. Invest Ophthalmol Vis Sci. 2016;57:5872–81.
Lou L, Wang J, Xu P, Ye X, Ye J. Socioeconomic disparity in global burden of cataract: an analysis for 2013 with time trends since 1990. Am J Ophthalmol. 2017;180:91–96.
Wang W, Yan W, Müller A, He M. A global view on output and outcomes of cataract surgery with national indices of socioeconomic development. Invest Ophthalmol Vis Sci. 2017;58:3669–76.
Lim JC, Caballero Arredondo M, Braakhuis AJ, Donaldson PJ. Vitamin C and the lens: new insights into delaying the onset of cataract. Nutrients. 2020;12:3142.
Hodge WG, Whitcher JP, Satariano W. Risk factors for age-related cataracts. Epidemiol Rev. 1995;17:336–46.
Age Related Eye Disease Group. Risk factors associated with age-related nuclear and cortical cataract: a case-control study in the Age-Related Eye Disease Study, AREDS Report No. Ophthalmology. 2001;108:1400–8.
Klein BE, Klein RE, Moss SE. Incidence of cataract surgery in the Wisconsin Epidemiologic Study of Diabetic Retinopathy. Am J Ophthalmol. 1995;119:295–300.
Caird FI, Garrett CJ. Progression and regression of diabetic retinopathy. Proc R Soc Med. 1962;55:477–9.
Lansingh VC, Carter MJ, Martens M. Global cost-effectiveness of cataract surgery. Ophthalmology. 2007;114:1670–8.
Lansingh VC, Carter MJ. Use of global visual acuity data in a time trade-off approach to calculate the cost utility of cataract surgery. Arch Ophthalmol. 2009;127:1183–93.
Brown GC, Brown MM, Busbee BG. Cost-utility analysis of cataract surgery in the United States for the year 2018. J Cataract Refract Surg. 2019;45:927–38.
Resnikoff S, Lansingh VC, Washburn L, Felch W, Gauthier TM, Taylor HR, et al. Estimated number of ophthalmologists worldwide (International Council of Ophthalmology update): will we meet the needs? Br J Ophthalmol. 2020;104:588–92.
Lou L, Ye X, Xu P, Wang J, Xu Y, Jin K, et al. Association of sex with the global burden of cataract. JAMA Ophthalmol. 2018;136:116–21.
Bourne RRA, Flaxman SR, Braithwaite T. Magnitude, temporal trends, and projections of the global prevalence of blindness and distance and near vision impairment: a systematic review and meta-analysis. Lancet Glob Health. 2017;5:e888–e897.
Flaxman SR, Bourne RRA, Resnikoff S. Global causes of blindness and distance vision impairment 1990-2020: a systematic review and meta-analysis. Lancet Glob Health. 2017;5:e1221–e1234.
Steinmetz JD, Bourne RA, Briant PS, Flaxman SR, Taylor HRB, Jonas JB, et al. GBD 2019 Blindness and Vision Impairment Collaborators; Vision Loss Expert Group of the Global Burden of Disease Study. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: the Right to Sight: an analysis for the Global Burden of Disease Study. Lancet Glob Health. 2021;9:e144–e160. https://doi.org/10.1016/S2214-109X(20)30489-7.
WHO. Universal eye health: a global action plan 2014–2019. World Health Organization; Geneva: 2013. https://www.who.int/publications/i/item/universal-eye-health-a-global-action-plan-2014-2019.
James SL, Abate D, Hassan Abate K, Abay SM, Abbafati C, Abbasi N, et al. GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1789–858. https://doi.org/10.1016/S0140-4906736(18)32279-7
RAAB Repository. 2023. http://raabdata.info. accessed 1 February 2023.
Vos T, Lim SS, Abbafati C, Abbas KM, Abbasi M, Abbasifard M, et al. GBD 2019 Diseases, Injuries, and Impairments Collaborators. Global burden of 359 diseases, injuries, and impairments, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–22. https://doi.org/10.1016/S0140-6736(20)30925-9.
Vollset SE, Goren E, Yuan C-W, Cao J, Smith A, Hsiao T, et al. Fertility, mortality, migration, and population scenarios for 195 countries and territories from 2017 to 2100: a forecasting analysis for the Global Burden of Disease Study. Lancet. 2020;396:1285–306. https://doi.org/10.1016/S0140-4956736(20)30677-2
Powe NR, Schein OD, Gieser SC, Tielsch JM, Luthra R, Javitt J, et al. Synthesis of the literature on visual acuity and complications following cataract extraction with intraocular lens implantation. Cataract Patient Outcome Research Team. Arch Ophthalmol. 1994;112:239–52. https://doi.org/10.1001/archopht.1994.01090140115033.
Muralikrishnan R, Venkatesh R, Prajna NV, Frick KD. Economic cost of cataract surgery procedures in an established eye care centre in Southern India. Ophthalmic Epidemiol. 2004;11:369–80. https://doi.org/10.1080/09286580490888762.
Le HG, Ehrlich JR, Venkatesh R, Srinivasan A, Kolli A, Haripriya A, et al. A Sustainable Model For Delivering High-Quality, Efficient Cataract Surgery In Southern India. Health Aff. 2016;35:1783–90. https://doi.org/10.1377/hlthaff.2016.0562.
He M, Chan V, Baruwa E, Gilbert D, Frick KD, Congdon N. Willingness to pay for cataract surgery in rural Southern China. Ophthalmology. 2007;114:411–6. https://doi.org/10.1016/j.ophtha.2006.09.012.
Lundstrom M, Behndig A, Kugelberg M, Montan P, Stenevi U, Pesudovs K. The outcome of cataract surgery measured with the Catquest-9SF. Acta Ophthalmol. 2011;89:718–23. https://doi.org/10.1111/j.1755-3768.2009.01801.x.
Marques AP, Ramke J, Cairns J, Butt T, Zhang JH, Jones I, et al. The economics of vision impairment and its leading causes: A systematic review. EClinicalMedicine. 2022;46:101354. https://doi.org/10.1016/j.eclinm.2022.101354.
Vashist P, Senjam SS, Gupta V, Gupta N, Kumar A. Definition of blindness under National Programme for Control of Blindness: Do we need to revise it? Indian J Ophthalmol. 2017;65:92–96. https://doi.org/10.4103/ijo.IJO_869_16.
Shekhawat NS, Stock MV, Baze EF, Daly MK, Vollman DE, Lawrence MG, et al. Impact of First Eye versus Second Eye Cataract Surgery on Visual Function and Quality of Life. Ophthalmology. 2017;124:1496–503. https://doi.org/10.1016/j.ophtha.2017.04.014.
Gothwal VK, Wright TA, Lamoureux EL, Khadka J, McAlinden C, Pesudovs K. Improvements in visual ability with first-eye, second-eye, and bilateral cataract surgery measured with the visual symptoms and quality of life questionnaire. J Cataract Refract Surg. 2011;37:1208–16. https://doi.org/10.1016/j.jcrs.2011.01.028.
Busbee BG, Brown MM, Brown GC, Sharma S. Cost-utility analysis of cataract surgery in the second eye. Ophthalmology. 2003;110:2310–7. https://doi.org/10.1016/S0161-6420(03)00796-6.
Frampton G, Harris P, Cooper K, Lotery A, Shepherd J. The clinical effectiveness and cost-effectiveness of second-eye cataract surgery: a systematic review and economic evaluation. Health Technol Assess. 2014;18:1–205. https://doi.org/10.3310/hta18680.
Dean WH, Buchan JC, Gichuhi S, Faal H, Mpyet C, Resnikoff S, et al. Ophthalmology training in sub-Saharan Africa: a scoping review. Eye. 2021;35:1066–83. https://doi.org/10.1038/s41433-020-01335-7.
Ibrahim N, Ramke J, Pozo-Martin F, Gilbert CE. Willingness to pay for cataract surgery is much lower than actual costs in Zamfara state, northern Nigeria. Ophthalmic Epidemiol. 2018;25:227–33. https://doi.org/10.1080/09286586.2017.1408845.
Baruwa E, Tzu J, Congdon N, He M, Frick KD. Reversal in gender valuations of cataract surgery after the implementation of free screening and low-priced high-quality surgery in a rural population of southern China. Ophthalmic Epidemiol. 2008;15:99–104. https://doi.org/10.1080/09286580801999118.
Ung L, Jonas JB, Lietman TM, Chodosh J. COVID-19 and the Unfinished Agenda of VISION 2020. Am J Ophthalmol. 2021;224:30–35. https://doi.org/10.1016/j.ajo.2020.11.016.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pesudovs, K., Lansingh, V.C., Kempen, J.H. et al. Global estimates on the number of people blind or visually impaired by cataract: a meta-analysis from 2000 to 2020. Eye (2024). https://doi.org/10.1038/s41433-024-02961-1
Published:
DOI: https://doi.org/10.1038/s41433-024-02961-1