Abstract
Purpose
To study the changes in corneal nerves and corneal sensitivity over a 6-month period in patients with herpes zoster ophthalmicus (HZO) compared with healthy subjects.
Methods
This was a prospective longitudinal study on patients with newly diagnosed HZO. In vivo confocal microscopy (IVCM) corneal nerve parameters and corneal sensitivity were measured and compared between eyes with HZO, contralateral eyes and controls at baseline, 2 and 6 months.
Results
Fifteen subjects with HZO and 15 healthy age and sex matched controls were recruited. HZO eyes revealed a reduction in corneal nerve branch density (CNBD) from baseline to 2 months (9.65 ± 5.75 vs. 5.90 ± 6.87/mm2, p = 0.018), and decreased corneal nerve fibre density (CNFD) at 2 months when compared with control (p = 0.025). However, these differences resolved by 6 months. HZO fellow eyes demonstrated increased corneal nerve fibre area (CNFA), corneal nerve fibre width (CNFW) and corneal nerve fractal dimension (CNFrD) at 2 months compared with baseline (p = 0.025, 0.031, 0.009). There was no change in corneal sensitivity for both HZO affected and HZO fellow eyes from baseline or over time, nor was it different from sensitivity in controls.
Conclusion
Corneal denervation was present at 2 months in HZO eyes, with an observed recovery by 6 months. HZO fellow eyes demonstrated increased corneal nerve parameters at 2 months, which could represent a proliferative response to nerve degeneration. IVCM is useful in monitoring corneal nerve changes, and is more sensitive in detecting nerve alterations than esthesiometry.
Similar content being viewed by others
Introduction
Herpes zoster (HZ) is a relatively common condition leading to significant morbidity and mortality, with an incidence of 4–4.5 per 1000 person-years [1]. Despite the availability of vaccines, the age-specific incidence of HZ is still rising, along with its disease burden [2]. Among the elderly population, HZ carries a mortality rate of 61 per 100,000 in those aged 65 or above [3]. HZ is caused by the reactivation of the varicella zoster virus (VZV) from its dormant state. Following a primary infection (chickenpox), the VZV virus remains latent in the dorsal ganglion. When viral reactivation involves the ophthalmic division of the trigeminal nerve, the condition is termed herpes zoster ophthalmicus (HZO), accounting for 10–20% of all HZ cases [4].
HZO classically presents with a unilateral painful skin rash along the dermatomal distribution of the first and/or second branch of the trigeminal nerve, with or without ocular involvement. The cornea, which is the most densely innervated tissue in our body, is susceptible to a spectrum of manifestations at every layer. These include epithelial keratitis, stromal keratitis, endotheliitis, and neurotrophic keratopathy. The trigeminal nerve contributes to blinking and tearing mechanisms, and releases neuromediators and growth factors to aid healing of the cornea. Any insult to the ophthalmic branch of the trigeminal nerve may lead to denervation of the cornea, a loss of protective mechanisms and trophic support, resulting in the development of neurotrophic keratitis [5].
In recent years, the use of in vivo confocal microscopy (IVCM) has gained a bigger role in the diagnosis and monitoring of corneal diseases [6,7,8], but the number of IVCM studies in this relatively common condition of HZO were limited to case reports or small series [9,10,11,12]. Significant alterations of corneal nerves were detected in a patient at 2 years after onset of HZO, including scarce non-branching subbasal nerves and even absence of subbasal nerves in the affected eye [9]. Contralateral eyes of HZO also demonstrated a loss of corneal nerves to a lesser degree [10]. The dendritiform cell densities of both eyes were shown to increase in unilateral HZO stroma at 57 months, suggesting that the immune activation and inflammatory process could persist long after the active stages of the disease [11].
The trigeminal nerve, being one of the twelve cranial nerves, belongs to the peripheral nervous system, and therefore carries regenerative potentials. When injured, Wallerian degeneration of the distal portion initiates a cascade of neurotransmitters that allows the proximal nerve end to regenerate and rewire into the distal portion [13]. There has only been one study demonstrating corneal nerve regeneration in HZO. Cruzat et al. studied two patients with HZO over time, and demonstrated nerve regeneration by IVCM and partial recovery of corneal sensation in one patient 5 years after the initial episode of HZO [12]. In post-LASIK eyes, various studies have reported the occurrence of nerve regeneration ranging from 54 days to 6 months after LASIK [14,15,16].
Studies on early corneal nerve changes following HZO are lacking. This information may impact the follow up and monitoring for neurotrophic keratitis in HZO patients. To date, there has been no longitudinal study on the course of corneal nerve alteration in HZO patients. We aim to study the morphology of the corneal nerves in the acute stage, and subsequent intermediate terms following HZO in both the affected and contralateral eyes, using healthy subjects as control. We will attempt to identify clinical features that are associated with such changes in the corneal nerves.
Methods
We conducted a prospective longitudinal study comparing patients with a clinical diagnosis of HZO to healthy controls. Three groups of eyes were compared—affected eyes of HZO (Group A), fellow eyes of HZO (Group B), and normal eyes from healthy subjects (Group C). The study adhered to the tenets of the Declaration of Helsinki and was approved by the joint Chinese University of Hong Kong—New Territories East Cluster Clinical Research Ethics Committee (2020.394). All subjects were recruited from the Prince of Wales Hospital ophthalmology clinic, and written informed consent was obtained before participation.
Inclusion and exclusion criteria
Patients with unilateral HZO who had an onset of symptoms within 2 weeks were recruited. The diagnosis was made based on clinical presentation of a characteristic maculopapular or vesicular rash and pain in the ophthalmic branch of the trigeminal nerve. Age and sex matched participants were then recruited in a 1:1 ratio during their follow up, provided that the below inclusion and exclusion criteria were met.
Immunocompromised patients, patients with poorly controlled diabetes mellitus (HbA1c > 6.5%), and those with a history of previous HZO in either eye, corneal dystrophy, keratouveitis, infectious keratitis, ocular trauma, regular contact lens wear, significant ocular surface disease (including severe dry eyes) and intracranial surgery or central nervous system abnormalities affecting the function of trigeminal ganglia were excluded. Patients with multi-dermatomal involvement were not recruited. Subjects with any prior intraocular or keratorefractive surgeries were also excluded.
Sample size calculation
The sample size was calculated based on Hamrah’s study which identified a difference of 1662 µm in mean corneal nerve density between eyes with HZO and healthy controls at 5.1 years from disease onset [10]. We hypothesised a smaller reduction in corneal nerve density at 2 and 6 months from disease onset. Based on an 80% study power and an alpha value of 0.05, 12 subjects per arm was required in order to detect a 1000 μm difference in corneal nerve densities between HZO eyes and healthy controls. In order to factor in a buffer of 20% dropout rate, we targeted to recruit 15 participants per arm.
Study outcomes
The primary outcome of this study was the subbasal corneal nerve fibre density CNFD (number of fibres per mm2) at 0, 2 and 6 months measured by IVCM. Secondary outcomes included corneal nerve branch density (CNBD), corneal nerve fibre length (CNFL), corneal nerve fibre total branch density (CTBD), corneal nerve fibre area (CNFA), corneal nerve fibre width (CNFW), and corneal nerve fibre fractal dimension (CNFrD) and corneal sensitivity measured by Cochet-Bonnet esthesiometer at baseline, 2 and 6 months.
Study procedure
All subjects were recruited and examined by the principal investigator [M.E.]. Demographic data were collected from patients. A complete ocular examination including pinhole visual acuity (VA), slit lamp biomicroscopy and dilated fundal examination was performed.
For the HZO group, the presence of Hutchinson’s sign (vesicles affecting the tip of the nose) at presentation and any ocular involvement were documented, including blepharitis (defined as lid swelling and hyperaemia), conjunctivitis (defined as diffuse conjunctival injection, graded 0–4 based on CCLRU grading scale), scleritis (defined as scleral injection, graded 0–4 based on standardised grading system [17]), episcleritis (defined as episcleral injection, graded 0–4), epithelial keratitis (punctate epithelial keratitis/pseudo-dendrite), stromal keratitis (nummular keratitis/deep stromal keratitis), endotheliitis, uveitis (graded 0–4 based on SUN classification [18]), retinitis (acute retinal necrosis/progressive outer retinal necrosis) and papillitis. Apart from examinations at baseline, 2 months and 6 months, patients were followed up according to their clinical progress, and managed based on their clinical presentation. All HZO patients were given a 7–10 day course of oral antiviral at presentation, with further continuation in patients with unresolved scleritis and uveitis. Topical antiviral ointment was added to patients with epithelial keratitis, episcleritis and scleritis. Topical steroid was prescribed to patients with episcleritis, scleritis, anterior uveitis, stromal keratitis and endotheliitis. Medications were tapered according to clinical response (i.e. resolution of keratitis, improvement in conjunctival/episcleral/scleral injection, reduction in anterior chamber activity). At each study visit, IVCM was performed and the corneal sensitivities were measured for both eyes.
For the control group, only one eye was selected for examination. When both eyes of a control fulfil the recruitment criteria, one eye was randomly chosen (www.randomizer.org). IVCM was performed in the same manner, and the corneal sensitivity was measured. As the rate of age-related corneal nerve reduction in the normal population is slow (0.2088 mm/mm2 per year) [19], it was assumed that neither corneal nerve parameters nor corneal sensitivity would show significant change at 6 months; hence these measurements were not repeated in the control group.
In vivo confocal microscopy
IVCM (Heidelberg Retina Tomograph III Rostock Cornea Module) was performed on both eyes after measurement of the corneal sensation. One drop of topical tetracaine hydrochloride 0.5% was instilled into each eye. A speculum was inserted only if there was significant eyelid swelling preventing adequate contact between the camera and the cornea. A sterile, single-use disposable cap (TomoCap) was used for each subject, after applying GenTeal Gel (hypromellose 0.3%) into the cap as a coupling agent. The subbasal nerve plexus was imaged using a method validated by Takhar et al. [20]. A 5 × 5 dot grid system was placed in front of the fellow eye of the subject. Subjects were asked to fixate on the target red dot on the system, while the operator identified the central whorl of the subbasal nerve plexus. Once the central whorl was identified, subjects were instructed to look along the dots on the grid, from left to right, row by row, as one image was captured at each dot. A total of at least 25 images were acquired per eye.
Images of the subbasal corneal nerve plexus were then analysed with ACCMetrics, which is a validated fully automated corneal nerve analysis software [21]. Seven parameters were generated: (1) corneal nerve fibre density (CNFD)—number of fibres per mm2, (2) corneal nerve branch density (CNBD)—number of branch points on the main fibres per mm2, (3) corneal nerve fibre length (CNFL)—total length of nerves in mm per mm2, (4) corneal nerve fibre total branch density (CTBD)—total number of branch points per mm2, (5) corneal nerve fibre area (CNFA)—total nerve fibre area mm2 per mm2, (6) corneal nerve fibre width (CNFW)—average nerve fibre width mm per mm2, and (7) corneal nerve fibre fractal dimension (CFracDim)—a measure of corneal nerve complexity. The mean values of all 25 images per eye were used for data analysis.
Corneal sensitivity
Corneal sensitivity of the central cornea was measured using Cochet-Bonnet esthesiometer. A thin nylon monofilament was extended to its full length of 60 mm. It was then retracted in 5 mm increments until the patient could feel its touch on the cornea. Two repeated measurements reaching the same value were obtained.
Data analysis
The SPSS statistical software was used for data analysis. Age and corneal sensitivity were reported by mean and standard deviation. Baseline VA was reported by median and interquartile range. The gender distribution and laterality of eyes were reported by proportions. The number and percentage of patients of each clinical manifestation of HZO were presented. Normality is checked with Shipiro–Wilk test and non-parametric tests were used for data not following a normal distribution. Mann–Whitney U test was used to compare IVCM parameters and corneal sensitivity between the three groups. Repeated measures analysis of variance (ANOVA) was used to examine across different time points. A p value of ≤0.05 was considered statistically significant.
Results
Demographics
Fifteen HZO patients were recruited (9 males and 6 females, mean age: 57.7 ± 16.1 years old). Three of them defaulted follow up after the first visit as they were asymptomatic and declined to further return during the COVID-19 pandemic. All the remaining 12 patients completed the three visits of the study. Fifteen normal controls were recruited (8 males and 7 females, mean age: 58.3 ± 17.3 years old). There was no difference in laterality of eyes between the HZO group and control (p = 0.715). Both groups were homogenous and no statistical differences were present for age and gender (p = 0.775, 0.713). One patient in the HZO group had diabetes mellitus with a HbA1c level of 6.3%. For the control group, five subjects had diabetes mellitus but none had a HbA1c exceeding 6.5%. Demographic data were summarised in Table 1.
Clinical characteristics
The mean presenting visual acuity of the affected eyes of the HZO group was 0.18 ± 0.25 logMAR. The visual acuity at 2 months and 6 months remained unchanged at 0.15 ± 0.34 logMAR and 0.15 ± 0.31 logMAR, respectively (p = 0.424 and 0.304). Blepharitis (46.7%) and conjunctivitis (33.3%) were the most frequent findings noted with HZO. None of the patients developed stromal keratitis, endotheliitis, or posterior segment involvement. The mean duration of topical steroids was 20.3 ± 39.6 days. The mean durations of topical and oral antivirals were 17.1 ± 17.1 days and 14.3 ± 40.2 days. None of the patients had clinical recurrence of disease within the 6-month study period.
HZO eyes showed reduction in CNBD at 2 months which returned to baseline at 6 months
The IVCM parameters were summarised in Table 2. In HZO affected eyes, there was a decrease in CNBD from baseline (9.65 ± 5.75/mm2) to 2 months (5.90 ± 6.87/mm2) (p = 0.018). This reduction was no longer present at 6 months (p = 0.564). Other IVCM parameters of HZO eyes did not show significant interval change during the 6 months.
HZO eyes had lower CNBD and CNFD at 2 months compared to normal eyes
In comparison to healthy eyes, significantly lower CNBD and the CNFD values were identified at 2 months. These differences were resolved by 6 months (p = 0.126, 0.103).
We analysed a subgroup of patients with Hutchinson’s sign (n = 4) or epithelial keratitis (n = 4), of which two patients had both signs (Fig. 1). When compared with controls, these eyes showed significant reduction not only in CNBD and CNFD at 2 months (p = 0.002, and <0.001), but also in CNFL and CTBD at 2 months (p = 0.025, and 0.042), and CNFD at 6 months (p = 0.033).
Fellow eyes of HZO showed significant increase in CNFA, CNFW and CNFrD at 2 months
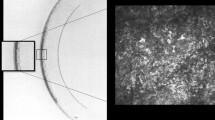
The reductions in CNBD and CNFD seen in HZO affected eyes were not observed in the fellow eyes. In contrast, there were significant increases in CNFA, CNFW, and CNFrD at 2 months compared to baseline (p = 0.025, 0.031, 0.009). The CNFW of fellow eyes at 2 months was also higher than that of the control group (p = 0.046). Similar to the changes in HZO-affected eyes, these differences were no longer present at 6 months in the fellow eyes. IVCM images of both eyes of an HZO patient together with images of an age and sex matched control are shown in Fig. 2.
HZO affected eye at baseline (1a), 2 months (1b) and 6 months (1c), HZO fellow eye at baseline (2a), 2 months (2b), and 6 months (2c), control (3). There is reduction in corneal nerve fibres (shown in red) and branching (shown in blue) from baseline (1a) to 2 months (1b) in the HZO affected eye, with partial recovery by 6 months (1c). This change is not apparent in the fellow eye (2a–c). The control eye shows normal nerve density and branching (3). IVCM in vivo confocal microscopy, HZO herpes zoster ophthalmicus.
Corneal sensitivity
The corneal sensitivities are presented in Table 3. There was no significant difference observed between HZO affected eyes or HZO fellow eyes, and control at all time points. There was also no longitudinal change across time amongst the HZO patients (p = 0.339–1.000).
Discussion
This is the first longitudinal study examining the acute, early and intermediate corneal nerve changes following HZO. This study identified that HZO eyes had significant reduction in CNBD at 2 months compared with baseline and control, and also a reduction in CNFD at 2 months compared with a normal eye. In addition, a subgroup of HZO eyes with either a positive Hutchinson’s sign or epithelial keratitis showed additional and significant reductions in CNFL and CTBD at 2 months, and CNFD at 6 months. In contrast, fellow eyes of HZO had an increase in CNFA, CNFW, and CNFrD from baseline to 2 months. No detectable change was observed in corneal sensitivities in any group.
Corneal denervation in HZO eyes
HZO affected eyes had a transient but significant reduction in CNBD and CNFD at 2 months, which later recovered by 6 months. This shows that the process of corneal denervation occurs within the first 2 months in HZO. The mechanism of corneal nerve degeneration in HZO has been postulated to be related to neuro-immune cross-talk as evidenced by a negative correlation between dendritiform cell density and size to corneal nerve parameters [11]. Herpes simplex virus and varicella zoster virus share similarities in disease mechanism and clinical presentation; IVCM studies in herpes simplex keratitis showed reduced corneal nerve parameters as early as days after disease onset [22], supporting our observation that nerve injury occurs early on in immune-mediated corneal nerve injury. Giannaccare et al. analysed the same seven IVCM parameters in ten fellow eyes of neurotrophic keratitis, and found reduced CNBD and CNFD while other parameters remained similar to control [23]. CNBD and CNFD are thus the two most sensitive parameters in detecting corneal denervation. Hamrah et al. has previously reported that patients with HZO showed significant reduction in total nerve length, total number of nerves, main nerve trunks, branching and corneal sensitivity [10]. However, the time since HZO onset was significantly longer in that study (at 5.1 ± 6.4 years), whereas our study focused on the first 6 months since onset. It is possible that corneal denervation continues to progress after 6 months. Furthermore, they only recruited HZO patients with corneal involvement, while our study included HZO with all manifestations and only 26.7% had corneal involvement.
In view of a possible link between corneal involvement and nerve changes, we conducted a subgroup analysis on HZO eyes with either Hutchinson’s sign or epithelial keratitis, which showed a reduction of additional IVCM parameters up to 6 months. The presence of Hutchinson’s sign implies the involvement of the nasociliary branch of the trigeminal nerve, and has been shown to be a risk factor of ocular inflammation and neurotrophic keratitis [24]. The nasociliary nerve provides sensory innervation for the cornea; hence its involvement may lead to a greater likelihood of denervation of the corneal subbasal plexus. Corneal sensory nerves interact closely with the corneal epithelium in order to maintain ocular surface homoeostasis and promote epithelial wound healing [25]; and a disruption to homoeostasis would lead to the development of neurotrophic keratitis [5]. It is possible that the presence of Hutchinson’s sign or epithelial keratitis could predict the development of corneal denervation. A retrospective review of HZO patients found that age, white ethnicity, BCVA at presentation, uveitis and disease recurrences were factors associated with neurotrophic keratitis [26]. Hutchinson’s sign was not included in their study. Corneal involvement at presentation was associated with neurotrophic keratitis on univariate but became insignificant after adjusting for age, sex, ethnicity, immunosuppression, diabetes, VA, intraocular pressure, uveitis, and recurrence; the authors attributed this to many patients developing corneal involvement only after initial presentation.
Corneal nerve regeneration in HZO eyes
In our study, the 2-month reduction in CNBD and CNFD in HZO eyes recovered by 6 months, suggesting that corneal nerve regeneration could occur as early as 6 months after the initial insult. The reinnervation process is induced by nerve damage, via upregulation of neurotrophins, immune regulatory factors, and nerve guidance factors such as SEMA 7A, which in turn leads to nerve growth and differentiation [27, 28]. Animal studies have shown that migrating Schwann cells, which play an important role in nerve regeneration, were observed 4 days after nerve injury, implying that the process of nerve regeneration begins soon after nerve damage occurs [29]. Corneal nerve regeneration after HZO has been scarcely reported. Cruzat et al. reported one case of corneal nerve regeneration and partial recovery of corneal sensation (from 0 to 25 mm) at 5 years after the onset of HZO [12]. Several studies have been conducted looking at skin biopsies of cutaneous zoster. Zografakis et al. has shown that there was an increase in subepidermal nerve fibre density in the affected dermatomes at 3 months post-zoster infection [30]. However, another study conducted by Petersen in a group of 57 zoster patients showed no recovery in cutaneous innervation by 6 months [31]. A longitudinal study on herpetic simplex virus keratitis eyes showed decreased corneal sensitivity and IVCM corneal nerve parameters at baseline (mean 50 days from onset of herpetic eye disease), followed by an increase 6 months later but not reaching parameters of contralateral eyes [27]. This also supports our observation of corneal nerve regeneration within 6 months of nerve damage.
Corneal nerve response in HZO fellow eyes
This is the first study that showed an early increase in corneal nerve parameters in fellow eyes of HZO. Hamrah et al. reported a significant reduction of corneal nerve in fellow eyes of HZO at 5 years, whilst the corneal sensitivity remained unaffected [10]. Skin biopsies in unilateral shingles has also shown damage to contralateral epidermal nerves [32]. This contralateral involvement is postulated to be mediated by the central nervous system, with primary afferent inputs projecting bilaterally via the spinal cord or brain circuits. There is also evidence that peripheral trigeminal nerve fibres directly project to bilateral areas of brainstem nuclei and the caudal medulla by crossing the pontine tegmentum [33]. Hence, unilateral nerve damage results in bilateral neuronal changes. However, this contralateral nerve damage was not observed in the first 6 months of HZO in our study. In contrast, we hypothesise that the increase in fellow eyes’ CNFA, CNFW, and CNFrD at 2 months could represent a compensatory or reparative process triggered by nerve growth factors in response to the damage in HZO eyes. The process of nerve fibre regeneration not only exhibits elongation of fibres, but also the widening of existing corneal nerves. CNFA, which is the total corneal nerve fibre area calculated from the total length and the nerve fibre width, was found to be a more sensitive measure to detect small changes in corneal nerve plexus [34]. Culver et al. also showed correlation between changes in CNFA with biomarker and functional indices after cibinetide (neurotrophic drug) administration, concluding that CNFA is a measure to assess disease modifying therapies for neuropathy [35].
Corneal sensitivity in HZO affected and fellow eyes
Despite the changes in IVCM parameters in both HZO affected and fellow eyes, the corneal sensitivities remained unchanged. The correlation between corneal nerve alteration and corneal sensitivity has been shown in previous studies [36, 37]. Benitez-Del-Castillo et al. showed a positive correlation between subbasal nerve density and mechanical, chemical, and thermal corneal sensitivities using a noncontact esthesiometer [36]. Zhivov et al. showed that impairment in subbasal nerve plexus structures was associated with reduced corneal sensitivity in a diabetic population [37]. Previous studies have shown that IVCM nerve parameters change is a more sensitive indicator of corneal denervation compared with corneal sensitivity [22], and hence the use of IVCM may be able to pick up early corneal nerve damage. In our study, we showed that milder degrees of corneal denervation may not be detectable by clinical examination alone. Therefore, IVCM is a more sensitive tool that plays a role in monitoring corneal nerve changes in these patients.
In this study, we have shown that HZO leads to early corneal denervation, especially in patients with Hutchinson’s sign and epithelial keratitis. Albeit no significant reduction in corneal sensitivity was detected clinically, we believe these patients should be monitored for neurotrophic keratitis particularly within the first few months of disease, preferably with the use of IVCM.
Despite the small sample size, our study carries a few merits. This is the first prospective longitudinal study that demonstrated significant corneal nerve changes in both eyes of HZO, by comparing with eyes in healthy age and sex matched controls. This is also the first IVCM study that evaluated the characteristics of corneal nerves during the acute, early to intermediate stages following HZO. Notwithstanding that IVCM is dependent on the experience of the operator, potential bias arising from inter-operator differences was mitigated by using one single operator and adopting a standardised and validated approach.
Limitations of this study include attrition bias as we encountered dropouts during the COVID-19 pandemic; as all subjects recovered soon after the acute illness, and none experienced a recurrence among those who completed the study, it was understandable that a few subjects would not return for follow up visits after obtaining initial treatment. Nonetheless, the small sample size limited the use of multi-variable regression analysis, hence we were not able to adjust for potential confounding effect of age and sex in corneal nerve parameters. Furthermore, the effect of age and sex in the association between HZO and corneal nerve changes could not be studied when both factors were matched in the recruitment of controls. Lastly, our study relies on the assumption that healthy eyes remain stable in corneal nerve characteristics and hence we only requested a single exam for controls. We believe this would be a better alternative to exposing these healthy subjects to increased risks as they attend to subsequent study visits during the pandemic. Finally, a study of larger scale and longer duration may give more information on nerve parameters other than density which was the primary outcome of the study. Together, this information will hopefully shed light on the timing of nerve degeneration and regeneration, as well as ascertain whether and when the fellow eye would display signs of corneal nerve impairment following HZO.
In summary, this study identified early corneal denervation in HZO eyes, together with corneal nerve proliferative response in fellow eyes. These changes were apparent on IVCM despite the absence of clinically detectable changes in corneal sensitivity. This illustrates the usefulness of IVCM in the understanding of the underlying pathophysiology behind not only HZO but also other forms of neurotrophic keratopathy. As an optical biopsy, IVCM provides a sensitive, objective and quantifiable method to monitor serial changes in corneal nerves. Our study has recognised potential corneal nerve parameters as a basis for future clinical studies on corneal nerve regeneration with nerve growth factor or other therapeutic modalities.
Summary
What was known before
-
Herpes zoster ophthalmicus leads to corneal denervation in both the affected eye and the fellow eye.
-
Corneal nerve regeneration after herpes zoster ophthalmicus has been demonstrated.
What this study adds
-
This is the first longitudinal in vivo confocal microscopy study analysing the early to intermediate changes in corneal nerve following herpes zoster ophthalmicus.
-
This study identified corneal nerve degeneration in affected eyes at 2 months, which later recovered by 6 months.
-
Corneal nerve proliferative response in fellow eyes was demonstrated at 2 months.
Data availability
All data generated during this study are included in this published article and its Supplementary files.
References
Yawn BP, Gilden D. The global epidemiology of herpes zoster. Neurology. 2013;81:928–30.
Rimland D, Moanna A. Increasing incidence of herpes zoster among Veterans. Clin Infect Dis. 2010;50:1000–5.
Bricout H, Haugh M, Olatunde O, Prieto RG. Herpes zoster-associated mortality in Europe: a systematic review. BMC Public Health. 2015;15:466.
Liesegang TJ. Herpes zoster ophthalmicus natural history, risk factors, clinical presentation, and morbidity. Ophthalmology. 2008;115:S3–12.
Sacchetti M, Lambiase A. Neurotrophic factors and corneal nerve regeneration. Neural Regen Res. 2017;12:1220–4.
Mok E, Kam KW, Aldave AJ, Young AL. Diagnosing paraproteinemic keratopathy: a case report. Case Rep Ophthalmol. 2021;12:337–43.
Siu GDJ, Kam KW, Young AL. Amniotic membrane transplant for bullous keratopathy: confocal microscopy & anterior segment optical coherence tomography. Semin Ophthalmol. 2019;34:163–7.
Ono T, Mori Y, Nejima R, Ogata M, Minami K, Miyata K. Sustainability of pain relief after corneal collagen cross-linking in eyes with bullous keratopathy. Asia Pac J Ophthalmol. 2018;7:291–5.
Patel DV, McGhee CN. Laser scanning in vivo confocal microscopy demonstrating significant alteration of human corneal nerves following herpes zoster ophthalmicus. Arch Neurol. 2010;67:640–1.
Hamrah P, Cruzat A, Dastjerdi MH, Prüss H, Zheng L, Shahatit BM, et al. Unilateral herpes zoster ophthalmicus results in bilateral corneal nerve alteration: an in vivo confocal microscopy study. Ophthalmology. 2013;120:40–7.
Cavalcanti BM, Cruzat A, Sahin A, Pavan-Langston D, Samayoa E, Hamrah P. In vivo confocal microscopy detects bilateral changes of corneal immune cells and nerves in unilateral herpes zoster ophthalmicus. Ocul Surf. 2018;16:101–11.
Cruzat A, Hamrah P, Cavalcanti BM, Zheng L, Colby K, Pavan-Langston D. Corneal reinnervation and sensation recovery in patients with herpes zoster ophthalmicus: an in vivo and ex vivo study of corneal nerves. Cornea. 2016;35:619–25.
Chen P, Piao X, Bonaldo P. Role of macrophages in Wallerian degeneration and axonal regeneration after peripheral nerve injury. Acta Neuropathol. 2015;130:605–18.
Linna TU, Pérez-Santonja JJ, Tervo KM, Sakla HF, Alió y Sanz JL, Tervo TM. Recovery of corneal nerve morphology following laser in situ keratomileusis. Exp Eye Res. 1998;66:755–63.
Latvala T, Barraquer-Coll C, Tervo K, Tervo T. Corneal wound healing and nerve morphology after excimer laser in situ keratomileusis in human eyes. J Refract Surg. 1996;12:677–83.
Kauffmann T, Bodanowitz S, Hesse L, Kroll P. Corneal reinnervation after photorefractive keratectomy and laser in situ keratomileusis: an in vivo study with a confocal videomicroscope. Ger J Ophthalmol. 1996;5:508–12.
Sen HN, Sangave AA, Goldstein DA, Suhler EB, Cunningham D, Vitale S, et al. A standardized grading system for scleritis. Ophthalmology. 2011;118:768–71.
Jabs DA, Nussenblatt RB, Rosenbaum JT. Standardization of Uveitis Nomenclature (SUN) Working Group. Standardization of uveitis nomenclature for reporting clinical data. Results of the First International Workshop. Am J Ophthalmol. 2005;140:509–16.
Zhao K, Yu H, Zheng X, Yang J, Wang X, Han Y, et al. Use of the inferior whorl for detecting age-related changes in human corneal subbasal nerve plexus with laser scanning confocal microscopy. Ophthalmic Res. 2021;64:769–74.
Takhar JS, Joye AS, Lopez SE, Marneris AG, Tsui E, Seitzman GD, et al. Validation of a novel confocal microscopy imaging protocol with assessment of reproducibility and comparison of nerve metrics in dry eye disease compared with controls. Cornea. 2021;40:603–12.
Petropoulos IN, Alam U, Fadavi H, Marshall A, Asghar O, Dabbah MA, et al. Rapid automated diagnosis of diabetic peripheral neuropathy with in vivo corneal confocal microscopy. Invest Ophthalmol Vis Sci. 2014;55:2071–8.
Hamrah P, Cruzat A, Dastjerdi MH, Zheng L, Shahatit BM, Bayhan HA, et al. Corneal sensation and subbasal nerve alterations in patients with herpes simplex keratitis: an in vivo confocal microscopy study. Ophthalmology. 2010;117:1930–6.
Giannaccare G, Pellegrini M, Taroni L, Bernabei F, Bolognesi F, Biglioli F, et al. Longitudinal morphometric analysis of sub-basal nerve plexus in contralateral eyes of patients with unilateral neurotrophic keratitis. Curr Eye Res. 2019;44:1047–53.
Zaal MJ, Völker-Dieben HJ, D’Amaro J. Prognostic value of Hutchinson’s sign in acute herpes zoster ophthalmicus. Graefes Arch Clin Exp Ophthalmol. 2003;241:187–91.
Eguchi H, Hiura A, Nakagawa H, Kusaka S, Shimomura Y. Corneal nerve fibre structure, its role in corneal function, and its changes in corneal diseases. Biomed Rest Int. 2017;2017:3242649.
Meyer JJ, Liu K, McGhee CNJ, Danesh-Meyer HV, Niederer RL. Neurotrophic keratopathy after herpes zoster ophthalmicus. Cornea. 2022;41:1433–6.
Danileviciene V, Zemaitiene R, Gintauskiene VM, Nedzelskiene I, Zaliuniene D. Corneal sub-basal nerve changes in patients with herpetic keratitis during acute phase and after 6 months. Medicina. 2019;55:214.
Chucair-Elliott AJ, Zheng M, Carr DJ. Degeneration and regeneration of corneal nerves in response to HSV-1 infection. Invest Ophthalmol Vis Sci. 2015;56:1097–107.
Chen B, Chen Q, Parkinson DB, Dun XP. Analysis of Schwann cell migration and axon regeneration following nerve injury in the sciatic nerve bridge. Front Mol Neurosci. 2019;12:308.
Zografakis C, Tiniakos DG, Palaiologou M, Kouloukoussa M, Kittas C, Staurianeas N. Increased density of cutaneous nerve fibres in the affected dermatomes after herpes zoster therapy. Acta Derm Venereol. 2014;94:168–72.
Petersen KL, Rice FL, Farhadi M, Reda H, Rowbotham MC. Natural history of cutaneous innervation following herpes zoster. Pain. 2010;150:75–82.
Oaklander AL, Romans K, Horasek S, Stocks A, Hauer P, Meyer RA. Unilateral postherpetic neuralgia is associated with bilateral sensory neuron damage. Ann Neurol. 1998;44:789–95.
Jacquin MF, Chiaia NL, Rhoades RW. Trigeminal projections to contralateral dorsal horn: central extent, peripheral origins, and plasticity. Somatosens Mot Res. 1990;7:153–83.
Brines M, Culver DA, Ferdousi M, Tannemaat MR, van Velzen M, Dahan A, et al. Corneal nerve fiber size adds utility to the diagnosis and assessment of therapeutic response in patients with small fiber neuropathy. Sci Rep. 2018;8:4734.
Culver DA, Dahan A, Bajorunas D, Jeziorska M, van Velzen M, Aarts LPHJ, et al. Cibinetide improves corneal nerve fiber abundance in patients with sarcoidosis-associated small nerve fiber loss and neuropathic pain. Invest Ophthalmol Vis Sci. 2017;58:BIO52–60.
Benitez-Del-Castillo JM, Acosta MC, Waffi MA, Diaz-Valle D, Gegundez JA, Fernandez C, et al. Relation between corneal innervation with confocal microscopy and corneal sensitivity with noncontact esthesiometry in patients with dry eye. Invest Ophthalmol Vis Sci. 2007;48:173–81.
Patel DV, Ku JY, Johnson R, McGhee CN. Laser scanning in vivo confocal microscopy and quantitative aesthesiometry reveal decreased corneal innervation and sensation in keratoconus. Eye. 2009;23:586–92.
Author information
Authors and Affiliations
Contributions
EM contributed to study design, patient recruitment, data acquisition and interpretation, and drafting of manuscript. KWK contributed to study design, data interpretation, and manuscript revision. ALY contributed to manuscript revision. All authors approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mok, E., Kam, K.W. & Young, A.L. Corneal nerve changes in herpes zoster ophthalmicus: a prospective longitudinal in vivo confocal microscopy study. Eye 37, 3033–3040 (2023). https://doi.org/10.1038/s41433-023-02469-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-023-02469-0