Abstract
Objectives
Analyse trends in incidence and aetiologies of childhood blindness (CHB) in Israel during 2014–2020, with comparison to the previous decade.
Methods
Descriptive, retrospective population-based trend study using Poisson regression. Data retrieved from the Israeli National Registry of the Blind included demographics, registration-years, and aetiologies. Primary and secondary outcomes were incidence of new certified blindness cases and its comparison with the previous decade, respectively.
Results
In total, 4.19 new CHB certificates per 100,000 were issued in Israel during 2014–2020, with a slight non-significant increase (p = 0.31). Males and younger children had higher incidence rates (p = 0.0008 and p = 0.0002, respectively). Leading causes were optic nerve anomalies (ONA), retinal dystrophies (RDYS), other retinal disorders (ORD) and cerebral visual impairment (CVI) (16.9%, 15.1%, 12.4% and 10.5%, respectively). Compared with the previous decade: ONA rates remained unchanged (p = 0.13) as did some other main aetiologies (i.e., albinism, CVI and nystagmus), while rates of RDYS and ORD increased (by 21.9%, p = 0.001 and 9.9% p = 0.02, respectively). Rates of retinopathy of prematurity (ROP), glaucoma, cataract and amblyopia remained very low (weighted average of 0.15, 0.14, 0.09 and 0.03 per 100,000, respectively).
Conclusions
The incidence of CHB certifications in Israel remained stable with a slight increase, stemming chiefly from RDYS resurgence and an increase in ORD. Main causes remained ONA and RDYS. The most common avoidable cause, ROP, remained scarce, maintaining the reduction seen in the earlier decade, as did cataract, glaucoma, and amblyopia. This may support future nationwide prevention policies to decrease the incidence of RDYS and ORD.
Similar content being viewed by others
Introduction
There are ~1.5 million blind children in the world, and an estimated 500,000 children go blind each year (one per minute) [1]. Regional differences in the prevalence and causes of paediatric blindness are believed to be based on both genetic and socioeconomic factors; current prevention and treatment schemes for genetic diseases are limited, while the latter might limit proper access to medical treatment [1,2,3,4].
Addressing paediatric blindness is of high priority due to its detrimental effects on children’s development, education, and future employment. These effects have been proved destructive to the quality of life for both the afflicted children and their families [5, 6]. Moreover, the global financial cost of childhood blindness (CHB), in terms of loss of earning capacity (per capita GNP), is greater than the cost of adult blindness and has recently been estimated at $6–27 billion [7], while the preventable causes have been shown to be as high as 80% of the total global burden [3].
Recognising trends over time of various aetiologies can aid the elucidation of correlations between CHB and healthcare and prevention policies as well as promoting advancements in medical care.
The purpose of this study was to document current trends in the annual incidence of common aetiologies of CHB in Israel, and compare them to those of previous years [4].
Materials and methods
The study and data collection conformed to all local laws and adhered to the principles of the Declaration of Helsinki. Approval was obtained from the Institutional Review Board of the Rambam Health Care Campus, Haifa, Israel (RMB-D-0217-21). This study included children 0–18 years of age who were deemed eligible according to the definition of blindness in Israel, after having completed the process of blindness certification provided by The Service for the Blind, Deaf and Assistive Technology, under the Ministry of Welfare and Social Affairs. (MOWSA) A further division of age-groups was made, with the terms “younger- and older-children” referring to children aged 0–5 years old and 6–18 years old, respectively.
Data collection
Israel has maintained a nationwide registry of blindness (NRB) certificates since 1987; this system was computerised in 2012. We conducted a descriptive, retrospective population-based trend study and analysed the incidence of paediatric blindness certificates issued between 2014 and 2020. The various available aetiologies for blindness in the application form for certification are listed in previous publications [4, 8]. Information on the size of the population (age ≤ 18 years) during the study period was obtained from the publicly available database of the Israel Central Bureau of Statistics [9].
Screening process
There are three routine state-mandatory ophthalmological assessments at the ages of 1–2, 3–4, and 5–6 years old. In addition, irrespective of age, children can be referred by a consultant community or hospital affiliated ophthalmologist, and parents can also apply directly to MOWSA”. Regardless of the pathway, every blindness certificate is only issued after a state-appointed consultant ophthalmologist examination is performed.
Blindness definition
Blindness in Israel corresponds to the WHO criteria [1], and is defined as either a visual acuity at distance for an aged-matched standardised optotype such as LEA numbers or symbols of less than 3/60 in the better-seeing eye, or a visual field with a radius no greater than 10° around central fixation in the better-seeing eye with the best possible optical correction. For very young or non-verbal children, qualitative assessments were used as appropriate.
Blindness certification process
Children are referred for evaluation after having failed the visual acuity screening test or if they are afflicted with a medical condition that causes severe visual impairment (Supplementary Table 1). Further details regarding this structured process have been previously described [4, 8].
Ocular examination
Complete eye examination included age-appropriate, best-corrected visual acuity assessment, a thorough ophthalmological examination, and visual field testing where applicable. Additional aspects have been previously specified [4, 8].
Blindness aetiology diagnosis
The formal diagnosis was made by a senior ophthalmology consultant appointed by The Service for the Blind, Deaf and Assistive Technology. Any diagnosis made by a referring ophthalmologist was confirmed by the consultant. The results of the visual acuity and visual field assessments for each eye, as well as the major and minor causes for visual impairment, were recorded on the application form that contains a list of 31 possible causes [4, 8]. Details of the remainder of this structured process have been previously published [4, 8]. The structured classification in the application form did not discern Retinitis pigmentosa coding from different types of retinal dystrophies (RDYS), including cone dystrophies, cone-rod dystrophy, and rod-cone dystrophies. This was also the case for different optic nerve anomalies (ONA), such as optic atrophy and optic nerve hypoplasia. Therefore, we have used these terms throughout the paper. In the case of co-existing multiple disorders, that main cause for blindness was chosen at the discretion of the state-appointed ophthalmologist.
Temporary certificates
Temporary certificates were only issued to preverbal children or those with a developmental delay, who could not be examined to produce a quantitative outcome measure such as visual acuity or computerised perimetry to assess visual field defects, yet the nature of their medical disorder (e.g., albinism, ONA etc.) have supported the eligibility for a temporary blindness certification, until they reach an age in which an examination could provide reliable measurable results.
Statistical analysis
All analyses were performed using R (R Core Team (2021). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. https://www.R-project.org/). Annual rates of all-cause, sex-specific, and disease-specific blindness were calculated. Poisson regression models were used to assess time-trends of all-cause, age, sex, and disease-specific rates of blindness. To compute the standard error for the rate ratios, we used the delta method. A two-tailed p value <0.05 was considered statistically significant.
Results
A total of 895 CHB certificates were issued between 2014 and 2020 (507 male; 213 temporary certificates). There were no differences in age (p = 0.42, χ2 = 6.03) or sex (p = 0.74, χ2 = 3.51) distribution over the years.
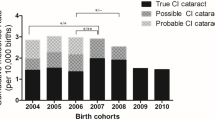
The incidence of newly certified blindness in children per 100,000 residents increased slightly from 3.87 in 2014 to 4.13 in 2020; this change was non-significant (p = 0.31) (Table 1 and Fig. 1).
The average was 4.19, and the yearly rate increase using Poisson was 4.6% (p < 0.001, 95% CI: 2.2–7.0%). To rule out an impact of temporary certificates on the annual trend (Supplementary Tables 2 and 3), we calculated the annual change without temporary certificates and observed that the increase over time remained significant (average 2.7%, 95% CI: 0.3–5.1%). Males had significantly higher blindness incidence rates than females (p = 0.0008, RR: 1.24; 95% CI: 1.08–1.43), and younger children had significantly higher blindness incidence rates than older children (p = 0.0002, RR: 1.23; 95% CI: 1.11–1.33). There was no significant difference in the rate of increase between males and females after adjustment for age group (p = 0.33, χ2 = 0.94) nor a difference in the rate of increase between younger and older children (p = 0.35, χ2 = 0.84) after adjustment for sex.
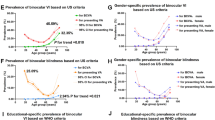
ONA and RDYS were the leading causes of CHB certifications in Israel (Table 2). This trend was maintained throughout the study period with respect to the crude rate of new certificates of blindness issued between 2014 and 2020 (Fig. 2).
There was a significant increase in the annual blindness certification incidence attributed to RDYS (p < 0.001, 14.3%; 95% CI: 7.6–21.5%) and other retinal disorders (p < 0.001, 11.7%; 95% CI: 5.1–18.7%) during this period (Table 3); the rates of blindness certifications attributed to ONA, CVI, nystagmus and albinism did not change. The rates of other causes, including ROP, cataract, and glaucoma, among others, were very low.
Comparison with the previous decade
The leading attributed causes of blindness among children remained ONA and RDYS. The blindness incidence rate attributed to ONA from 2014 to 2017 was not significantly different from that of 2013 (0.40; 95% CI: 0.17–0.64); the last 3 years (2018–2020) exhibited an increased rate which was similar to the rate observed during 2003–2008. Overall, ONA rates did not significantly change from the previous decade (p = 0.13).
In contrast to the previous decade, the annual rate of RDYS issued certificates increased (p = 0.0002, +14.3%; 95% CI: +7.6–21.5%), rather than decreased (p = 0.008, −7.1%; 95% CI: −11.2 to −3.0%). However, the blindness certification incidence rate of RDYS from 2014 to 2016 was not significantly different from that of 2013 (p = 0.37, incidence rate = 0.40; 95% CI: 0.17–0.64), and the rates observed from 2017 to 2020 returned to those of the beginning of the previous decade. Overall, the annual change in blindness incidence rate was 21.9% higher than in the previous decade (p < 0.001; 95% CI: 12.4–32.2%). The annual certification rate of other retinal disorders increased between 2014 and 2020 by 9.9% over the previous decade (p = 0.02, 95% CI: 1.9–18.6%), with a significant increase over 2013 (incidence rate = 0.33; 95% CI: 0.11–0.55) during the years 2016–2017 (p = 0.05) and 2019–2020 (p = 0.03).
We found no significant change in the annual certification rates of albinism, CVI or nystagmus. The rate of albinism exhibited a non-significant decline (p = 0.42, −2.8%; 95% CI: −9.4 to +4.2%) which was not significantly different from the decline of the previous decade (p = 0.41, −7.6%, 95% CI: −14.3 to −0.9%). There were very few annual cases of ROP, glaucoma, amblyopia, and cataract (median 2003–2013 vs. 2014–2020: 7 vs. 4, 4 vs. 5, 3 vs. 4, and 5 vs. 2, respectively); thus, trend analysis was unreliable.
Discussion
Reliable data regarding CHB, particularly in high-income countries, are sparse [10]. This study aimed to investigate trends in paediatric blindness incidence in Israel between 2014 and 2020 and compare them with those of the same population during the previous decade (2003–2013) to identify what has changed.
The incidence of CHB certifications in Israel showed a non-significant increase (p = 0.31), in accordance with a recent study from the UK which reported unchanged incidence of severe visual impairment/blindness (SVI/BL) certifications between 2000 and 2015 [11]. The pandemic might have affected these results, given the annual increase until the year 2020. There are some possible explanations such as increasing social awareness of the benefits of certifications, an increase in ophthalmologists’ availability nationwide, or a change in policy brought about by better cooperation between government agencies. On the other hand, this could also be an artificial increase due to an unusual high number of certifications issued in 2019, due a technical delay in the processing of applications prior to 2019, which is our current assumption. Due to the small number of cases, this should be examined in a few years’ time to allow to collect long-term trends and differentiate between short-term fluctuations, and the effects of the pandemic [12, 13].
Our findings also show higher blindness certification incidence rates in boys compared to girls. These findings are consistent with a greater decline in girls as opposed to boys in the previous decade in the same population [4], yet inconsistent with studies in other parts of the world [14, 15]. Another possible explanation for this gap could be the result of under-certification of girls, previously reported by Israeli investigators in other care areas [16, 17].
Moreover, and as expected due to congenital cases, higher blindness certification incidence rates were evident in the younger 0–5 years age group of, as opposed to the older 6–18 age group. This has been reported previously; for example, a recent British study reported that incidence rates are the highest at infancy [11, 15]. the rate of increase in the incidence rates over the years, however, was similar across similar across all ages.
Similarly, to the same population in previous years [4], ONA and RDYS were the leading causes of CHB certifications in Israel. These were followed by, in descending order, other retinal disorders, CVI, nystagmus, albinism, ROP, glaucoma, amblyopia and cataract. To date, CVI and optic nerve anomalies remain the most common causes of SVI/ BL in high-income countries [2, 11, 13, 18,19,20]. In addition, in line with other studies, we found ROP, cataract and amblyopia and glaucoma to be the most common treatable causes [11, 13, 19, 20].
ONA showed stable blindness certification incidence rates over the study period; these rates roughly corresponded with those observed in previous years. The blindness certification incidence rates of RDYS in the same population increased during the study period in contrast to a decreasing trend in the previous decade. However, the rates observed at the end of the study period only approached the baseline rates observed at the beginning of the previous decade. The decrease in consanguineous marriage in Israel and higher availability of genetic counselling did not seem to truly affect the rates of RDYS as the previous study has suggested, and it seems important to reassess prevention policies in at-risk populations to facilitate and encourage genetic counselling and testing to yet again decrease these resurging, inherited congenital causes of CHB, including RDYS and other retinal disorders [4, 21].
We observed a non-significant decline and plateauing in the average annual blindness certification incidence of ROP, mimicking a similar drop in the previous decade [4]. Improved protocols, such as implementation of the G-ROP study as well increased use of intra-vitreal injections of anti VEGF agents, such a Bevacizumab (Avastin®; Genentech, Inc., South San Francisco, CA, USA), a once off-label indication that was recently officially added to the third revision of the joint statement of the American Academy of Paediatrics and Ophthalmology to treat ROP, May underlie this trend. Another possible explanation could be improved care of pre-term infants [22, 23].
Glaucoma, cataract, and amblyopia remained very low, displaying a plateauing of their annual certification rates, in concordance with findings in other high-income countries [14, 15, 20]. This supports that the medical care of these treatable conditions remains effective to date. The annual certification rates of CVI, nystagmus and albinism, however, showed an erratic pattern. A longer follow-up may reveal the trends of these aetiologies.
This study has several limitations, the first of which is its retrospective nature, thus key information that is not routinely collected could have provided further insight into other risk factors and comorbidities that were missing from the present NRB dataset. Secondly, underreporting to the registry can affect the reliability of the data; however, we believe that the good primary health care system and high availability of ophthalmological examinations with free access to the application for blindness certification in Israel, and the economic and social incentives for blindness certification, have led most caregivers to apply. Thirdly, the examination methods were not included in the application form and only one disorder is coded as the main cause for visual impairment in the better-seeing eye. Another limitation could be the unknown effects of the Covid-19 pandemic. However, both the applications for blindness certification as well as ophthalmological consultations have remained in effect throughout the pandemic; the substantial medical and financial incentives stayed significant, and we have witnessed a steady number of applications before and after the pandemic. Therefore, we believe our results were not substantially affected. Further elaboration of retinal diseases on the application form may shed light on obscure causes of blindness that we were unable to analyse. We recommend that MOWSA officials update the application form to differentiate retinal dystrophy types and optic nerve pathologies, as well as include ethnicity data, in order to promote future NRB based research. The trends of some causes of blindness, such as RDYS or ROP, may require a longer time period for interpretation, as low rates or an erratic incidence pattern might hamper our ability to reach a definite conclusion about the trends of these aetiologies. Lastly, data regarding the specific pathways undertaken by each applicant were not available. This may have had an impact on the validity of our findings. Despite this, all pathways were available for every subject, and final, formal examinations and diagnoses were performed and determined by a MOWSA appointed consultant ophthalmologist, all of which may have helped to minimise this possible effect.
To conclude, the blindness certifications issued for children in Israel remained rather stable, with a slight non-significant increase, attributed mostly to RDYS and other retinal disorders. The most common aetiologies remain ONA and RDYS. Certifications attributable to preventable causes of blindness in Israel have decreased over the years, plateauing at a low annual rate. The rate of ROP remained low after the improvement seen in the earlier decade. Further collaborative nationwide studies of common mutations, particularly of RDYS and other inherited, congenital retinal disorders, as well as increasing availability of genetic counselling, may reduce the incidence of these important causes of blindness [24,25,26].
Summary
What was known before
-
In previous years (1999–2013), a substantial decline in childhood blindness was witnessed in Israel, and was attributed to a reduction in retinal dystrophies.
-
A recent study from the UK showed stable childhood blindness certification rates between 2000 and 2015.
What this study adds
-
The certification incidence of childhood blindness has remained stable in recent years, with a slight non-significant rise mainly due to retinal dystrophies and other retinal disorders, in contrast to the decline observed in previous years.
-
These findings may support the efforts to improve nationwide prevention policies, aiming to improve public awareness, and increase pre-natal genetic counselling and testing to decrease the incidence of congenital RDYS and other retinal disorders.
-
It may also indicate a need for allocating additional resources to research and development of genetic therapeutics.
Data availability
Data will be provided with investigator support, after approval of a proposal, with a signed data access agreement.
References
World Health Organization. Global initiative for the elimination of avoidable blindness: action plan 2006-11. World Health Organization; 2007. https://apps.who.int/iris/handle/10665/43754.
Steinkuller PG, Du L, Gilbert C, Foster A, Collins ML, Coats DK. Childhood blindness. J AAPOS. 1999;3:26–32.
Pascolini D, Mariotti SP. Global estimates of visual impairment: 2010. Br J Ophthalmol. 2012;96:614–8.
Mezer E, Chetrit A, Kalter-Leibovici O, Kinori M, Ben-Zion I, Wygnanski-Jaffe T. Trends in the incidence and causes of severe visual impairment and blindness in children from Israel. J AAPOS. 2015;19:260–5.e1.
Rahi JS, Gilbert CE, Foster A, Minassian D. Measuring the burden of childhood blindness. Br J Ophthalmol. 1999;83:387–8.
Bhattacharjee H, Das K, Borah RR, Guha K, Gogate P, Purukayastha S, et al. Causes of childhood blindness in the northeastern states of India. Indian J Ophthalmol. 2008;56:495–9.
Smith AF, Smith JG. The economic burden of global blindness: a price too high! Br J Ophthalmol. 1996;80:276–7.
Israeli A, Peer H, Gleitman I, Falick Y, Mezer E. Time trends of etiologies of blindness in Israel 2009-2020: have methods to decrease leading causes of blindness been exhausted? Am J Ophthalmol. 2022;240:149–58.
Anon. Population in localities. 2022. https://www.cbs.gov.il/en/subjects/Pages/Population-in-Localities.aspx.
GBD 2019 Blindness and Vision Impairment Collaborators, Vision Loss Expert Group of the Global Burden of Disease Study. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: the right to sight: an analysis for the Global Burden of Disease Study. Lancet Glob Health. 2021;9:e144–60.
Teoh LJ, Solebo AL, Rahi JS. British Childhood Visual Impairment and Blindness Study Interest Group. Temporal trends in the epidemiology of childhood severe visual impairment and blindness in the UK. Br J Ophthalmol. 2021:bjophthalmol-2021-320119.
Mitry D, Bunce C, Wormald R, Leamon S, Simkiss P, Cumberland P, et al. Causes of certifications for severe sight impairment (blind) and sight impairment (partial sight) in children in England and Wales. Br J Ophthalmol. 2013;97:1431–6.
Solebo AL, Teoh L, Rahi J. Epidemiology of blindness in children. Arch Dis Child. 2017;102:853–7.
de Verdier K, Ulla E, Löfgren S, Fernell E. Children with blindness—major causes, developmental outcomes and implications for habilitation and educational support: a two-decade, Swedish population-based study. Acta Ophthalmol. 2018;96:295–300.
Krumpaszky HG, Lüdtke R, Mickler A, Klauss V, Selbmann HK. Blindness incidence in Germany. A population-based study from Württemberg-Hohenzollern. Ophthalmologica. 1999;213:176–82.
Calderon-Margalit R, Paltiel O. Women’s health in Israel. Lancet. 2018;391:538–9.
Israeli A, Gal D, Younis A, Ehrenberg S, Rozner E, Turgeman Y, et al. Sex-differences in atrial fibrillation patients: bias or proper management? Vasc Health Risk Manag. 2022;18:347–58.
Kong L, Fry M, Al-Samarraie M, Gilbert C, Steinkuller PG. An update on progress and the changing epidemiology of causes of childhood blindness worldwide. J AAPOS. 2012;16:501–7.
Blohmé J, Bengtsson-Stigmar E, Tornqvist K. Visually impaired Swedish children. Longitudinal comparisons 1980-1999. Acta Ophthalmol Scand. 2000;78:416–20.
Chong C, McGhee CNJ, Dai SH. Causes of childhood low vision and blindness in New Zealand. Clin Exp Ophthalmol. 2019;47:165–70.
Sharkia R, Mahajnah M, Athamny E, Khatib M, Sheikh-Muhammad A, Zalan A. Changes in marriage patterns among the Arab community in Israel over a 60-year period. J Biosoc Sci. 2016;48:283–7.
Chiang MF, Quinn GE, Fielder AR, Ostmo SR, Paul Chan RV, Berrocal A, et al. International classification of retinopathy of prematurity, third edition. Ophthalmology. 2021;128:e51–68.
Fierson WM, American Academy of Pediatrics Section on Ophthalmology, American Academy of Ophthalmology, American Association for Pediatric Ophthalmology and Strabismus, American Association of Certified Orthoptists. Screening examination of premature infants for retinopathy of prematurity. Pediatrics. 2018;142:e20183061.
Cideciyan AV. Leber congenital amaurosis due to RPE65 mutations and its treatment with gene therapy. Prog Retin Eye Res. 2010;29:398–427.
Yahalom C, Kimchi A, Macarov M, Shemesh E, Rosenmann A, Blumenfeld A. Albinism in Israel: clinical and genetic characteristics. Investigative Ophthalmol Vis Sci. 2018;59:1831.
Sharon D, Ben-Yosef T, Goldenberg-Cohen N, Pras E, Gradstein L, Soudry S, et al. A nationwide genetic analysis of inherited retinal diseases in Israel as assessed by the Israeli inherited retinal disease consortium (IIRDC). Hum Mutat. 2020;41:140–9.
Author information
Authors and Affiliations
Contributions
AI designed the study, coordinated and supervised the data collection, statistical analysis, and wrote the manuscript as well the revision. He also conducted all the steps of the submission process. IG and HP designed the data collection instruments, collected the data, verified the validity of the data, and carried out the initial statistical analysis. They have also contributed their insight on the process of certification. YF contributed his insight on the relevant procedures and methods of the Service for the Blind, Deaf and Assistive Technology, and changes in policies. This allowed in turn to better address the results and analysed what could have affected the trends. He then reviewed and revised the manuscript. EM conceptualised the study, coordinated, and supervised data collection, and critically reviewed the manuscript for important intellectual content. He also oversaw modified and approved all the steps of submission and revision. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Israeli, A., Peer, H., Gleitman, I. et al. Childhood blindness incidence and aetiologies trends in Israel 2014–2020: what should we focus on?. Eye 37, 2559–2564 (2023). https://doi.org/10.1038/s41433-022-02374-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02374-y
This article is cited by
-
Dissecting the complex sex-based associations of myopia with height and weight
Eye (2024)
-
The role of parental health beliefs in seeking an eye examination for their child
BMC Ophthalmology (2023)
-
Characteristics and differences of strabismus surgeries performed in private versus public settings: a national multicenter study
International Ophthalmology (2023)