Abstract
Background
To assess the main causes leading to childhood visual impairment/blindness in a center for low vision in Israel and to analyze the literature on pediatric blinding diseases in developed countries.
Methods
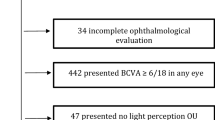
Retrospective study based on observational case series. Data were obtained from medical records of visually impaired children, seen at a national referral low vision center. Children were divided into two groups: moderate visual impairment (6/18 to 6/60) and severe visual impairment (SVI)/blindness (<6/60). Inherited eye diseases (IED) were grouped together for analysis. Data from the Israeli blind registry from the same period of time were analyzed for comparison. A review of literature on childhood blindness in developed countries since 2000 was conducted.
Results
A total of 1393 children aged 0–18 years were included in the study. Moderate visual impairment was seen in 1025 (73.6%) and SVI/blindness in 368 (26.4%) of the studied children. Among blind children, IED accounted for at least 51% of all diagnoses, including mainly albinism and retinal dystrophies. IED prevalence was equally high in both main ethnic groups (Jewish and Arab Muslims). Non-IED (22.6%) included mainly patients with cerebral visual impairment and retinopathy of prematurity.
Conclusions
The leading cause of childhood visual impairment and blindness in our patient cohort was IED. Analyses of the literature from the last two decades show that IED are a major cause for SVI/childhood blindness in other developed countries as well. Updated patterns of global childhood blindness may suggest a need for new approach for screening programs and modern tactics for prevention.
Similar content being viewed by others
Introduction
Childhood blindness causes a significant economic burden on the family and community because blind and visually impaired children have a lifetime of blindness ahead of them [1]. Globally, nutritional and infectious causes of blindness in children have declined substantially in developing countries, although these persist in some focal settings [2]. In the least developed countries, congenital and developmental cataract, retinal dystrophies, and congenital anomalies are gaining prominence as causes of blindness in children [3]. For children in developed countries, cerebral visual impairment (CVI) and optic nerve anomalies are classically described among the most common causes of blindness [4]. Inherited eye diseases (IED) are known to be common, accounting for 14% of all childhood blindness cases in African countries and up to 53% of cases in developed countries such as Europe and the United States [1, 3,4,5,6], but there is not enough emphasis on how prevalent they have become during the last decade.
The World Health Organization (WHO) defines blindness as a best corrected visual acuity (BCVA) worse than 3/60. Visual impairment is divided into mild (6/12–6–18), moderate (worse than 6/18), and severe (SVI) worse than 6/60. Israel has a nationwide blindness registry since 1987 [7]. The definition of blindness used in Israel is slightly less rigid (3/60 and worse). Patients are identified by ophthalmologists and are registered if they have legal blindness. The standard registration form has a list of some of the most common diseases causing blindness but not all of them are enumerated, so an important number of pathologies are not mentioned on the list and, instead, are grouped as “others.” CVI was added to the list in 2009, but other common diseases such as Best disease, Stargardt disease, congenital stationary night blindness, achromatopsia, aniridia, and others are still not included separately [8].
Our study presents an analysis of the main causes for visual impairment and blindness in children, based on the database of a national referral center for low vision. Our center has a team composed of optometrists, ophthalmologists, social workers, and genetic counselors and offers a multidisciplinary approach for patients diagnosed with visual impairment or blindness. The team provides a comprehensive approach including diagnosis, visual rehabilitation and visual aids training, access to social services, complementary “special teachers” for children at school and governmental benefits, genetic tests, treatment, and prevention options. Children are referred to our center (unique of its kind in Israel) from ophthalmologists from all over the country in order to reach the comprehensive low-vision assistance given by our team. The cost of the visit to our center is covered by the Israeli ministry of welfare.
Materials and methods
We conducted a retrospective study with review of medical records of children aged 0–18 years, referred to the Michaelson Institute for low vision, at Hadassah-Hebrew University Medical Center in Jerusalem, from January 2015 to December 2019.
Approval for this study, according to the Helsinki tenets, was obtained from the Institutional Review Board at Hadassah-Hebrew University Medical Center, Jerusalem.
Inclusion criteria included children with visual impairment defined as BCVA of 6/18 or less (better eye), or children with unknown exact visual acuity who had a diagnosis known to severely affect vision or visual field (for example, early onset retinitis pigmentosa, achromatopsia). Details extracted from children’s medical files included: age, ethnic origin (when available), gender, ocular diagnosis, inheritance, BCVA, and associated diseases. Genetic counseling and testing were routinely offered to patients with suspected IED.
Data from the Israeli blind registry from the same period of time were analyzed for comparison, and a review of the literature on childhood blindness from the last decade was conducted.
Diseases causing visual impairment/blindness were divided into two main groups: IED and non-IED, in order to study the incidence of IED as a cause of visual impairment in children. Visual acuity was assessed for distance using a computerized monitor with linear Lea symbols for young children and numerical linear optotypes for older children. The data were divided into two main groups according to BCVA patients: “moderate visual impairment” with BCVA from 6/18–6/60 and “SVI/blindness” (BCVA < 6/60) or a visual field worse than 20° in cooperative children.
Statistical analysis was performed using the Mann–Whitney U test (nonparametric test), Pearson and chi-square tests.
Results
A total of 1393 patients were included in the study; 58.1% male and 41.9% female. Mean age was 8.1 years (+/−5.1), median 8 (range 0.6–18). Mean visual acuity was logMAR 0.7 (+/−0.3), median 0.7 (range 0.2–2.3). Verbal visual acuity was possible to assess in 1312/1393 studied children (Lea symbols for distance); 81 (5.8%) children were not cooperative for quantitative visual acuity tests.
Associated non-ophthalmic disorders were present in 159 patients (11.4%). The most common systemic associations were cerebral palsy and Usher syndrome.
Ethnic origin showed a majority of Jewish patients (67.8%) followed by Arab Muslims (26.9%) and others, mainly Druze and Christian Arabs (5.2%). There was a statistically significant correlation between the most common eye diseases and ethnicity; among Jewish, albinism was the most common disease (48.4%) and among Arab Muslims, inherited retinal diseases (IRD) were the most common (50.6%) (P: <0.001) (Table 1).
IED included: albinism, IRD [retinitis pigmentosa (RP), achromatopsia, cone-rod dystrophies, congenital stationary night blindness, Stargardt disease, Best disease], Aniridia and patients with confirmed inherited optic atrophy (OA), retinoblastoma, and congenital cataract. IED as a group was the cause of visual impairment/blindness (vision 6/18 or less) in 1078/1393 (77.4%) of children in our study (Table 2).
Non-IED included mainly CVI, retinopathy of prematurity (ROP), myopic maculopathy, congenital glaucoma and some of the patients with OA (secondary to nongenetic diseases as hydrocephalus), and congenital cataract with no genetic background identified. There were six children diagnosed with congenital glaucoma; none of the families had a familial history of glaucoma and they disagreed to perform genetic testing so they were left out of the IED group.
Moderate visual impairment was found in 1025 patients (73.6%); the most prevalent disorders in this group were albinism, IRD, and nystagmus (Table 2). IED accounted for at least 77.7% of all diagnoses in this group.
SVI/blindness was present in 368 (26.4%) of studied children. The most common ocular pathologies were IRD followed by albinism and CVI; at least 51% of ocular pathology in this group was due to IED (Table 2). According to the WHO definition of blindness, a lower number of children belonged to the <3/60 group (Table 1).
The ocular pathologies that accounted for the poorest mean visual acuity included CVI and IRD, mainly Leber’s congenital amaurosis.
Data collected from a review of the literature on childhood visual impairment and blindness in developed countries were summarized in Table 3.
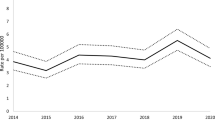
Data provided by the Israeli national registry for the blind were analyzed for comparison during the same time period (2015–2019); main causes leading to childhood blindness were OA and RP (both of them 16%), “other retinal pathology” (15%) and CVI (10%) (Table 4). Main causes for childhood blindness in children aged 0–5 years were retinal disease (IRD other than RP), OA, and CVI. In children aged 6–18 years, the main causes were RP, IRD, and OA.
Discussion
Hereby, we present an analysis of the main causes for visual impairment and blindness in children, based on the database of a national referral center for low vision located in a tertiary hospital in Jerusalem. We aimed for this data (and not for the national registry of blind) to include children not only with blindness but also with visual impairment, to evaluate the correlation with ethnicity and to be able to analyze all diagnoses independently.
Two main retinal pathologies were among the most common causes and include two relatively large areas of childhood visual problems (retinal dystrophies and albinism) accounting for the substantial numbers in accordance to the literature [9]. Albinism was among the most common causes for visual impairment (BCVA 6/18 to 6/60), followed by retinal dystrophies. The most common ocular pathologies leading to blindness (BCVA < 6/60) were IRD, albinism, and CVI, in decreasing order. Interestingly, there was a statistically significant correlation between the most common eye diseases and ethnicity; albinism was the most common disease among Jews and IRD was the most common among Arab Muslims.
A previous publication based on the Israeli registry for blindness published in 2015, referred a decreasing rate of childhood blindness in Israel, raising the possibility that the cause was a lower incidence of IED over the years of the study [8]. Interestingly, if we group RP (13%), albinism (4%), and “other retinal pathologies” (11%) taken from their table, we reach 28% which makes IED the main cause of blindness [8]. Analysis of recent data (2015–2019) from the same Israeli registry for the blind, shows that when grouping the same diagnoses as above, (RP, other retinal pathology (all IRD other than RP) and albinism) IED reaches 37% of childhood blindness causes, showing a rising percentage of IED as a cause of childhood blindness in Israel. Furthermore, IED prevalence reaches 43% if we take similar data from 2019 alone (Table 4). As previously discussed, other IED are not included separately in the blind registry’s list (such as aniridia, or diseases that might be genetic such as OA, congenital cataract/glaucoma) and cannot be documented, reducing the real number of IED. Also details regarding pathology origin (genetic or not), as in OA, congenital cataracts, and glaucoma are not provided, reducing further the total estimation for IED prevalence. Stratification of data from the national registry in two age groups showed as expected, that CVI was most prevalent in the 0–5 age group compared with the 6–18 age group. IED were the most common cause of blindness in both age groups.
CVI incidence reached only 10.7% of causes. One possible explanation for the relative low percentage of CVI might be that the diagnosing ophthalmologists documented this cause of blindness as OA, causing an apparently lower incidence of CVI and higher incidence of OA as an etiology for childhood blindness. In our center, CVI percentage reached 22% as a cause of blindness, which is relatively close to the published percentage in England in 2010 [9].
We can also appreciate that we have seen through our center, around half the number of children that got a blind certificate through the Israeli blind registry, during the same period of time, making our cohort representative.
Rates of blindness secondary to ROP are falling in the developed world because of the success of screening and treatment protocols. ROP is now becoming an avoidable cause of blindness in middle-income countries owing to improvements in perinatal medicine [10].
Several authors have reported that CVI is the leading cause of SVI/ blindness in children in the developed world [9, 11, 12]. In 2010, Durnian published that CVI was the most common cause (27%) for visual loss in children in England. However, when grouping “genetic causes” of vision impairment from Durnian’s publication, retinal dystrophies, aniridia, albinism, and the “hereditary” OA (2.3% of all OA described in the article) together reach a higher percentage (29.2%) of blindness than that caused by CVI (27%) (Table 3). Furthermore, in the latter publication, if we take into consideration that among other common causes of childhood blindness like congenital cataract (3.5%), congenital nystagmus (2.3%) and congenital glaucoma (1.2%) many are inherited, the number of IED might be even higher. We may say that also in England, IED as a group is the leading cause of childhood blindness. Similarly, in a publication by de Verdier in 2018, IED “grouped together” reach a higher number (17.3%) compared to CVI (8%) in Sweden [13].
In 2016, Bosch et al. published interesting data regarding the genetic basis of CVI [14]. They found that 5 of 25 children with CVI (20%) who were investigated by whole-exome sequencing, had variants in four genes known to be associated with CVI (AHDC1, NGLY1, NR2F1, PGAP1) establishing a conclusive genetic diagnosis for CVI. This knowledge shows us the importance of monogenetic disorders in the pathogenesis of CVI, so far mainly investigated as an “acquired brain damage”, highlighting the necessity to test for genetic defects using genome-wide diagnostic tools. Furthermore, if a certain percentage of CVI has genetic grounds, it might further increase the number of IED in developed countries.
Rudanko reported in 2004, that the main cause for visual impairment in 431 full-term children born in Finland were “genetic eye diseases” reaching 53%, emphasizing the lack of treatment for these genetic eye disorders over two decades covered by the study [15]. Kong et al. reported in 2012 that hereditary eye diseases accounted for 44% of blindness in childhood in Europe based on literature searches [16]. Boonstra et al. reported in their 2012 study that during the last two decades in the Netherlands, untreatable disorders such as genetic eye diseases and CVI have become the major causes for children’s blindness as a result of increased survival of preterm children and improved diagnostic possibilities [17].
One of the major difficulties in comparing incidence of blindness between published studies in the literature is that different criteria for defining and grouping visual impairment and blindness are used. Many studies group SVI and blindness together, others include even moderate visual impairment and yet others use a more strict criteria for blindness [9, 11, 13]. When considering strictly the definition of blindness by the WHO (<3/60) in our 2019 patients, the percentage of blindness was higher in the Arab Muslims and others ethnic groups compared to Jewish.
Possible biases in our study include the fact that this was a retrospective study and that it was based on a single multidisciplinary tertiary low vision center database, and not on a national registry. However, analysis of our data compared to the Israeli national registry for the blind leads to similar conclusions. Another limitation in our study is the lack of consistent information regarding ethnic origin in all the studied years as well as the fact that we cannot differentiate Muslims Arabs from Israel, from those from the Palestinian Authority, limiting the information regarding the possible higher rate of IED due to frequent consanguineous marriages in the Palestinian Authority.
We believe that reporting only the primary ocular diagnoses to describe the leading causes of blindness can be misleading. When “IED” are analyzed as a major group, it can allow priorities to be determined and appropriate strategies to be delineated in order to adapt the system toward prevention of childhood blindness.
In conclusion, IED as a group is a major cause for childhood visual impairment and blindness in Israel as well as in other developed countries of the world. Despite many advances in our understanding of IED, treatment options remain limited with the best hopes for treatment lying in the use of gene therapy, growth promotion therapies for degenerative diseases, and possibly the grafting of retinal cells. However, improved methods for identifying disease-causing mutations together with genetic counseling, genetic testing, and prenatal and/or preimplantation genetic diagnosis provide a feasible approach for preventing the recurrence of these blinding diseases in the same family [18]. Awareness among physicians regarding the possibility of prevention of these severe blinding diseases is of crucial importance. Changing patterns of global childhood blindness calls for a need for reassessment of research, screening programs, prioritization of examinations, and tactics for prevention.
Summary
What was known before
-
Analysis of isolated causes of childhood blindness in developed world during the last two decades points toward CVI as the main cause in many countries.
What this study adds
-
Main causes leading to childhood blindness are changing.
-
Grouping IED together shows that genetic eye diseases are far more common than previously reported and represent the main cause for childhood blindness in developed countries.
-
Reassessment of screening and prevention tactics might be needed.
References
Frick KD, Foster A. The magnitude and cost of global blindness: an increasing problem that can be alleviated. Am J Ophthalmol. 2003;135:471–6.
Kalua K, Patel D. Causes of blindness among children identified through village key informants in Malawi. Can J Opthalmol. 2008;43:425–7.
Gogate P, Kalua K, Courtright P. Blindness in childhood in developing countries: time for a reassessment? PLoS Med. 2009;6:e1000177. https://doi.org/10.1371/journal.pmed.1000177.
Solebo AL, Rahi J, Teoh L. Epidemiology of blindness in children. Arch Dis Child. 2017;102:853–7.
World Health Organization. Programme for the Prevention of Blindness and Deafness. Global initiative for the elimination of avoidable blindness. World Health Organization. 2000. https://apps.who.int/iris/handle/10665/63748.
Khan RI, O’Keefe M, Kenny D, Nolan L. Changing pattern of childhood blindness. Ir Med J. 2007;100:458–61.
Farber MD. National Registry for the Blind in Israel: estimation of prevalence and incidence rates and causes of blindness. Ophthalmic Epidemiol. 2003;10:267–77. https://doi.org/10.1076/opep.10.4.267.15910.
Mezer E, Chetrit A, Kalter-Leibovici O, Kinori M, Ben-Zion I, Wygnanski-Jaffe T. Trends in the incidence and causes of severe visual impairment and blindness in children from Israel. J Am Assoc Pediatr Ophthalmol Strabismus. 2015;19:260–265.e1. https://doi.org/10.1016/j.jaapos.2015.04.002.
Durnian JM, Cheeseman R, Kumar A, Raja V, Newman W, Chandna A. Childhood sight impairment: a 10-year picture. Eye. 2010;24:112–7. https://doi.org/10.1038/eye.2009.32.
Gilbert C, Rahi J, Eckstein M, O’Sullivan J, Foster A. Retinopathy of prematurity in middle-income countries. Lancet. 1997;350:12–4. https://doi.org/10.1016/S0140-6736(97)01107-0.
Rahi JS, Cable N, British Childhood Visual Impairment Study Group. Severe visual impairment and blindness in children in the UK. Lancet. 2003:1359–465.
Rosenberg T, Flage T, Hansen E, Riise R, Rudanko SL, Viggosson G, et al. Incidence of registered visual impairment in the Nordic child population. Br J Ophthalmol. 1996;80:49–53. https://doi.org/10.1136/bjo.80.1.49.
de Verdier K, Ulla E, Löfgren S, Fernell E. Children with blindness—major causes, developmental outcomes and implications for habilitation and educational support: a two-decade, Swedish population-based study. Acta Ophthalmol. 2018;96:295–300. https://doi.org/10.1111/aos.13631.
Bosch DG, Boonstra FN, de Leeuw N, Pfundt R, Nillesen WM, de Ligt J, et al. Novel genetic causes for cerebral visual impairment. Eur J Hum Genet. 2016;24:660–5. https://doi.org/10.1038/ejhg.2015.186.
Rudanko SLLL. Visual impairment in children born at full term from 1972 through 1989 in Finland. Opthalmology. 2004;111:2307–12.
Kong L, Fry M, Al-Samarraie M, Gilbert C, Steinkuller PG. An update on progress and the changing epidemiology of causes of childhood blindness worldwide. J Am Assoc Pediatr Ophthalmol Strabismus. 2012;16:501–7. https://doi.org/10.1016/j.jaapos.2012.09.004.
Boonstra N, Limburg H, Tijmes N, van Genderen M, Schuil J, van Nispen R. Changes in causes of low vision between 1988 and 2009 in a Dutch population of children. Acta Ophthalmol. 2012;90:277–86. https://doi.org/10.1111/j.1755-3768.2011.02205.x.
Yahalom C, Macarov M, Lazer-Derbeko G, Altarescu G, Imbar T, Hyman JH, et al. Preimplantation genetic diagnosis as a strategy to prevent having a child born with an heritable eye disease. Ophthalmic Genet. 2018. https://doi.org/10.1080/13816810.2018.1474368.
Acknowledgements
The authors thank the Israeli National Registry for the Blind and the Ministry of Welfare in Israel for providing access to the national data on childhood blindness.
Author information
Authors and Affiliations
Contributions
CY was responsible for designing the research protocol, analysis and interpretation of data, writing and revising the manuscript. RB, RP, and IS were responsible for collecting and analyzing the data, searching for references, and revising the manuscript. MM and AB were involved in data acquisition, analysis, interpretation and drafting the manuscript. KH was responsible for analysis and interpretation of data, writing and revising the manuscript. All of the authors gave final approval of this version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yahalom, C., Braun, R., Patal, R. et al. Childhood visual impairment and blindness: 5-year data from a tertiary low vision center in Israel. Eye 36, 2052–2056 (2022). https://doi.org/10.1038/s41433-021-01743-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01743-3
This article is cited by
-
Visual conservation treatment dilemmas in neuroblastoma with bilateral blindness
Discover Oncology (2024)