Abstract
Background
To report the rate of primary periocular BCC recurrence following surgical excision in low-risk and high-risk BCCs, and to propose long term follow up guidelines.
Methods
Retrospective case series of primary BCC treated with surgical excision (Mohs micrographic surgery [MMS], wide local excision [WLE] or fast paraffin excision) who have histologically-confirmed BCC subtype and histologically-measured tumour clearance margins.
Results
77 patients (78 eyelids) were included. Mean age was 72.0 ± 12.8 years with a female predominance (42, 54.5%). Most common histological BCC subtype was nodular (39, 50.0%). 44 (56.47.1%) patients underwent MMS. Tumour clearance was achieved in 59 (75.6%) eyelids after one surgery. 9 had further surgery to achieve tumour clearance while 10 were monitored. There was no statistical significance between recurrence rates in patients who had tumour clearance compared with patients with incomplete tumour clearance after initial surgery (p = 0.15). In patients with incomplete tumour clearance, there was no statistical significance between recurrence rates in those who underwent further surgery versus those monitored (p = 0.47). Average follow-up duration was 37.9 ± 17.2 months. Three (3.9%) cases had recurrent BCC. All three cases had high-risk BCC features (infiltrative subtypes and/or incomplete tumour excision after initial surgery).
Conclusions
There was no evidence of recurrence of completely excised, low-risk BCCs at three years, regardless of type of surgical excision. We recommend patients with completely excised, primary BCCs without high-risk features be monitored for one year. Patients with any high-risk BCC features, such as incompletely excised tumours or high-risk histological subtypes, should be monitored for five years.
Similar content being viewed by others
Introduction
Primary basal cell carcinoma (BCC) is the most common form of periocular malignancy. The Royal College of Pathologists has published guidelines since 2003 regarding the minimum histological dataset that should be reported for primary cutaneous BCCs [1]. In the UK, the standard surgical options are excision with a predefined safety surgical margin of resection (e.g., WLE) or excision with tissue margin control (e.g., frozen section, fast paraffin or MMS).
Follow up of excised BCC can constitute a large workload in oculoplastic clinics. We report the rate of primary periocular BCC recurrence following surgical excision in low-risk and high-risk BCCs in a real-world clinical setting, and propose safe long term follow up guidelines accordingly.
Methods
In this retrospective case series, all medical records of patients presenting with periocular BCCs between January 2011 and November 2013 at Moorfields Eye Hospital were screened for study entry. For study inclusion, all patients were required to have: primary BCC treated with surgical excision; known histologically-confirmed subtype; reported tumour clearance margins; and were followed up for a minimum of 12 months following surgery for low-risk BCC, or minimum of 36 months following surgery for high-risk BCC.
Patients who underwent non-surgical treatment (e.g., radiotherapy), or had recurrent BCC initially diagnosed and treated elsewhere (two patients), were excluded from the study, as patients with these risk factors would be followed up long term.
Data collected included: patient demographics; location of lesion; surgical excision details; histological subtype; outcome including histologically-measured tumour clearance, further treatment, recurrence rate and follow up duration. All research was conducted in accordance with the Declaration of Helsinki. The protocol was approved by the Moorfields Eye Hospital with a waiver of consent granted (CA20/AD/656).
Low-risk versus high-risk BCC [2]
Low-risk BCC were classified according to tumour factors (low-risk histological subtype [nodular, superficial]; complete tumour clearance; no perineural or lymphovascular invasion; not involving the medial canthus), and patient factors (no genetic predisposition, no active or history of long-term immunosuppression).
High-risk BCC was classified according to tumour factors (high-risk histological subtype [infiltrative, micronodular], basosquamous differentiation, positive tumour at surgical margin or narrow tumour clearance margin of <1 mm, level of invasion beyond subcutaneous fat, thickness >6 mm, presence of perineural invasion and/or lymphovascular involvement; medial canthus site), and patient factors (genetic predisposition e.g. Gorlin syndrome, active immunosuppression).
Selection for surgery
Patients presenting with a suspected BCC were discussed at the local skin cancer multidisciplinary team meeting after an incisional biopsy confirmed the diagnosis.
At our institution, patients with BCCs undergo surgical excision in the form of fast paraffin excision or wide local excision (WLE) with minimum 3 mm surgical margins, or they undergo Mohs micrographic surgery (MMS) in an affiliated institution with subsequent reconstruction at Moorfields Eye Hospital.
The decision between WLE or fast paraffin excision was made on surgeon preference. Frozen section excisions are not carried out at our institution.
MMS technique
This is covered in detail elsewhere [3, 4]. In brief, the tumour is debulked, and 1–2 mm area around the debulked margin of the tumour is excised. A map of the excision site is drawn, the excised tissue is divided into pieces, and their position drawn on the map and marked with sutures. The tumour undergoes histological examination, further layers are excised if tumour cells are identified, and the process is continued until no further tumour is seen in the excised tissue.
WLE technique
Lesions were excised with a 3 mm margin from the clinical edge of the lesion and the defect was reconstructed as a one-stage procedure.
Fast paraffin excision
Lesions were excised with a 3 mm margin from the clinical edge of the lesion. The specimen was subjected to rapid turnaround (<48 h), and further excision with paraffin examination was performed if the margins were involved until a clear margin was obtained. Reconstruction was performed once the margins were clear.
Tumour clearance
Complete tumour clearance was defined as 1 mm or more histological clearance of both deep and peripheral tumour margins. Patients who were found to have <1 mm tumour clearance after initial excision were classified for the purposes of our study as having incomplete tumour clearance, and were offered further surgery or were monitored. This decision was made on an individual case-by-case basis after further discussion at our local skin cancer multidisciplinary team meeting. Factors involved in the decision-making process include age, location of tumour, histological subtype, any evidence of tumour aggressiveness (e.g. lymphatic or perineural invasion), and patient’s wishes.
Statistical analyses
Continuous variables are reported as mean ± standard deviation. Categorical data are reported as frequency and percentage of the study population unless otherwise specified. A Fisher exact test or Chi-squared test were used when comparing categorical variables. The independent t-test was used for continuous variables. The 2-tailed significance threshold was set at P < 0.05.
Statistical analyses were conducted using IBM SPSS version 26.0 (IBM Corp. Armonk, N.Y, USA).
Results
77 patients (78 eyes) met criteria and were included in this study
Demographics and clinical presentation
Most patients were women (42, 53.8%). The mean patient age was 72.0 ± 12.8 years (range: 29–90 years). 40 (51.3%) had right eyelid BCC. The majority had lower eyelid BCC (51, 65.4%), while 11 (14.1%) had BCC in the medial canthus. Seven patients had a history of previous BCCs elsewhere on the face or body. Two patients were undergoing active immunosuppression treatment (one for breast cancer and spinal metastasis, one for idiopathic thrombocytopenic purpura). None of the patients had genetic predisposition for BCC.
Surgical excision details
45 (57.7%) cases underwent MMS, 22 (28.2%) had WLE, and 11 (14.1%) underwent fast paraffin excision for initial surgical excision.
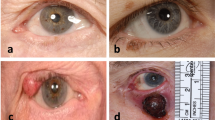
Histological subtype
All cases were primary periocular BCC. There were 39 (50.0%) nodular BCCs, 16 (20.5%) infiltrative, 3 (3.8%) nodulocystic, and 20 (25.7%) mixed subtypes.
Two cases had nodular BCC with squamous component. They had complete tumour clearance following surgical excision, and were not associated with any recurrences at 24 and 48 months, respectively.
There were no cases of perineural or lymphovascular invasion, level of invasion beyond subcutaneous fat, or tumours with thickness >6 mm.
Outcome
Tumour clearance was achieved in 58 (74.4%) cases after one surgery (44 cases had MMS, 8 cases had WLE and 6 cases had fast paraffin), and a further 9 (11.7%) achieving tumour clearance after second surgery. The median follow up duration for this subgroup was 36 ± 18.1 months. There was one recurrence in this subgroup (see below).
Of the 19 cases with incomplete tumour clearance after initial surgery, the median tumour margin clearance was 0.2 ± 0.3 mm. 16 (84.2%) had nodular BCC, 1 had infiltrative BCC, 1 had nodulocystic BCC, and 1 had mixed infiltrative and superficial BCC. 15 (78.9%) had lower eyelid lesions. 14 (73.7%) cases had WLE as first line surgery, 5 (26.3%) had fast paraffin excision and none had MMS.
Of these 19 cases, 9 had further surgery to achieve tumour clearance, which included WLE in seven cases and MMS in two cases. Tumour clearance was achieved after the second operation in these nine cases. The median follow up duration for this subgroup was 36 ± 10.7 months. There were no recurrences in this subgroup.
In contrast, of these 19 cases, 10 did not have further surgery to achieve tumour clearance and were monitored instead. The median follow up duration for this subgroup was 36 ± 14.4 months. There were two recurrences in this subgroup (see below).
There was no statistical significance between recurrence rates in patients who had tumour clearance compared with patients with incomplete tumour clearance after initial surgery (p = 0.15). In patients with incomplete tumour clearance, there was no statistical significance between recurrence rates in those who underwent further surgery versus those who were monitored (p = 0.47).
The characteristics and outcomes of subgroups requiring further surgery due to incomplete tumour clearance after initial surgery are outlined in Table 1.
Recurrences
The average follow up duration for all patients was 37.9 ± 17.2 months. Three (3.8%) cases had recurrent BCC. Two occurred in infiltrative or mixed infiltrative BCC subtypes, and one occurred in a case with nodular BCC. Recurrence occurred in one each following MMS (2.3%), WLE (4.5%) and fast paraffin excision (9.1%).
A 77 year old male had left lower eyelid infiltrative BCC which was excised with MMS which achieved tumour clearance. The tumour recurred after 12 months and was excised via WLE with clear margins. The patient has not had further recurrence at final follow up 24 months after the second procedure.
A 75 year old male with a past medical history of mesothelioma treated with radiotherapy, presented with right lower eyelid nodular BCC which was excised with fast paraffin. The patient had narrow tumour clearance but did not have any further excisions as he elected to monitor the lesion. During monitoring he received high-dose steroid therapy for immune thrombocytopenic purpura. His tumour recurred at 60 months. This was an incidental finding following a surgical repair of late development of cicatricial ectropion by wedge excision without any clinical evidence of recurrence. The recurrence was managed with MMS. This patient did not have further recurrence 12 months after the second procedure, and subsequently passed away from an unrelated medical condition.
A 70 year old female with a previous history of BCCs elsewhere had left lateral canthal mixed infiltrative and superficial BCC which was excised with WLE. The patient had narrow tumour clearance but did not have any further excisions as she elected to monitor the lesion. Her tumour recurred at 36 months and was managed with MMS. This patient has not had further recurrence at final follow up 18 months after the second procedure.
There was no statistical significance between tumour type and recurrence rate (p = 0.20) or type of initial surgery and recurrence rate (p = 0.50).
The characteristics and outcomes of patients with recurrences are outlined in Table 2.
Discussion
The management of periocular BCCs aims for complete tumour resection confirmed by histopathological analysis. Our results showed an overall recurrence rate of 3.8%, Two occurred in infiltrative or mixed infiltrative BCC subtypes, and one occurred in a patient with nodular BCC. Recurrence occurred in one each following MMS (2.3%) after 12 months, WLE (4.5%) after 36 months and fast paraffin excision (9.1%) after 36 months. All patients with recurrence had at least one of two high-risk BCC features: infiltrative subtype and/or incomplete tumour clearance after initial surgery.
Surgery provides the most effective treatment for BCCs and remains the gold standard [5]. Recurrence rates following surgical excision are reported between 0 and 9.5%, although there is variation in the literature depending on histological subtype, surgical excision type and follow up duration [6,7,8,9,10]. Our results showed an overall recurrence rate of 3.8%, which is comparable with figures previously published.
Although there was no significant difference in recurrence rates between our patients with incomplete excision who had further surgery against those who were observed, we would recommend re-excision as the most appropriate course when tumour clearance has not been achieved, especially when high-risk tumour subtypes are reported, in line with previous studies [9, 11].
In our case series, tumour clearance was achieved in 74.4% after one surgery, with a further 11.7% achieving tumour clearance after second surgery. Incomplete tumour clearance is known to increase the risk of recurrence, with recurrence rates ranging from 0.39 to 3.96% with complete excision, and up to 50% with incomplete excision [6,7,8, 12,13,14]. This was seen in two of our three recurrences, which occurred in patients with incomplete tumour clearance who did not undergo further surgical excision. McGrath et al reported that, in BCCs with involved margins on initial excision, 18.6% had residual tumour while 78.2% had no residual tumour on histological examination of further excised tissue [15]. They found that risk factors for specimens with residual tumour include micronodular (54.1%) and nodular (23.7%) subtypes, and lower eyelid location (72.1%) [15]. In Ho et al, 8.7% of tumours needed more than one excision for complete clearance, which increased to 20.5% for infiltrative subtypes [9]. In our study, 84.2% of patients with incomplete tumour clearance after initial surgery had nodular subtype and 78.9% had lower eyelid lesions. These studies and our results further strengthen the notion that patients with incomplete tumour clearance at first excision should be advised to have further surgical excision.
MMS remains the gold standard for tumour clearance and preserving healthy tissue. The technique involves examining frozen section areas of tissues to ensure negative surgical margins, while allowing for maximal tissue preservation [3, 4]. MMS offers the lowest recurrence risk of BCC [10, 12], with rates reported around 1.5–5.8% [10, 16,17,18], higher in recurrent BCCs (6.5–20%) compared with primary BCC (0–1.6%) at 5 years [12, 17], with a mean time to recurrence of 39 months [17]. We had one case of infiltrative BCC recurrence post-MMS (2.3%) that occurred at 12 months. However, we recognise that MMS can be costly, time-consuming, and may not be available across all institutions.
Safe margins for WLE are debated across clinicians. Several studies have reported on the range of surgical excision margins to obtain clear margins around the eyelids and elsewhere in the body [6, 19,20,21,22]. Periocular BCCs are typically excised with 3–4 mm margins, however this may not adequately lead to complete tumour excision in up to 17–54% [23, 24]. In Hamada et al, non-infiltrative BCC excision with 4 mm margins gave a zero recurrence rate [24]. Gulleth et al found that a 3 mm margin can be safely used for non-infiltrative BCC 2 cm or smaller, obtaining a 95% cure rate [7]. Additionally, a clinician’s choice for WLE margin may also be influenced by a combination of other factors such as BCC subtype, tumour size, tumours with clinically poorly defined margins, or recurrence [23]. We routinely perform WLE with 3 mm margins to aim for complete excision of the tumour, which in our study was associated with one case (4.5%) of mixed infiltrative and superficial BCC recurrence that occurred at 36 months.
There is variation across institutions on how long patients are reviewed following surgical excision of BCCs. Five years of clinical follow-up for periocular BCC, a high-risk site, is recommended to ensure early detection of recurrence [9]. Ho et al had previously published their data in support of discharging patients with completely excised solid or nodular BCC after 6 months, and reviewing patients with infiltrative of recurrent BCC for 5 years [9]. In our case series, there were no evidence of recurrence of nodular BCCs with low-risk characteristics at three years. Our three patients with recurrences all had high-risk factors: two with infiltrative or mixed infiltrative subtype, and one with narrow clearance margin after initial surgery who did not have further surgery. Our study therefore supports similar recommendations of discharging patients with completely excised, primary BCCs without high-risk features at one year.
There are a few limitations to consider. Firstly, is regarding the relatively small number of cases included which represents the main limitation of our study, we acknowledge that small numbers can influence the statical analysis. Secondly, we recognise that we have a high rate of MMS at our institution, which may not be an accessible service for all units. We have attempted to minimise the treatment bias by analysing our MMS patients separately from our fast paraffin and WLE patients. Thirdly, patients from earlier in the series were more likely to have incomplete histological dataset reports including those regarding tumour clearance rates. We have attempted to overcome this limitation by only including patients where measured tumour clearance margins were reviewed and reported, which reduced the sample size included in this study. We would recommend that the standardised histological dataset is used where possible when reporting on the histological features of periocular BCCs [1].
In conclusion, there was no evidence of recurrence of completely excised, primary low-risk BCCs at three years, regardless of type of surgical excision. On the basis of these results, we recommend patients with completely excised, primary low-risk BCCs without high-risk features conclude their surveillance time earlier as recommended by [9] Ho et al. however on periocular tumour excision it is prudent to follow up patients until the scar maturates, which is usually achieved at one year post-operative [25], based on the knowledge that scarring can induce cicatricial lid malposition. Patients with histologically narrow clearance margins, recurrent, or high-risk histological subtypes, should be monitored for five years. All patients should be advised to monitor for new lesions and to seek referral if any suspicious lumps are identified.
Summary
What was known before
-
Primary basal cell carcinoma (BCC) is the most common form of periocular malignancy.
-
BCCs are classified into low-risk or high-risk subtypes depending on tumour and patient factors.
-
Follow up of excised BCC can constitute a large workload in oculoplastics clinics.
What this study adds
-
There was no evidence of recurrence of completely excised, low-risk BCCs at three years, regardless of type of surgical excision.
-
We recommend patients with completely excised, primary BCCs without high-risk features be monitored for one year.
-
Patients with any high-risk BCC features, such as incompletely excised tumours or high-risk histological subtypes, should be monitored for five years.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Slater DBP Dataset for histopathological reporting of primary cutaneous basal cell carcinoma. Royal College of Pathologists. 2019 [Available from: https://www.rcpath.org/uploads/assets/53688094-791e-4aaa-82cec42c3cb65e35/Dataset-for-histopathological-reporting-of-primary-cutaneous-basal-cell-carcinoma.pdf.
Crowson AN. Basal cell carcinoma: Biology, morphology and clinical implications. Mod Pathol 2006;19:S127–47.
Morris DS, Elzaridi E, Clarke L, Dickinson AJ, Lawrence CM. Periocular basal cell carcinoma: 5-year outcome following Slow Mohs surgery with formalin-fixed paraffin-embedded sections and delayed closure. Br J Ophthalmol. 2009;93:474–6.
der Plessis PJ, Dahl MG, Malcolm AJ, Sviland L, Dickinson AJ, Lawrence CM. Mohs’ surgery of periocular basal cell carcinoma using formalin-fixed sections and delayed closure. Br J Dermatol. 1998;138:1003–8.
Bath-Hextall FJ, Perkins W, Bong J, Williams HC. Interventions for basal cell carcinoma of the skin. Cochrane Database Syst Rev. 2007:CD003412.
Poignet B, Gardrat S, Dendale R, Lemaitre S, Lumbroso-Le Rouic L, Desjardins L, et al. Basal cell carcinomas of the eyelid: Results of an initial surgical management. J Fr Ophtalmol. 2019;42:1094–9.
Gulleth Y, Goldberg N, Silverman RP, Gastman BR. What is the best surgical margin for a Basal cell carcinoma: a meta-analysis of the literature. Plast Reconstr Surg. 2010;126:1222–31.
Smeets NW, Krekels GA, Ostertag JU, Essers BA, Dirksen CD, Nieman FH, et al. Surgical excision vs Mohs’ micrographic surgery for basal-cell carcinoma of the face: randomised controlled trial. Lancet 2004;364:1766–72.
Ho SF, Brown L, Bamford M, Sampath R, Burns J. 5 years review of periocular basal cell carcinoma and proposed follow-up protocol. Eye (Lond). 2013;27:78–83.
Wong VA, Marshall JA, Whitehead KJ, Williamson RM, Sullivan TJ. Management of periocular basal cell carcinoma with modified en face frozen section controlled excision. Ophthalmic Plast Reconstr Surg. 2002;18:430–5.
guidelines NCCNN. Basal cell skin cancer 2022 [Available from: https://www.nccn.org/professionals/physician_gls/pdf/nmsc.pdf.
Malhotra R, Huilgol SC, Huynh NT, Selva D. The Australian Mohs database, part II: periocular basal cell carcinoma outcome at 5-year follow-up. Ophthalmology 2004;111:631–6.
Mohs FE. Micrographic surgery for the microscopically controlled excision of eyelid cancers. Arch Ophthalmol. 1986;104:901–9.
Glatt HJ, Olson JJ, Putterman AM. Conventional frozen sections in periocular basal-cell carcinoma: a review of 236 cases. Ophthalmic Surg. 1992;23:6–8. discussion 9
McGrath LA, Meeney A, Currie ZI, Mudhar HS, Tan JH. Staged excision of primary periocular basal cell carcinoma: Absence of residual tumour in re-excised specimens: a 10-year series. Br J Ophthalmol. 2019;103:976–9.
Weesie F, Naus NC, Vasilic D, Hollestein LM, van den Bos RR, Wakkee M. Recurrence of periocular basal cell carcinoma and squamous cell carcinoma after Mohs micrographic surgery: A retrospective cohort study. Br J Dermatol. 2019;180:1176–82.
Litwin AS, Rytina E, Ha T, René C, Woodruff SA. Management of periocular basal cell carcinoma by Mohs micrographic surgery. J Dermatol Treat. 2013;24:232–4.
Pieh S, Kuchar A, Novak P, Kunstfeld R, Nagel G, Steinkogler FJ. Long-term results after surgical basal cell carcinoma excision in the eyelid region. Br J Ophthalmol. 1999;83:85–8.
Peden R, Radwan M, Wright M. Small margin (up to 2 mm) excision of periocular basal cell carcinomas in the setting of a one-stop clinic - long-term outcomes at a minimum of 11 years’ follow-up. Eye (Lond). 2020;34:2036–40.
Ito T, Inatomi Y, Nagae K, Nakano-Nakamura M, Nakahara T, Furue M, et al. Narrow-margin excision is a safe, reliable treatment for well-defined, primary pigmented basal cell carcinoma: an analysis of 288 lesions in Japan. J Eur Acad Dermatol Venereol. 2015;29:1828–31.
Babaye-Nazhad S, Amirnia M, Alikhah H, Khodaeyani E, Atapour N. Safety margin in excision of basal cell carcinoma. Pak J Biol Sci. 2009;12:1408–14.
Ünverdi Ö, Yücel S, Berk OS. Recommended surgical margins for basal cell carcinoma: Is 3 mm safe enough? Adv Ski Wound Care. 2020;33:209–12.
Almousa R. Predictors for margin of resection >4 mm in the management of periocular basal cell carcinoma. Korean J Ophthalmol. 2021;35:391–6.
Hamada S, Kersey T, Thaller VT. Eyelid basal cell carcinoma: Non-Mohs excision, repair, and outcome. Br J Ophthalmol. 2005;89:992–4.
Sorg H, Tilkorn DJ, Hager S, Hauser J, Mirastschijski U. Skin wound healing: An update on the current knowledge and concepts. Eur Surg Res. 2017;58:81–94.
Author information
Authors and Affiliations
Contributions
VJ contributed towards data gathering and analysis. VJ also drafted and revised the article towards final approval. PS and OV contributed towards data gathering and analysis, and revising/approving the final article. CS and FM contributed towards planning the paper, data gathering and analysis, and revising/approving the final article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Juniat, V., Shah, P., Vonica, O. et al. Periocular basal cell carcinoma recurrence following surgical treatment: Safe surveillance time. Eye 37, 971–976 (2023). https://doi.org/10.1038/s41433-022-02133-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02133-z
This article is cited by
-
Long-term results after surgical basal cell carcinoma excision in the eyelid region: revisited
Wiener klinische Wochenschrift (2024)
-
Recurrence rates of periocular basal cell carcinoma following intra-operative en-face frozen section margin controlled excision
Irish Journal of Medical Science (1971 -) (2024)