Abstract
Purpose
To assess prevalence and associated factors of parapapillary gamma zone enlargement (GZE).
Methods
Using fundus photographs and optical coherence tomographic images of participants of the population-based Beijing Eye Study, we examined gamma zone changes in a 10-year follow-up.
Results
The study included 89 highly myopic eyes (61 participants; age: 65.0 ± 9.8 years) and 86 randomly selected non-highly myopic eyes. GZE prevalence was significantly higher in highly myopic eyes than non-highly myopic eyes (75/89; 84%; 95% CI: 77, 92 versus 18/86; 21%; 95% CI:12, 30; p < 0.001). None of the eyes showed a reduction in gamma zone size. Higher prevalence of segmental GZE without enlargement of Bruch’s membrane opening (BMO) (mean: 26/175; 14.9%; 95% CI: 9.5, 20.2) was associated with optic disc size reduction (OR: 43.3; 95% CI: 10.9, 172; p < 0.001), disc-fovea distance elongation (OR: 15.4; 95% CI: 3.12, 76.4; p = 0.001) and lower prevalence of high axial myopia (OR: 0.08; 95% CI: 0.01, 0.44; p = 0.001). Higher prevalence of circular GZE (mean: 38/175; 21.7%; 95% CI: 16, 28) was correlated with optic disc enlargement (OR: 4.30; 95% CI: 1.58, 11.7; p = 0.004), and higher prevalence of myopic maculopathy progression (OR: 4.04; 95% CI: 1.60, 10.2; p = 0.003), or alternatively, higher prevalence of high myopia (OR: 4.44; 95% CI: 1.76, 11.2; p = 0.002). Circular GZE or BMO enlargement was associated with lower prevalence of macular BM defect enlargement (p = 0.035). GZE occurred perpendicular to the orientation of myopic lacquer cracks in 12 out of 17 (71%; 95% CI: 46, 95) eyes with lacquer cracks. Segmental GZE occurred in 49 (89%) out of 55 eyes in the same direction as shortening of the disc diameter developed.
Conclusions
The observations support the possibility of a posterior myopic axial elongation-associated BMO shift, leading to a segmental GZE in non-highly myopic eyes, followed by a circular GZE in highly myopic eyes. Large gamma zone might be protective against macular Bruch’s membrane defects.
Similar content being viewed by others
Introduction
Parapapillary gamma zone has been defined as the parapapillary region free of Bruch’s membrane (BM) [1,2,3,4,5,6]. In previous histomorphometric and clinical studies, size and prevalence of gamma zone was associated with longer axial length, more myopic refractive error, older age, and prevalence of macular BM defects [2, 3, 6, 7]. Longitudinal studies showed an association between widening of gamma zone and a corresponding change in the ophthalmoscopical shape of the optic disc, changing from a mostly circular form to a vertically oval one [8,9,10,11]. The reasons for the development and enlargement of gamma zone and for the associations between changes in gamma zone and morphometric changes in the posterior fundus including the optic nerve head have not fully been explored yet [7, 12]. We therefore conducted this study to assess the frequency and associations of a change in gamma zone in a 10-year follow-up in a population-based study to uncover hints for the aetiology of gamma zone and its clinical importance.
Methods
The population-based longitudinal Beijing Eye Study conducted in a rural region and urban area of Greater Beijing was first performed in the 2001 and repeated in 2011 [11]. Approving the study protocol, the Medical Ethics Committee of the Beijing Tongren Hospital confirmed that all methods were performed in accordance with the declaration of Helsinki and with the relevant guidelines and regulations. All study participants gave their written informed consent. As described in detail previously, all participants underwent a structured questionnaire, systemic examinations, and a comprehensive ophthalmic examination [13,14,15]. The ocular examinations included the determination of visual acuity, slit lamp examination and photography of the cornea, lens, optic disc and macula (fundus camera Type CR6-45NM; Canon Inc., Tokyo, Japan). In the year 2011, we additionally performed spectral-domain optical coherence tomography (OCT) of the macula and optic nerve head including the peripapillary area (enhanced depth imaging mode) (Spectralis®, Heidelberg Engineering Co, Heidelberg, Germany). We applied the optic disc scan protocol with six radial scan lines with a scan length of 6 mm, centred on the optic disc, and each scan consisting of 100 A-scans. The parapapillary region was examined with the intrinsic viewer (Heidelberg Eye Explorer software version 1.7.0.0; Heidelberg Engineering), which automatically synchronised the vertical lines of each B-scan and the infrared image taken by the OCT device. Parapapillary gamma zone was defined as the region between the end of BM and the border of the optic disc defined by the peripapillary border tissue of the peripapillary scleral flange Elschnig (i.e., the border of the lamina cribrosa).
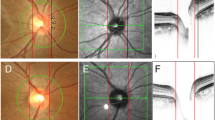
We additionally determined the horizontal diameter and vertical diameter of BM opening (BMO), with the measurement lines running through the optic disc centre, and the largest width of gamma zone and its location. Using the fundus photographs, we assessed the distance between the optic disc centre and the foveola. Parapapillary delta zone was defined as a region within gamma zone and which was located directly at the optic disc border and the peripheral margin of which was characterised by the peripapillary arterial circle of Zinn-Haller (if detectable), the merging line of the dura mater with the posterior sclera (if detectable on the OCT images) and/or by a difference in the ophthalmoscopical appearance on the fundus photographs. Comparing the fundus photographs taken in 2001 and in 2011, we noted any change in the size and shape of the optic disc, gamma zone and delta zone, angle kappa (defined as the angle between the temporal superior arterial arcade and the temporal inferior arterial arcade with the optic disc centre as its angle vertex), disc-fovea distance and angle (angle between the optic disc centre-fovea line and the horizontal), and stage of myopic maculopathy (Figs. 1 and 2). The latter was defined according to the META-analysis for Pathologic Myopia Study Group [16]. A change in the size of gamma zone was differentiated into a mostly circular gamma zone enlargement with an enlargement occurring mostly in all directions, and a segmental enlargement with the increase occurring predominantly in one direction. The optic disc area was defined as the ophthalmoscopically visible part of the neuroretinal rim and optic cup, i.e. the ophthalmoscopically visible part of the lamina cribrosa covered by the neuroretinal rim or showing the optic cup.
a Fundus photograph taking in 2001 (left image) and in 2011 (right image), with segmental enlargement of parapapillary gamma zone (yellow arrow) and decrease in the horizontal disc diameter (black bar in 2001; same black bar minus red bar in 2011); gamma zone enlargement and disc diameter reduction occurred in the same direction. b Fundus photograph taking in 2001 (left image) and in 2011 (right image), with segmental inferior enlargement of parapapillary gamma zone (yellow arrow) and decrease in the vertical disc diameter (black bar in 2001; same black bar minus red bar in 2011); gamma zone enlargement and disc diameter reduction occurred in the same direction; Note: disc-fovea (same red bars in 2001 and 2011) unchanged.
In the statistical analysis performed with the help of a software package (SPSS for Windows, version 25.0, IBM-SPSS, Chicago, IL, USA), we determined the mean frequencies of the outcome parameters (such as change in gamma zone and optic disc size) and expressed them as mean and 95% confidence intervals (CIs). In a binary regression analysis, we examined associations between the frequency of a gamma zone change and the frequencies of other ocular variables. A following multivariable analysis primarily included all parameters, which were significantly associated with the outcome parameter in the univariate analysis. We then dropped all parameters, which were no longer significantly with the outcome parameter in the multivariate analysis. We determined the odds ratio (ORs) and their 95% CIs. All p values were two-sided and considered statistically significant when they were <0.05.
Results
The investigation carried out in the year 2011 included 2695 participants from the baseline survey from 2001 [13,14,15]. The remaining of the 4439 participants originally taking part in the survey in 2001 had either died (n = 379), had moved (n = 1365), or were no longer interested in participating in the study. As also already described in detail previously, out of 204 highly myopic eyes (defined by a refractive error of ≤−6.0 dioptres and/or an axial length >26.0 mm) in the survey of 2001, 89 eyes (axial length: 27.6 ± 1.3 mm; range: 26.06–30.88 mm; 61 participants) were re-assessed in 2011 and had evaluable fundus images from both surveys [13,14,15]. These highly myopic participants did not differ in age from the remaining participants (age in 2011: 65.0 ± 9.8 years versus 64.7 ± 19.7 years; p = 0.17). The study additionally consisted of 86 randomly selected non-highly myopic eyes (57 individuals) which had also been assessed in 2001 and 2011, with a mean refractive error of −0.97 ± 2.61 dioptres in 2001 and −1.02 ± 2.45 dioptres in 2011, and a mean axial length of 23.6 ± 1.1 mm (range: 21.64–25.90 mm) [13,14,15]. The non-highly myopic group and the highly myopic group did not vary significantly in age (66.7 ± 9.7 years versus 65.0 ± 9.8 years; p = 0.25) and gender (p = 0.89).
An enlargement of gamma zone was observed in 93/175 eyes (53.1%; 95% CI; 45.7, 60.6), with a segmental gamma zone enlargement detected in 55/175 eyes (31.4%; 95% CI: 24.5, 38.4) and a circular gamma zone enlargement present in 38/175 eyes (21.7%; 95% CI; 16,28) (Table 1). None of the eyes showed a reduction in gamma zone size. Gamma zone enlargement occurred significantly (p < 0.001) more often in the highly myopic group than in the non-highly myopic group (gamma enlargement: 75/89 (84%; 95% CI: 77, 92) versus 18/86 (21%; 95% CI: 12, 30); circular gamma zone enlargement: 31/89 (35%; 95% CI: 25, 45) versus 7/86 (8%; 95% CI: 2, 14); segmental gamma zone enlargement: 44/89 (49%; 95% CI: 39, 60) versus 11/86 (13%, 95% CI: 6, 20).
In the eyes with a segmental gamma zone enlargement, the enlargement occurred most often into the temporal inferior direction (45%) followed by the temporal direction (32%), the inferior direction (11%), and the nasal direction (10%). In the eyes with a segmental gamma zone enlargement, an enlargement of gamma zone occurred in 49 (89%) of the 55 eyes in the same direction as a shortening of the disc diameter developed, while in the remaining eyes with a segmental gamma zone enlargement, the disc diameter either did not change or the disc diameter changed in a different direction than the gamma zone enlargement occurred.
In binary logistic regression analysis, gamma zone enlargement was associated (univariate analysis) with longer axial length (p < 0.001), enlargement of macular BM defects (p < 0.001), reduction in angle kappa (p < 0.001), high axial myopia versus non-highly axial myopia (P < 0.001), presence of macular BM defects in 2011 (P = 0.001), macular BM defect enlargement (P < 0.001), BMO enlargement (p < 0.001), BMO shift (p < 0.001), choroidal shift (p < 0.001), choroidal stretching (p < 0.001), presence of delta zone in 2001 (p < 0.001) and in 2011 and delta zone enlargement (p < 0.001), disc-fovea distance elongation (p < 0.001), stage of myopic maculopathy in 2001 (p < 0.001) and in 2011 (p < 0.001) and progression of myopic maculopathy (p < 0.001), optic disc enlargement (p < 0.001), optic disc size reduction (p < 0.001) and any optic disc size change (p < 0.001), straightening of the papillo-macular retinal vessels (p < 0.001), and temporal vascular arcade rotation (p < 0.001) (Table 2). It was not significantly associated with age (p = 0.21), gender (p = 0.20), higher intraocular pressure (IOP) (p = 0.04), the presence of macular BM defects in 2001 (p = 0.25), and choroidal rotation (p = 0.16). In multivariable analysis, a higher prevalence of gamma zone enlargement was correlated with a longer axial length (OR: 1.98; 95% CI: 1.37, 2.88; p < 0.001), and marginally significantly with a higher prevalence of myopic maculopathy progression (OR: 7.16; 95% CI: 0.79, 66.7; p = 0.08).
A segmental gamma zone enlargement was detected in 26 eyes (14.9%; 95% CI: 9.5, 20.2). A higher prevalence of a segmental gamma zone enlargement was associated (univariate analysis) with female gender (p = 0.04), the prevalence of the parameters of reduction in angle kappa (p = 0.001), disc-fovea distance elongation (p < 0.001), optic disc size reduction (p < 0.001), any optic disc size change (p < 0.001), and marginally with a higher prevalence of straightening of the papillo-macular retinal vessels (p = 0.06). It was not significantly correlated with age (p = 0.93), IOP (p = 0.78), the prevalence of longer axial length (p = 0.69), enlargement of macular BM defects (p = 0.59), prevalence of high axial myopia (p = 0.11), presence of macular BM defects in 2001 (p = 0.99) or 2011 (p = 0.99), macular BM defect enlargement (p = 0.59), choroidal shift (p = 0.47), choroidal stretching (p = 0.57), presence of delta zone in 2001 (p = 0.10) and in 2011 (p = 0.12) and delta zone enlargement (p = 0.17), stage of myopic maculopathy in 2001 (p = 0.76) and in 2011 (p = 0.79) and progression of myopic maculopathy (p = 0.27), optic disc enlargement (p = 0.12), and temporal vascular arcade rotation (p = 0.77). In multivariable analysis, a higher prevalence of segmental gamma zone enlargement was associated with a decrease in optic disc size (OR: 43.3; 95% CI: 10.9, 172; p < 0.001), longer disc-fovea distance (OR: 15.4; 95% CI: 3.12, 76.4; p = 0.001), and lower prevalence of high axial myopia (OR: 0.08; 95% CI: 0.01, 0.44; p = 0.001).
A circular gamma enlargement was detected in 38 eyes (21.7%; 95% CI: 16, 28). A higher prevalence of a circular gamma enlargement was associated with longer axial length (p = 0.001), higher IOP (p = 0.04), and with a higher prevalence of the parameters of reduction in angle kappa (p = 0.001), disc-fovea distance elongation (p < 0.001), optic disc enlargement (p < 0.001), any optic disc size change (p = 0.02), straightening of the papillo-macular retinal vessels (p < 0.001), enlargement of macular BM defects (p < 0.001), prevalence of high axial myopia (p < 0.001), presence of macular BM defects in 2011 (p = 0.01), macular BM defect enlargement (p < 0.001), choroidal shift (p < 0.001), choroidal stretching (p = 0.001), presence of delta zone in 2001 (p < 0.001) and in 2011 (p = 0.001) and delta zone enlargement (p < 0.001), stage of myopic maculopathy in 2001 (p < 0.001) and in 2011 (p < 0.001) and progression of myopic maculopathy (p < 0.001). It was not significantly correlated with age (p = 0.41), gender (p = 0.38), the prevalence of optic disc size reduction (p = 0.18), presence of macular BM defects in 2001 (p = 0.10), and temporal vascular arcade rotation (p = 0.76). In multivariable analysis, a higher prevalence of circular gamma enlargement was associated with a higher prevalence of an optic disc enlargement (OR: 4.30; 95% CI: 1.58, 11.7; p = 0.004) and higher prevalence of myopic maculopathy progression (OR: 4.04; 95% CI: 1.60, 10.2; p = 0.003), and marginally significantly with a higher prevalence of high myopia (OR: 2.82; 95% CI: 0.96, 8.27; p = 0.056).
In eyes with lacquer cracks or macular BM defects, detected in the year 2001 and/or in 2011, the orientation of the lacquer cracks was perpendicular to the direction of the gamma zone enlargement in 12 (71%; 95% CI: 46, 95)) out of 17 eyes.
Discussion
In this longitudinal population-based study, we observed an enlargement of gamma zone significantly more often in highly myopic eyes than in non-highly myopic eyes (84% versus 21%). None of the eyes showed a reduction in gamma zone size. Segmental gamma zone enlargement was associated with a decrease in optic disc size, longer disc-fovea distance and lower prevalence of high axial myopia, while circular gamma enlargement correlated with optic disc enlargement and myopic maculopathy progression or alternatively with high myopia. Gamma zone enlargement predominantly occurred perpendicular to the orientation of myopic lacquer cracks and in the same direction as shortening of the disc diameter and elongation of the disc-fovea distance occurred.
Some findings obtained in our study agree with observations made in previous investigations. The association between gamma zone enlargement and lengthening of the disc-fovea distance supports the notion that the length of BM on the disc-fovea line does not change with axial elongation and that the axial elongation-associated increase in the disc-fovea distance is mostly due to the development and widening of gamma zone [14, 17]. The observation that a segmental widening of gamma zone correlated with a decrease in the disc diameter lying in the same direction in which the maximal gamma widening occurred fits with the notion of a shift of BMO into the posterior direction (Fig. 3) [13, 18]. This BMO shift may lead to an overhanging of BM into the intrapapillary compartment at the nasal disc border, and to a lack of BM at the temporal disc border, with the subsequent development of a temporal gamma zone [18, 19]. Due to the shift of the nasal BM margin into the intrapapillary region, the ophthalmoscopically visible part of the lamina cribrosa decreases, since its nasal part is covered by the overhanging BM border [13, 18, 19]. The enlargement of gamma zone was associated with a higher prevalence of moderate myopia while the prevalence of circular gamma enlargement was higher in the highly myopic group. It may give a hint that the process of myopic axial elongation may include first, in moderately myopic eyes, a shift of the BMO unchanged in its size and leading to the development and enlargement of a (temporal) gamma zone. If further axial elongation occurs, the BMO may enlarge in then highly myopic eyes. This BMO enlargement may lead to a circular enlargement of gamma zone, with a retraction of the formerly overhanging BM part at the nasal optic disc border and secondary enlargement of the ophthalmoscopically visible optic disc. In agreement with the notion of a shift of the BMO as the primary step of gamma zone development is the finding that the prevalence of a segmental gamma zone enlargement, without accompanying BMO enlargement, was associated with a lower prevalence of high myopia. In contrast, a circular gamma zone enlargement, in association with a BMO enlargement, was detected mainly in highly myopic eyes.
These three layers of the optic nerve head canal may be aligned to each in the newborn (this Figure, upper part). In the process of myopic axial elongation, the BMO may shift, usually in direction to the fovea (this Figure, middle part). It leads to an overhanging of Bruch’s membrane (BM) at the nasal optic disc border, and to an absence of BM at the temporal side of the optic disc, called parapapillary gamma zone. Due to the BMO shift, the overhanging BM covering the nasal part of the anatomical optic disc (defined as all the region with the lamina cribrosa as its bottom) prevents this optic disc part from being detectable upon ophthalmoscopy. It leads to a reduction of the ophthalmoscopically visible optic disc area. With further axial elongation in highly myopic eyes, the BMO enlarges, leading to a circular gamma zone and to an increase in the ophthalmoscopic optic disc size (due to the retraction of the overhanging part of BM), in addition due to an enlargement of the lamina cribrosa (this Figure, lower part).
The hypothesis of a shift of the BMO as part of the posterior BM in the non-highly eyes is supported by the observation, that the direction of the segmental gamma enlargement was parallel to the elongation of the disc-fovea distance, suggesting that the posterior BM as a whole, including the BMO, moved backward in relationship to the scleral flange opening (i.e., the lamina cribrosa). The latter relatively stayed back, i.e., remained to be located more anteriorly [17]. This notion fits with the anatomic finding, that in eyes with temporal gamma zone, the macular retinal ganglion cell axons enter the optic nerve head canal in the direction from posterior to anterior, before bending posteriorly when leaving the lamina cribrosa and running towards the apex of the orbit [13]. It also fits with the finding that the disc diameter decreased in the same direction in which gamma zone widened most. It is in contrast to the hypothesis that it is an anterior shift of the lamina cribrosa leading to the oblique retinal nerve fibre exit out of the axially elongated globe, as discussed by Kim et al. [12]. An assumed anterior shift of the lamina cribrosa, as compared to a posterior shift of the BMO, with both mechanisms leading to an oblique, anteriorly directed exit of the retinal nerve fibres, may however be unlikely, since the optic nerve fibres anyway have to turn posteriorly to leave the orbit in the posterior superior orbital region. In particular, the assumed backward pull of the optic nerve which might get too short to allow a full adduction of highly myopic eyes would make one assume a posterior, and not an anterior, shift of the lamina cribrosa, since the optic nerve dura mater indirectly inserts at the lamina cribrosa through the peripapillary scleral flange [7, 20, 21].
The observation that the direction of the segmental gamma zone widening occurred usually in a direction perpendicular to the orientation of lacquer cracks supports the notion, that axial elongation is associated with an increased strain in the BM, first perhaps leading to a widening of the BMO, and if the relaxing effect of that is not sufficient, to the development of additional BM breaks (i.e., lacquer cracks) in the macular region [18]. The increased BM strain at the posterior pole may perhaps be due to the myopic enlargement of the globe in the horizontal and vertical globe diameters, with one millimetre axial elongation being association with about 0.1 mm increase in the coronal globe diameters [22].
The association between an enlargement of gamma zone and a narrowing of angle kappa can geometrically be explained. Since the distance between the temporal superior vascular arcade and temporal inferior vascular arcade, measured on a vertical line running through the fovea does not change in axial elongation, angle kappa decreases if the disc-fovea-distance increases [14, 17]. The association between a widening of the gamma zone and a straightening of the macular retinal vessels can also geometrically be explained by the elongation of the disc-fovea distance, since the retinal vessels and the retinal nerve fibres are the only connection between the,macular retina and the optic disc. Interestingly, none of the eyes showed a reduction in gamma zone size. It is in contrast to a case series study which examined patients with a marked reduction of IOP into the single digit range by anti-glaucomatous surgery, and in which a decrease in the width of gamma zone was observed [23]. It raises the question of the role of the IOP in the appearance of gamma zone and on the possibility of the BM to shift in dependence of a low IOP. Interestingly, in our study in which the minimal IOP was 9 mm Hg, a change in gamma zone was not associated with IOP in the multivariable analysis.
The reason for the assumed backward shift of BMO has remained elusive so far. One may perhaps discuss that the process of myopic axial elongation occurs by a growth of BM in the equatorial region. It would change the spherical eye shape to ta prolate form, push back the posterior BM, and lead to a secondary compression and thinning of the choroid, most marked at the posterior pole. It would also lead to a posterior shift of the BMO in relationship to the peripapillary scleral flange opening (lamina cribrosa), since the sclera, not being the primary mover in the process, would lag behind the movement of BM [18]. It has also remained unclear why an enlargement of the BMO may not occur in non-highly myopic eyes. One may speculate that the presumed enlargement of the BM in the equatorial region may be directed predominantly into the posterior direction, leading mostly to an elongation of the anterior-posterior axis (“myopic axial elongation”). In highly myopic eyes, the equatorial BM enlargement may additionally occur in the coronal plane, leading to an increase in the vertical and horizontal globe diameters. Due to geometric reasons, this change in the globe shape may lead to a stretching of BM in the posterior segment, leading potentially first to an enlargement of the BMO, followed by the development of additional BM defects in the macular region.
A limitation of our study should be considered. Out of 204 highly myopic eyes examined in the year 2001, only 89 (43.6%) were re-examined in the year 2011. This rate of re-participation of 44% is relatively low, however it may be acceptable for a 10-year follow-up of a population-based investigation of adult and elderly individuals. In addition, a main purpose of our study was to assess factors associated with an enlargement of parapapillary gamma zone.
In conclusion, the findings may support the possibility of a shifting and enlarging BMO in myopic eyes. In a first step, in non-highly myopic eyes, the BMO might shift usually into the temporal direction, leading potentially to an overhanging of BM into the intrapapillary compartment, development of gamma zone at the opposite disc side, a subsequent reduction in the ophthalmoscopically visible optic disc area and an elongation of the disc-fovea distance. In a second step, in highly myopic eyes, the BMO might enlarge leading to the development of a circular gamma zone and enlargement of the ophthalmoscopical visible optic disc due to a retraction of the overhanging BM. As a speculation, the cause for the backward shift of the BMO might be an enlargement of the BM in the equatorial region, mostly in the anterior-posterior direction, potentially leading to a change in the globe shape from a spherical form to a prolate shape [18].
Summary
What was known before
-
Parapapillary gamma zone has been defined as the parapapillary region free of Bruch’s membrane (BM).
-
In previous histomorphometric and clinical studies, size and prevalence of gamma zone was associated with longer axial length, more myopic refractive error, older age, and prevalence of macular BM defects.
-
Longitudinal studies showed an association between widening of gamma zone and a corresponding change in the ophthalmoscopical shape of the optic disc, changing from a mostly circular form to a vertically oval one.
-
The reasons for the development and enlargement of gamma zone and for the associations between changes in gamma zone and morphometric changes in the posterior fundus including the optic nerve head have not fully been explored yet.
What this study adds
-
The observations support the notion of a posterior myopic axial elongation-associated Bruch’s membrane opening shift, leading to a segmental gamma zone enlargement in non-highly myopic eyes, followed by a circular gamma zone enlargement in highly myopic eyes.
-
Large gamma zone may be protective against macular Bruch’s membrane defects.
Change history
28 February 2022
The figures were changed to color figures in pdf.
References
Jonas JB, Jonas SB, Jonas RA, Holbach L, Panda-Jonas S. Histology of the parapapillary region in high myopia. Am J Ophthalmol. 2011;152:1021–9.
Jonas JB, Jonas SB, Jonas RA, Holbach L, Dai Y, Sun X, et al. Parapapillary atrophy: histological gamma zone and delta zone. PLoS ONE. 2012;7:e47237.
Jonas JB, Ohno-Matsui K, Spaide RF, Holbach L, Panda-Jonas S. Macular Bruch’s membrane defects and axial length: association with gamma zone and delta zone in peripapillary region. Invest Ophthalmol Vis Sci. 2013;54:1295–302.
Da Y, Jonas JB, Huang H, Wang M, Sun X. Microstructure of parapapillary atrophy: beta zone and gamma zone. Invest Ophthalmol Vis Sci. 2013;54:2013–8.
Kim M, Kim TW, Weinreb RN, Lee EJ. Differentiation of parapapillary atrophy using spectral-domain optical coherence tomography. Ophthalmology. 2013;120:1790–7.
Kim M, Choung HK, Lee KM, Oh S, Kim SH. Longitudinal changes of optic nerve head and peripapillary structure during childhood myopia progression on OCT: Boramae Myopia Cohort Study Report 1. Ophthalmology. 2018;125:1215–23.
Wang YX, Panda-Jonas S, Jonas JB. Optic nerve head anatomy in myopia and glaucoma, including parapapillary zones alpha, beta, gamma and delta: histology and clinical features. Prog Retin Eye Res. 2020;83:100933.
Kim TW, Kim M, Weinreb RN, Woo SJ, Park KH, Hwang JM. Optic disc change with incipient myopia of childhood. Ophthalmology. 2012;119:21–6.
Lee KM, Choung HK, Kim M, Oh S, Kim SH. Change of β-zone parapapillary atrophy during axial elongation: Boramae Myopia Cohort Study Report 3. Invest Ophthalmol Vis Sci. 2018;59:4020–30.
Guo Y, Liu LJ, Tang P, Feng Y, Lv YY, Wu M, et al. Parapapillary gamma zone and progression of myopia in school children: The Beijing Children Eye Study. Invest Ophthalmol Vis Sci. 2018;59:1609–16.
Yan YN, Wang YX, Yang Y, Xu L, Xu J, Wang Q, et al. Ten-year progression of myopic maculopathy: the Beijing Eye Study 2001-2011. Ophthalmology. 2018;125:1253–63.
Lee KM, Choung HK, Kim M, Oh S, Kim SH. Positional change of optic nerve head vasculature during axial elongation as evidence of lamina cribrosa shifting: Boramae Myopia Cohort Study Report 2. Ophthalmology. 2018;125:1224–33.
Zhang Q, Wang YX, Wei WB, Xu L, Jonas JB. Parapapillary beta zone and gamma zone in a normal population: the Beijing Eye Study 2011. Invest Ophthalmol Vis Sci. 2018;59:3320–9.
Jonas RA, Yan YN, Zhang Q, Wang YX, Jonas JB. Elongation of the disc-fovea distance and retinal vessel straightening in a 10-year follow-up of the Beijing Eye Study. Sci Rep. 2021;11:9006.
Jonas RA, Brandt CF, Zhang Q, Wang YX, Jonas JB. Location of parapapillary gamma zone and vertical fovea location. the Beijing Eye Study 2011. Invest Ophthalmol Vis Sci. 2021;62:18.
Ohno-Matsui K, Kawasaki R, Jonas JB, Gemmy-Cheung CM, Saw SM, Verhoeven V, et al. International classification and grading system for myopic maculopathy. Am J Ophthalmol. 2015;159:877–83.
Jonas JB, Wang YX, Zhang Q, Liu Y, Xu L, Wei WB. Macular Bruch’s membrane length and axial length. The Beijing Eye Study. PLoS ONE. 2015;10:e0136833.
Jonas JB, Ohno-Matsui K, Jiang WJ, Panda-Jonas S. Bruch membrane and the mechanism of myopization. A new theory. Retina. 2017;37:1428–40.
Reis AS, Sharpe GP, Yang H, Nicolela MT, Burgoyne CF, Chauhan BC. Optic disc margin anatomy in patients with glaucoma and normal controls with spectral domain optical coherence tomography. Ophthalmology. 2012;119:738–47.
Demer JL. Optic nerve sheath as a novel mechanical load on the globe in ocular duction. Invest Ophthalmol Vis Sci. 2016;57:1826–38.
Wang X, Fisher LK, Milea D, Jonas JB, Girard MJA. Predictions of optic nerve traction forces and peripapillary tissue stresses following horizontal eye movements. Invest Ophthalmol Vis Sci. 2017;58:2044–53.
Jonas JB, Ohno-Matsui K, Holbach L, Panda-Jonas S. Association between axial length and horizontal and vertical globe diameters. Graefes Arch Clin Exp Ophthalmol. 2017;255:237–42.
Panda-Jonas S, Xu L, Yang H, Wang YX, Jonas SB, Jonas JB. Optic disc morphology in young patients after antiglaucomatous filtering surgery. Acta Ophthalmol. 2014;92:59–64.
Funding
National Natural Science Foundation of China (#81570835).
Author information
Authors and Affiliations
Contributions
All authors participated in the design of the study, collection and analysis of data, and writing and final approval of the manuscript
Corresponding author
Ethics declarations
Competing interests
JBJ and RAJ: European patent application 16 720 043.5 and US patent application US 2019 0085065 A1: Agents for use in the therapeutic or prophylactic treatment of myopia or hyperopia). JBJ: Advisory Board Novartis; Patent holder with Biocompatibles UK Ltd. (Farnham, Surrey, UK) (Title: Treatment of eye diseases using encapsulated cells encoding and secreting neuroprotective factor and/or anti-angiogenic factor; Patent number: 20120263794), Patent application: Agents for the use in the therapeutic or prophylactic treatment of retinal pigment epithelium associated diseases. All other authors: None.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jonas, J.B., Zhang, Q., Xu, L. et al. Parapapillary gamma zone enlargement in a 10-year follow-up: the Beijing Eye Study 2001–2011. Eye 37, 524–530 (2023). https://doi.org/10.1038/s41433-022-01978-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-01978-8