Abstract
Background/aims
Amblyopia is the most common visual deficit in children and accurate visual acuity (VA) assessment is essential for diagnosis. While ETDRS high-contrast logMAR VA is the reference standard test for adults, less agreement exists for pre-literate children. A new picture optotype acuity test (The Auckland Optotypes [TAO]) has shown favourable comparison to letter acuity charts but has not yet been evaluated in children with amblyopia. This study aimed to compare VA obtained using TAO to crowded logMAR letters in children age 5–8 years with amblyopia.
Methods
Children with amblyopia (n = 54 [20.37% strabismic, 18.52% anisometropic, 61.11% mixed], mean age 78.30 ± 11.72 months) were recruited from paediatric ophthalmology/orthoptic clinics at Moorfields Eye Hospital NHS Foundation Trust, London, and Cambridge Community Services NHS Trust, Bedford. Best-corrected VA was measured in both the amblyopic eye (AE) and fellow eye (FE) using TAO and a crowded letter acuity chart. Bland–Altman analysis was used to measure 95% limits of agreement (LoA) for VA measures captured (AE, FE and interocular difference [IOD]).
Results
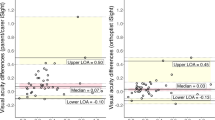
Good agreement between TAO and letter VA measurement was observed (mean bias: AE –0.01, FE 0.01, IOD –0.02). For AE measures 95% LoA were from –0.25 to 0.24 logMAR, this being similar for FE (–0.24 to 0.25) and IOD measures (–0.30 to 0.27).
Conclusion
TAO and letters elicited similar VA in children with amblyopia. TAO could be a useful picture-based chart for paediatric vision assessment.
Similar content being viewed by others
Introduction
Accurate measurement of visual acuity (VA) is central to the detection of amblyopia, the most common vision deficit in childhood, and the monitoring of treatment efficacy. Measuring VA in children is difficult and requires age-appropriate tests and experienced clinicians. The Early Treatment Diabetic Retinopathy Study (ETDRS) chart is the reference standard VA test for adults; however, it is not suitable for pre-literate children. Picture-based vision charts have been designed to address this; however, these often have their own limitations, for example, overestimation of VA compared to letter optotypes [1,2,3,4].
In the UK, in pre-literate children the Kay Picture test [1] is widely used. Clinical validation has shown that it overestimates VA by 0.10–0.20 logMAR, compared to crowded letter tests [2, 3]. In children with amblyopia, Kay Picture values have been found to differ from ETDRS measurements by around 0.20 logMAR. There has also been a suggestion of proportional bias, with increasing VA overestimate with worsening levels of VA [4]. The Kay Pictures subsequently have been redesigned to address some of these issues but with limited validation [5].
Recently, a new picture optotype test, The Auckland Optotypes (TAO), has been developed [6]. TAO is an open access set of psychometrically robust, picture optotypes. It consists of ten optotypes that have a consistent stroke width, 1:1 aspect ratio and are fully enclosed with limited acute angles (Fig. 1). Existing evidence suggests that VA obtained with TAO is comparable to that obtained with ETDRS in adults. Similarly, strong agreement has been found between TAO and Sloan letters as well as Lea symbols in visually normal children [6,7,8]. Such agreement is promising and suggests that TAO could enhance the accuracy of VA assessment in pre-literate children and potentially fulfil the criteria for a picture optotype test suitable for use in clinical trials. However, before TAO could be advocated for clinical or research use, validation in children with visual difficulties and in particular amblyopia is required.
The aim of this study was to examine the agreement of VA measurements obtained using TAO to that of the reference standard VA test for children with amblyopia crowded logMAR letters (HOTV/Keeler Crowded logMAR).
Methods
Participants
Fifty-four children aged 5–8 years (mean ± SD, 78.30 ± 11.72 months) with unilateral amblyopia were recruited to this study between 13 June 2019 and 27 February 2020. Amblyopia was defined as an interocular difference (IOD) ≥0.20 logMAR, with fellow eye (FE) acuity of 0.20 logMAR or better. Children with a history of intraocular surgery, current ocular surface inflammation, glaucoma, cataract or developmental delay were excluded. Due to screen size limitations, participants with VA > 1.40 logMAR were excluded. Ethical approval was obtained from the Research Ethics Committee London – Surrey (19/LO/0519). All procedures adhered to the tenets of the Declaration of Helsinki. Informed parental consent was obtained prior to study procedures and children also provided written assent where appropriate.
Psychophysical procedure
Study procedures were undertaken at Moorfields Eye Hospital NHS Foundation Trust, City Road, London (site 1) and Cambridgeshire Community NHS Trust, Bedford (site 2). At both sites, a consistent clinical testing room was used for test presentation, i.e., both optotype acuity tests were presented under the same room illumination and the test chart brightness was >80 cd/m2 for all measures. Testing order of acuity tests was randomised using simple block randomisation.
At site 1, both TAO and letter (HOTV) tests were presented on a 19” GNR TS902 LCD monitor (pixel resolution 1280 × 1024, refresh rate 60 Hz) via the COMPlog computerised system calibrated for a 3.5 m viewing distance. The COMPlog testing algorithm employs an initial range finding phase whereby a single crowded optotype is presented in 0.20 logMAR steps until a single reversal is obtained. Threshold VA was then measured by presenting a single line of five optotypes, separated by half an optotype width and surrounded by an overall crowding box, decreasing in 0.10 logMAR intervals. If all five optotypes could not be simultaneously presented due to limitations in screen size, the lines were broken into smaller numbers of optotypes such that a cumulative total of five optotypes was presented for each line size. This was the case for both TAO and letter tests. The simultaneous presentation of five optotypes per line could occur from 0.80 logMAR. Testing was terminated once all optotypes at a given VA level (i.e., a whole line) were incorrectly identified.
At site 2, TAO and letters were presented as hand-held tests at 3 m distance. TAO was presented on a hand-held Microsoft Surface Go 10-inch tablet (screen resolution: 1800 × 1200, refresh rate: 60 Hz) via COMPlog, as above. Letter acuity was assessed using hand-held Keeler LogMAR Crowded Test in a similar two-stage process. Initially participants were asked to identify either the second or third letter on a line, decreasing in 0.20 logMAR steps until one letter was incorrectly identified. Threshold VA testing then began from the last correct response, decreasing in 0.10 logMAR intervals. Testing was terminated once all optotypes on the line were incorrectly identified.
Data collection was undertaken by experienced orthoptists/paediatric optometrist. An opaque occluder was used for uniocular testing; the amblyopic eye (AE) was always tested first. Participants were instructed to name the optotypes aloud; a matching card was permitted if required. A forced-choice procedure was employed in all cases to minimise the effect of observer criterion, i.e., if children were unsure of the optotype presented at threshold, they were encouraged to attempt/guess before termination. Optotype presentation duration was unlimited and, in all cases, single optotype scoring was applied. VA was recorded in standard logMAR notation. A scaling factor (–0.216 logMAR) was applied to TAO measures to account for a different bounding box to stroke width ratio compared with Sloan letters (SC Dakin, personal communication, 2019). The stroke width/total optotype ratio for TAO is 1:8.23, compared to 1:5 for Snellen, 1:7 for Lea Symbols and 1:10 for Kay pictures. Therefore, such a scaling factor is required to achieve equivalence between different optotype sets [6].
Data analysis
Analysis was conducted using MATLAB 2020a (The MathWorks Inc., USA). Bland–Altman limits of agreement (LoA) analysis was used to measure agreement between the VA tests. The upper and lower 95% LoA and associated 95% confidence intervals were calculated. Proportional bias was evaluated using Pearson’s correlation and ordinary least-squares linear regression analysis. VA measures in the AE and FE, in addition to IOD were evaluated separately. Equality plots were also constructed for AE, FE and IOD comparisons between charts, with paired samples t-tests being undertaken to determine if there were statistically significant differences in these measures with each chart form. A three-way ANOVA with the fixed effects of chart type and testing site, together with the random effect of amblyopia severity was performed to examine what experimental factors may influence the IOD measures captured in this study. For the purposes of this analysis, amblyopia severity was determined by logMAR letter acuity in the AE. AE acuity <0.6 was considered moderate amblyopia and ≥0.6 severe amblyopia [9, 10]. An α of 0.05 was considered statistically significant with Holm–Bonferroni correction being applied to P values where necessary.
Results
All participants successfully completed both TAO and logMAR letter VA tests. Participant characteristics are detailed in Table 1.
Bland–Altman analysis indicated good agreement between TAO and crowded logMAR letters (Fig. 2a–c). LoA for FE measurements were ±0.25 logMAR, with similar values for AE (±0.24 logMAR) and IOD (±0.32 logMAR). A paired t-test (with Holm–Bonferroni correction) also revealed there to be no statistically significant differences in either FE (P = 0.49), AE (P = 0.79) and IOD (P = 0.45) measurements with either test examined. No statistically significant proportional bias between chart forms was observed for AE (r2 = 0.04, P = 0.16) and FE measures (r2 = 0.06, P = 0.07), but was evident for FE measures (r2 = 0.08, P = 0.04, Fig. 2c) whereby IOD measures appeared to be underestimated by TAO relative to letter acuity measures when amblyopia was more dense. A similar trend may be observed from the equality plot examining the relationship between IOD measures with TAO and logMAR letter acuity (Fig. 2e). Further examination also revealed there to be statistically significant interaction effects between study site and amblyopia grade (F(1,107) = 8, P = 0.005) on IOD values. No other interaction effects were observed. Post-hoc analysis (Fig. 3) revealed there be markedly lower IOD values in participants at site 2 compared to site 1 (P < 0.001, Fig. 3c), this reflecting the fact that relatively fewer patients with severe amblyopia were recruited at this site compared to site 1 (Table 1).
a–c Bland–Altman LoA plots indicate good agreement between TAO and crowded logMAR letters for the amblyopic eye (a), fellow eye (b) and interocular difference measures (c). 95% confidence intervals surrounding the 95% LOA are represented by grey shading with different plot markers for each test site. d–f Equality plots comparing TAO and logMAR. Ordinary least-squares linear regression line is included (black) along with an equality line (grey).
Discussion
Good agreement was established between TAO and letter VA (Fig. 2a–c), indicating that TAO appears to be an equivalent measure to letter VA in children with amblyopia. The 95% LoA established in this study in the AE (±0.24 logMAR) and FE (±0.25 logMAR) were similar to, albeit slightly wider than, previously reported comparisons between TAO and logMAR letters in visually normal children (±0.20 logMAR) [7, 8]. The LoA observed in this study are also in line with those for well-established and widely used picture acuity charts. For example, in a paediatric population the agreement between Lea Symbols and ETDRS has been shown to be in the region of 0.30 to –0.20 logMAR [11]. LoA between Kay Pictures and Keeler crowded logMAR charts, both of which have fewer optotype alternatives than TAO, has been reported as 0.225 to –0.030 logMAR [3, 5, 11]. However, TAO does appear advantageous as the mean bias observed in this analysis is lower than that reported for other picture acuity charts indicating closer agreement with VA measures with the reference standard ETDRS chart [3, 5, 11].
While there was no overall influence of study site on observed trends for IOD measures with each chart form (Fig. 3a), site 1 did exhibit higher overall IOD values in children with severe amblyopia (AE ≥0.6 logMAR, Fig. 3c). We hypothesise that this observed difference in overall IOD (across both chart forms) is a result of differences in the cohorts recruited at each study site, rather than any systematic differences between tests, investigators or study procedures at each site. Indeed, it may be seen from Fig. 3c that a greater number of patients with dense amblyopia (as defined using logMAR letter VA) were recruited and tested at site 1 compared to site 2.
While we observed good agreement between TAO and letter VA, TAO appeared to underestimate IOD relative to letters in severe amblyopia (≥0.6 crowded letter logMAR, Figs. 2a and 3b). This underestimation is somewhat surprising as the agreement between amblyopic and FE acuity using TAO compared to letter optotypes was a good level and similar LoA were found for either eye. We propose that this underestimation of IOD in severe amblyopia is a result of differences in TAO design compared to letters. For example, TAO, consisting of ten optotypes, contains more possible alternatives than the letters used in paediatric letter charts considered in this study. It has been demonstrated that the number of alternatives in a forced choice (AFC) test is inversely related to VA threshold measures [12, 13]; the letter tests used in this study being truncated (COMPlog: 4-AFC, Keeler: 6-AFC) relative to TAO (10-AFC) that could contribute to lower IOD in severe amblyopia as there is increased probability of an incorrect ‘guess’ at threshold with TAO. TAO optotypes also lack acute angles that could potentially increase their difficulty relative to letters at threshold [14, 15]. Further examination of the equality plot comparing TAO and letter VA for the FE in the cohort examined (Fig. 2e) would suggest that such issues appear to bias measures primarily at the higher VA range (better than 0.20 logMAR). It is also possible that this trend could also be attributed to the small participant sample within this VA range (n = 14) or increased measurement variability in severe amblyopia. As this was an unexpected finding in this sample, further work with an appropriate sample size would be beneficial to specifically determine if IOD varies with amblyopia severity when examined with TAO and conventional tests. Further work incorporating inter and intra-test variability would also be useful to evaluate the precision of cross-sectional and longitudinal VA measures with TAO in amblyopia.
No proportional bias was observed with AE measures, this being evident in both the Bland–Altman (Fig. 2a) and equality plots (Fig. 2d). This is particularly relevant in amblyopia as poorer AE VA triggers increased patching doses; thus, any VA overestimation could result in insufficient treatment for the severity of the condition. Therefore, TAO could be advantageous in the accurate estimate of AE acuity in pre-literate children.
Conclusions
This study describes the first comparison of TAO to logMAR letters in children with amblyopia. Good agreement was found between the tests, using a clinical testing protocol, suggesting that TAO could be appropriate for clinical VA measures in children with amblyopia. We recognise that this is a preliminary study and a larger sample size would be advantageous to expand on these findings. Further investigation of TAO VA measures in younger children and in severe amblyopia would be advantageous.
Summary
What was known before
-
N/A
What this study adds
-
This study describes the first comparison of TAO to logMAR letters in children with amblyopia. Good agreement was found between the tests, using a clinical testing protocol, suggesting that TAO could be appropriate for clinical VA measures in children with amblyopia.
References
Kay H. New method of assessing visual acuity with pictures. Br J Ophthalmol. 1983;67:131–3.
Anstice NS, Jacobs RJ, Simkin SK, Thomson M, Thompson B, Collins AV. Do picture-based charts overestimate visual acuity? Comparison of Kay Pictures, Lea Symbols, HOTV and Keeler logMAR charts with Sloan letters in adults and children. PLoS One. 2017;12:e0170839.
O’Boyle C, Chen SI, Little JA. Crowded letter and crowded picture logMAR acuity in children with amblyopia: a quantitative comparison. Br J Ophthalmol. 2017;101:457–61.
Shah N, Laidlaw DA, Rashid S, Hysi P. Validation of printed and computerised crowded Kay picture logMAR tests against gold standard ETDRS acuity test chart measurements in adult and amblyopic paediatric subjects. Eye (Lond). 2012;26:593–600.
Milling A, Newsham D, Tidbury L, O’Connor AR, Kay H. The redevelopment of the Kay picture test of visual acuity. Br Ir Orthopt J. 2015;13:14–21.
Hamm LM, Yeoman JP, Anstice N, Dakin SC. The Auckland Optotypes: an open-access pictogram set for measuring recognition acuity. J Vis. 2018;18:13.
Hamm LM, Langridge F, Black JM, Anstice NS, Vuki M, Fakakovikaetau T, et al. Evaluation of vision screening of 5-15-year-old children in three Tongan schools: comparison of The Auckland Optotypes and Lea symbols. Clin Exp Optom. 2020;103:353–60.
Hamm LM, Anstice NS, Black JM, Dakin SC. Recognition acuity in children measured using The Auckland Optotypes. Ophthalmic Physiol Opt. 2018;38:596–608.
Group PEDI. The clinical profile of moderate amblyopia in children younger than 7 years. Arch Ophthalmol. 2002;120:281–7.
Holmes JM, Kraker RT, Beck RW, Birch EE, Cotter SA, Everett DF, et al. A randomized trial of prescribed patching regimens for treatment of severe amblyopia in children. Ophthalmology. 2003;110:2075–87.
Dobson V, Clifford-Donaldson CE, Miller JM, Garvey KA, Harvey EM. A comparison of Lea Symbol vs ETDRS letter distance visual acuity in a population of young children with a high prevalence of astigmatism. J Aapos. 2009;13:253–7.
Shah N, Dakin SC, Redmond T, Anderson RS. Vanishing Optotype acuity: repeatability and effect of the number of alternatives. Ophthalmic Physiol Opt. 2011;31:17–22.
Carkeet A. Modeling logMAR visual acuity scores: effects of termination rules and alternative forced-choice options. Optom Vis Sci. 2001;78:529–38.
Ferris FL, Freidlin V, Kassoff A, Green SB, Milton RC. Relative letter and position difficulty on visual acuity charts from the Early Treatment Diabetic Retinopathy Study. Am J Ophthalmol. 1993;116:735–40.
Sloan LL, Rowland WM, Altman A. Comparison of three types of test target for the measurement of visual acuity. Q Rev Ophthalmol. 1952;8:4–16.
Acknowledgements
The authors would like to thank Professor Steven Dakin for his assistance in illustration of TAO optotypes for this paper. We also express our gratitude to the patients of Moorfields Eye Hospital Paediatric Clinic and Cambridge Community Services (Bedford) Eye Clinic and their parents/guardians who kindly gave their time to participate in this research.
Funding
Supported in part by an in-practice research grant from the College of Optometrists (EMMcV), a research award grant from the British Isles Paediatric Ophthalmology and Strabismus Association (BIPOSA) (SML) and by the National Institute for Health Research (NIHR) Biomedical Research Centre based at Moorfields Eye Hospital NHS Foundation Trust and UCL Institute of Ophthalmology (AD-N, PJM, NS). The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
Author information
Authors and Affiliations
Contributions
EMMcV was responsible for the College of Optometrists funding application, assisting with ethics application, recruitment of participants, acquisition of data, statistical analysis and drafting the final manuscript. SML was responsible for the initial study design and concept, protocol development, BIPOSA funding application, ethics application, recruitment of participants, acquisition of data, statistical analysis and drafting the final manuscript. SM was responsible for the recruitment of participants at site 2 and acquisition of data. NS was responsible for assisting in the College of Optometrists funding application, editing the final manuscript, administrative, technical or material support and supervision. PJM was responsible for assisting in the College of Optometrists funding application and editing the final manuscript, statistical analysis, administrative, technical or material support and supervision. AD-N was responsible for the initial design and concept of the study, NIHR Biomedical Research Centre grant application, ethics application, overseeing the study, editing the final manuscript, statistical analysis, administrative, technical or material support and supervision. EMMcV and SML had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. All authors contributed to analysis/interpretation of data, drafting of the manuscript and critical revision of the manuscript for important intellectual content.
Corresponding author
Ethics declarations
Competing interests
PJM: Heidelberg Engineering & LKC Inc. (research support). NS: The Moorfields Acuity Chart (co-inventor) and COMPlog Clinical Vision Measurement Systems Ltd. (research support). AD-N: Santen Inc. (medical advisor).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
McVeigh, E.M., Ludden, S.M., Mohamed, S. et al. Preliminary clinical validation of a new picture–based visual acuity test in children with amblyopia: a comparison of The Auckland Optotypes and crowded logMAR letters. Eye 36, 2341–2345 (2022). https://doi.org/10.1038/s41433-021-01840-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01840-3