Abstract
Objectives
This paper evaluates the accuracy of the Eye-N-JOY (ENJ), a novel device (Patent no. US 9844317 B2), for identifying the presence of amblyopic risk factors. This device was developed to assess both visual acuity, ocular alignment, and eye movement; all while watching images on a tablet screen.
Methods
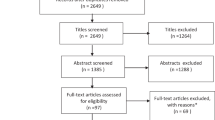
A prospective, single-center, comparison study. Participants were examined by the ENJ first and then underwent a comprehensive full eye examination by pediatric ophthalmologists including cycloplegic refraction. Both the technician operating the ENJ and the physicians were masked to each other’s findings. Children aged 18–72 months (1.5 to 6 years) attending a tertiary medical center for a full standard pediatric ophthalmology examination were included. The visual acuity and alignment were compared between the ENJ and the gold standard full ophthalmologic examination. The differences were noted, and the sensitivity and specificity were calculated.
Results
A total of 51 children were enrolled, 33 (64.7%) girls, aged 18–72 months. All children successfully completed the examination by the ENJ. No significant difference between the ENJ and the reference examination was detected in visual acuity measurements in both eyes (Pv = 0.553 for the right eye and 0.803 for the left). Overall agreement between all referral indications between the ENJ and reference examination was 84.3%, with 90.9% agreement in VA referral criteria and 90.1% in alignment referral criteria.
Conclusions
Eye-N-Joy can reliably examine both visual acuity and ocular misalignment in verbal and pre-verbal children.
Similar content being viewed by others
Introduction
Vision screening and eye examinations in infants and children are performed to detect conditions that can threaten vision. Amblyopia is the most common preventable and reversible condition that causes visual impairment, mainly monocular, in children [1], estimated to affect 1–3.6% of children [2,3,4,5,6,7]. It is a developmental disorder that leads to reduced vision when ocular images are either blurry or misaligned. It is caused by refractive errors, misalignment of the eyes or deprivation of vision in one or both eyes; the first two etiologies account for more than 90% of cases [2]. Amblyopia also leads to abnormal binocular vision and decreased depth perception and stereoacuity [8]. It can affect fine [4,5,6,7] and gross motor skills [9, 10] including balance [11,12,13], and visual-auditory speech integration [3].
Early detection of amblyopia using proper screening programs permits early intervention [12]. Current Public Health England (PHE) guidelines prepared with the National Screening Committee are to screen all children age 4 to 5 years in a school setting13: The UK National Screening Committee recommended in 2019 vision screening for all children aged 4 to 5 in a school setting, while the US Preventive Services Task Force (USPSTF) recommends screening of all children between the ages of 3 and 5 years at least once to detect the presence of amblyopia and amblyogenic risk factors [3]. Screening at younger ages is related to high false-positive rates, and has not been shown to be cost-effective [14].
Traditional vision screening is directed for visual acuity and the presence of amblyopia and is assessed by examining the child’s ability to recognize letters or symbols (optotypes). It is a challenging and an inaccurate test in illiterate children and unattainable in preverbal children. It is also time-consuming and generally requires dedicated skilled personnel. The US Preventive Services Task Force statement followed by the American academy of Pediatrics supported the use of vision screening technologies for preschool vision screening [3, 4].
Many instrument-based screening devices for vision screening aim to recognize risk factors of amblyopia, but do not evaluate directly for amblyopia and low vision by testing visual acuity. The first available instruments were the off-axis photoscreeners,which recognize abnormal patterns of light reflections caused by refractive error, strabismus, and cataract [5,6,7, 15]. Hand-held autorefractors can detect the refractive status of each eye separately without the ability to evaluate for strabismus [16, 17]. There are devices, which integrate the evaluation of refractive errors with either strabismus evaluation or photoscreening [5, 16], and lately a new scanner for the occurrence of strabismus and microstrabismus based on birefringence as an early sign for amblyopia was presented [18, 19].
The Eye-n-Joy (GreenCtech Ltd. Israel) is a new modality aimed to provide an alternative to the above-mentioned current vision screening in children. The Eye-n-joy (ENJ) device specifically addresses young pre-verbal children. It is mainly aimed to recognize children with amblyopia by evaluating for both ocular alignment and visual acuity.
The primary purpose of this pilot study was to evaluate the accuracy of the ENJ device in the assessment of visual impairment and the presence of amblyopia risk factors in verbal and preverbal children, aged 1.5 to 6 years, undergoing evaluation in a professional pediatric eye care setting. The secondary aim was to assess compliance.
Methods
Study design and settings
A prospective, single-center, comparison study recruiting children aged 1.5 to 6 years between March of 2018 to May of 2019.
The study took place at the Pediatric Ophthalmology Unit, Tel Aviv Medical Center. The study protocol was reviewed and approved by the IRB Ethics Committees of the participating medical centre (No. 0342-15TLV) in compliance with the Declaration of Helsinki. Written informed consent was obtained from parents of each patient, prior to enrollment in the study.
Participants
Children aged 1.5 to 6 years (18 to 72 months) who were referred to Tel Aviv Medical Center for an ophthalmic evaluation were recruited. Inclusion criteria included children aged 1.5 to 6 years old. Exclusion criteria included history of developmental delay or cognitive deficit, obvious ocular abnormalities warranting specialist referral, history of ocular surgery or any condition that would preclude the ability of the investigator to obtain a reliable measurement, and history of epilepsy or other neurological abnormalities. All participants underwent an exam by the ENJ and then a full pediatric ophthalmologist evaluation (reference examination). The ENJ and the reference examinations were performed by 2 independent testers in separate rooms, to maintain masking of the study’s test results. Both examinations were performed on the same day.
Eye-n-Joy™ device
The ENJ Device assessment was performed by a device technician. The child was positioned in front of a tablet, at a test distance of 55 cm for children younger than 3 years and 84 cm for children >3 years old, wearing the system’s child-friendly glasses and watching a video displayed on the tablet’s screen for 1 min. For details about the ENJTM device program and structure please look at Appendix 1 as well as Figs. 1–4.
a, b Left eye is covered. Right eye fixates, left eye does not move. c, d Right eye is covered. Both eyes do not change position. Eye tracking is demonstrated by a gradual change in color of the fixating dots from blue to red with time. Each figure represents 2 s of tracking. Both axes values are in Pixels. 40 pixels = 1 PD. X-axis represents horizontal fixation movement and Y-axis represents vertical fixation movement. (color figure online).
a, b Left eye is covered. Right eye fixates, left eye drifts to exotropic position. c, d Right eye is covered. Left eye fixates and right eye drifts to exotropic position. Eye tracking is demonstrated by a gradual change in color of the fixating dots from blue to red with time. Each figure represents 2 s of tracking. Both axes values are in Pixels. 40 pixels = 1 PD. X-axis represents horizontal fixation movement and Y-axis represents vertical fixation movement. (color figure online).
a, b Left eye is covered. Right eye fixates by moving down, left eye drifts down under the cover. c, d Right eye is covered. Left eye fixates by moving up and right eye drifts up under the cover. Eye tracking is demonstrated by a gradual change in color of the fixating dots from blue to red with time. Each figure represents 2 s of tracking. Both axes values are in Pixels. 40 pixels = 1 PD. X-axis represents horizontal fixation movement and Y-axis represents vertical fixation movement. (color figure online).
Data source and measurement variables
After fulfilling the ENJTM examination, all children completed a reference examination, which included a comprehensive ophthalmological examination performed by pediatric ophthalmologists and orthoptists and comprised the following: (i) Evaluation of visual acuity according to the child’s ability; Snellen chart or LEA symbols were used for verbal children, preverbal children were examined by Teller Acuity Cards, if cooperation was poor CSM method was used (ii) Pupillary reaction to light test (iii) Alignment evaluation including cover tests (iv) Stereoacuity using the Randot test for children older than 3 years (v) Cycloplegic refraction examination by handheld retinoscope performed 40 min after cyclopentolate 1% drops were administered twice, 5 min apart (vi) Fundus examination. All prescriptions and recommendations were based solely on the reference examinations.
The primary endpoint of the study was defined as visual acuity measurements determined by the ENJ device and the visual acuity measurements determined by the conventional, manual ophthalmic test method using the Teller Acuity Cards, LEA symbols, or Snellen optotypes, depends on patients age.
The secondary endpoint of the study was the determination of the presence of amblyopic risk factors using the ENJ device compared to conventional, manual ophthalmic test methods including strabismus evaluation and cycloplegic refraction examination.
Testability of the ENJ device in children was evaluated by assessing whether the children were able to complete the ENJ examination.
We set criteria for referral for the ENJ device based on American Academy of Ophthalmology recommendations [20] as detailed in Supplementary Table 1. We used the same VA and alignment criteria as well as amblyogenic refractive error in the reference exam to find correspondence between the ENJ and gold standard exams and to assess for sensitivity and specificity of the ENJ device to detect amblyopia.
Statistics
Data were recorded in Microsoft Excel and analysed using SPSS version 25 (SPSS Inc., Chicago, IL, USA). Continuous variables such as age were compared within subjects using the paired sample t-test. Binary variables were tabulated. Sensitivity, specificity, and overall agreement were also calculated, and variables were compared within subjects using the McNemar test for symmetry. All tests were 2-tailed, and the threshold for statistical significance was defined as a p-value < 0.05.
Results
A total of 51 children were enrolled, 33 (64.7%) girls, aged 18–72 months (Median = 46 months/3.8 years). Supplementary Table 2 presents demographic data and findings in both ENJ and reference exam.
Fourteen (27.45%) of the children were preverbal. Seven of them (50%) cooperated with Teller VA exam while the rest were evaluated by CSM method only.
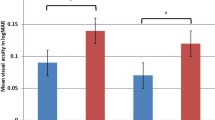
Mean measurable VA exam by the ENJ device in 44 of 51 patients was in the right eye (RE) 0.166 ± 0.14 LogMAR (equivalent to 20/29 Snellen) and in the left eye (LE) 0.155 ± 0.14 (equivalent to 20/29 Snellen). There were no significant differences between RE and LE. The corresponding value measured in the reference test were 0.133 ± 0.10 (equivalent to 20/27) and 0.124 ± 0.12 (equivalent to 20/27), respectively. no significant difference between the ENJ and the reference exams (Pv = 0.553 and 0.803, respectively).
Seven patients (15.9%) needed a referral for further investigation due to suspected amblyopia attributable to reduced visual acuity (VA) on the ENJ test. We compared VA referral criteria of the ENJ and VA result in the reference examination. Overall agreement was 90.9%, sensitivity was 75% and specificity was 90.0% (Table 1a).
Six patients (11.8%) needed a referral for a specialist’s evaluation due to suspected strabismus on the ENJ test while the reference exam revealed 2 patients (3.9%) with clinically significant strabismus. The alignment referral criteria of the ENJ compared to the reference examination, revealed an overall agreement of 90.1%, with a sensitivity of 66.6% and specificity of 91.6% (Table 1b).
According to the cycloplegic refraction in the reference exam evaluation; Mean spherical equivalent (SE) was +1.25 (±1.02) and +1.29 (±1.08) in RE and LE, correspondingly. Mean astigmatic error was 0.36 (±0.52) and 0.28 (±0.44) in RE and LE, correspondingly. Amblyogenic refractive error was found in 2 patients (patient 21 had amblyogenic anisometropia and patient 40 had high hyperopic refractive error).
As the ENJ does not examine refraction we observed if these patients were eventually referred due to other reasons. Patients 21 had an exceedingly small esotropia on the ENJ test that led to the referral. Patient 40 met both vision and alignment criteria for referral by the ENJ.
Overall comparison of all referral indications between the ENJ and reference examination including the cycloplegic refraction showed agreement was 86.3%, sensitivity was 83.3% and specificity was 86.7% (Table 1c).
We looked in details in all cases (n = 7), in which there was no accordance between the two tests.
Patient 12 was almost 6 years old when taking the test and was referred by the ENJ due to reduced VA in the left eye. In the reference test VA was within normal limits as the rest of the examination. Patient 20 had normal vision on the ENJ test but had VA of 20/30 in the RE at the age of 6, which was defined as suspected amblyopia. Cycloplegic refraction revealed astigmatism of 1.25D in that eye, which explained the difference.
Patient 10 had worse VA in the RE compared to the LE in both exams. However, the difference between the eyes reached the referral criteria in the ENJ and not in the reference exam.
There were patients who received a recommendation for further follow-up or a prescription of glasses. For example, Patient number 2 passed the ENJ screening test. In the reference test, the patient had a difference in VA of 1 line with a corresponding difference in cycloplegic refractive error of 0.75D, therefore, we prescribed glasses and recommended follow-up in 6 months. However, the patient did not meet the criteria for amblyopia. Another example is patient 9, whose cycloplegic refraction was plano at an age of 28 months, therefore follow-up for the development of myopia was recommended. Patient 51 was diagnosed with Duane syndrome in the reference test. She did not have abnormal head position or strabismus and the ENJ exam was considered normal.
Patient 23 was found to have inferior oblique overaction and DVD on the reference test. Eye-N-Joy test found esodeviation in this case.
There were 13 patients that were not found to be amblyopic or have significant amblyogenic risk factors on the reference test but were prescribed glasses or were recommended to be followed-up by a physician within one year due to hyperopia, astigmatism, tendency toward myopia, or mild myopia. Only one patient (patient number 10) was referred due to amblyopic risk factors by the ENJ because of two lines of difference between the two eyes in VA.
Discussion
Improved vision screening strategies for amblyopia are necessary to allow for early intervention to reduce the burden of the disease and to decrease long-term visual disabilities. Traditional vision screening using optotypes may be inaccurate or extremely limited in Illiterate and preverbal children leading to a high rate of false-positive tests and waste of public resources [14]. The need for highly professional personnel such as ophthalmologists or orthoptists limits its accessibility and inflates the cost of such screening making it not cost-effective as a screening tool [14].
The aim of our study was to evaluate the reliability of the Eye-n-Joy (GreenCtech Ltd. Israel) a novel screening device, in detecting both visual acuity and ocular alignment. Other screening devices mainly rely on early recognition of risk factors of amblyopia and do not necessarily evaluate vision. With this new tool, amblyopia can be assessed directly by screening for vision in preverbal children.
Though this was a preliminary and relatively small study, cooperation was observed to be excellent. The ENJ is very friendly, the test is accompanied by pleasant music and cute pictures that make children pay attention. The exam took less than 60 s, and all participants were cooperative.
One of the main advantages of the ENJ is its ability to evaluate VA in young children. Comparing VA between the reference test and the ENJ showed no statistical difference. All 7 preverbal children, who did not cooperate with the Teller cards were all able to sit in front of the screen and get examined by the ENJ. (Fig. 4).
The ENJ is extremely sensitive in the evaluation of ocular misalignment. It did not miss any case of strabismus in primary position according to the reference test.
There is a consensus among pediatric ophthalmologists about the importance of amblyopia screening at a young age. While most devices look for risk factors of amblyopia including refractive errors, anisometropia and strabismus, the ENJ looks directly at both the VA which is the essence of amblyopia and strabismus, which is measured by alternate cover test (Figs. 1–3) and is a major cause for amblyopia.
ENJ is fast, efficient, and reliable and its data is repeatable and can be easily applied by unskilled technicians. But unfortunately, there are certain drawbacks to its use; it cannot test for abnormal eye movements, such as deficient ductions in Duane’s syndrome (patient 50) or refractive errors that may lead to amblyopia in the future (Case 2). Therefore, we believe that children who pass the test should be screened on a yearly basis, as opposed to children who pass a full comprehensive examination by skilled personnel including cycloplegic refraction that is found to be normal.
This study has some limitations. Though sample size was relatively large, the efficacy of this device would have been better demonstrated with a larger and a more diverse group of patients. The device would have been better validated across different populations and pathologies. Unfortunately, the instrument was withdrawn from the study by the owner due to financial reasons. Furthermore, the device was examined only in comparison to the gold standard of a skilled personnel’s examination including cycloplegic refraction, and was not assessed in contrast to other screening devices.
Further research is necessary to fully understand the ENJ ability to detect amblyopia in comparison to other available devices.
In conclusion, the Eye-N-Joy is a reliable and easy-to-use device that can assist in the screening of amblyopia and strabismus in both verbal and pre-verbal children.
Summary
What was known before
-
Instrument based vision screening for high refractive error and amblyopia is recommended for infants and children aged 1–5 years visual acuity examination is challenging and inaccurate in illiterate and preverbal children.
What this study adds
-
The Eye-n-Joy is a new device aimed to screen for amblyopia risk factors by combining both visual acuity and alignment evaluation The Eye-n-joy is a reliable and easy-to-use device for the screening of amblyopia and strabismus in both verbal and pre-verbal children.
References
Wu C, Hunter DG. Amblyopia: diagnostic and therapeutic options. Am J Ophthalmol. 2006;141:175–84.
Gunton KB. Advances in amblyopia: what have we learned from PEDIG trials?. Pediatrics. 2014;131:540–7.
Village G. Vision screening for children 1 to 5 years of age: US preventive services task force recommendation statement. Pediatrics. 2011;127:340–6.
Donahue SP, Nixon CN. Visual System Assessment in Infants, Children, and Young Adults by Pediatricians. Pediatrics. 2016;137:28–30.
Arnold RW, Miller JM. Vision in Preschoolers Study [1] (multiple letters). Ophthalmology. 2004;111:2313–5.
Kirk VG, Clausen MM, Armitage MD, Arnold RW. Preverbal photoscreening for amblyogenic factors and outcomes in amblyopia treatment: early objective screening and visual acuities. Arch Ophthalmol. 2008;126:489–92.
Teed RG, Bui CM, Morrison DG, Estes RL, Donahue SP. Amblyopia therapy in children identified by photoscreening. Ophthalmology. 2010;117:159–62.
Jeon HS, Choi DG. Stereopsis and fusion in anisometropia according to the presence of amblyopia. Graefe’s Arch Clin Exp Ophthalmol. 2017;117:159–62.
Buckley JG, Panesar GK, MacLellan MJ, Pacey IE, Barrett BT. Changes to control of adaptive gait in individuals with long-standing reduced stereoacuity. Investig Ophthalmol Vis Sci. 2010;51:2487–95.
Engel-Yeger B. Evaluation of gross motor abilities and self perception in children with amblyopia. Disabil Rehabil. 2008;30:243–8.
Zipori AB, Colpa L, Wong AMF, Cushing SL, Gordon KA. Postural stability and visual impairment: assessing balance in children with strabismus and amblyopia. PLoS One. 2018;13:0205857.
Garretty T. Final visual outcomes and treatment received for children referred from a UK primary school visual screening program: a comparison of an orthoptic-led program with orthoptic-delivered services. Strabismus. 2017;25:184–90.
Solebo AL, Rahi JS Childhood vision screening. External review against programme appraisal criteria for the UK National Screening Committee. Version: Final (2019).
Solebo, Ameenat Lola, Phillippa M. Cumberland, Jugnoo S. Rahi. Whole-population vision screening in children aged 4–5 years to detect amblyopia. Lancet. 2015;385:2308–19.
Lempert P. Amblyopia and photoscreening. Ophthalmology. 2010;117:1661.
De Juan V, Sanchez I, Ortiz-Toquero S, Martin R Advantages, limitations, and diagnostic accuracy of photoscreeners in early detection of Amblyopia: a review. Clin Ophthalmol Volume 10, 2016.
Ruben JB, Granet DB, Blocker RJ, Bradford GE, Karr DJ, Lueder GT, et al. Instrument-based pediatric vision screening policy statement. Pediatrics. 2012;130:983–6.
Loudon SE, Rook CA, Nassif DS, Piskun NV, Hunter DG. Rapid, high-accuracy detection of strabismus and amblyopia using the pediatric vision scanner. Investig Ophthalmol Vis Sci. 2011;52:5043–8.
Jost RM, Stager D, Dao L, Katz S, McDonald R, Birch EE High specificity of the Pediatric Vision Scanner in a private pediatric primary care setting Presented in part as a poster 41st Annual Meeting of the American Association for Pediatric Ophthalmology and Strabismus, New Orleans, Louisiana, March 25–29, 201. J AAPOS 19, 521-5 (2015).
Wallace DK, Morse CL, Melia M, Sprunger DT, Repka MX, Lee KA, et al. Pediatric Eye Evaluations Preferred Practice Pattern®: I. Vision screening in the primary care and community setting; II. Comprehensive ophthalmic examination. Ophthalmology. 2018;125:184–227.
Acknowledgements
The hospital was financially compensated for this project, The study investigators did not receive any financial nor other incentives. The company or the hospital did not have access to the data and did not review the paper.
Author information
Authors and Affiliations
Contributions
All authors collected the data. DMH,ABZ and CS designed the study. NG, AR and DMH made the statistical analysis. NG, AR, ABZ and DMH wrote the paper. All authors have authorized the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Rosenblatt, A., Stolovitch, C., Gomel, N. et al. A novel device for assessment of amblyopic risk factors in preverbal and verbal children–a pilot study. Eye 36, 2312–2317 (2022). https://doi.org/10.1038/s41433-021-01860-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01860-z