Abstract
Introduction
Ophthalmic simulation is cost-effective in complication prevention. However, there is no consistent resource allocation to provide the necessary time and finance to sustain such activities. We wished to identify the current support for the regional Simulation Leads in the UK.
Methods
An online SurveyMonkey questionnaire was sent to all 26 UK ophthalmic regional Simulation Leads in February 2021 regarding current simulation activity and the degree of time and resource support available.
Results
There were 22 responses within 1 month (84.6% response rate). 72.7% run regular simulation induction events for new trainees. 60% run mandatory laser simulation events. 38.1% run immersive simulation (vitreous loss fire drill). 47.6% run yearly sub-specialty events. 45.5% were required to make additional work arrangements to run simulation events. 77.3% had no job plan time allocation for simulation. 59.1% dedicated >1 hr/week to simulation. 68.2% EYESI simulators were purchased via charity/endowments. 72.7% had access to dedicated dry lab simulation (40.9% wet lab). 40.9% used deanery funds to purchase initial model eyes (supplemented by charity (36.4%) and endowments (31.8%)). 65% used unspent study leave budgets for ongoing model eyes, yet 15% reported trainees purchasing their own.
Conclusion
Nearly all ophthalmic simulation in the UK is undertaken via goodwill and personal commitment to excellence by the regional Simulation Leads. There is minimal allowance of time or finance for these vital activities, which is sporadic at best, and unsustainable. We call for the necessary investment and dedicated time allocation to permit ophthalmic simulation to be supported and maintained.
Similar content being viewed by others
Introduction
The awareness that simulation provides safer surgical experiences is increasingly being recognised and expanded in ophthalmic training [1]. There are a range of publications demonstrating objective improvement in surgical competency following the use of modular virtual reality simulation, such as the EYESI simulator (Haag-Streit) [2,3,4,5]. Accompanied with greater use of bespoke model practice eyes, straight-forward techniques and complex surgical scenarios can be simulated and practiced prior to encountering them intra-operatively [6]. These can be used repeatedly to keep costs down and skills up [6]. Immersive situational simulation has been shown to improve confidence in dealing with stressful scenarios such as posterior capsule rupture causing vitreous loss, and alternative 3-piece IOL insertion [7,8,9,10,11].
Challenges to widespread ophthalmic simulation engagement have included the accusation that it is too expensive, and not truly representative of intra-ocular surgery [1, 12]. However, it is being increasingly acknowledged that the true costs of surgical complications are significantly under-appreciated [13]. Use of the EYESI simulator by junior ophthalmology trainees has been shown to be cost-effective through cataract complication prevention [14]. It has also been noteworthy that engagement with ophthalmic simulation increased and has been maintained following suspension of surgical activities during COVID lockdowns [15]. To this end, the Royal College of Ophthalmologists has developed a network of voluntary regional Simulation Leads to establish and deliver simulation activities through sharing best practices and resources. Some of this activity is mandatory for new trainees (induction courses, introduction to surgical skills, Modules A and B on the EYESI), but most other educational opportunities are optional, and their success is reliant on local engagement. In 2019 the Training Committee set a goal for simulation workshops or courses to be delivered annually in every region by 2021 for both common laser treatments and managing vitreous loss in cataract surgery. The levels of local infrastructure support are highly variable on a regional basis and can be sporadic at best. There is currently no consistent resource allocation to provide the necessary time and finance to sustain these activities.
In light of this, we wished to identify the current level of support available to the regional Simulation Leads to deliver ophthalmic simulation in 2021 in the UK.
Methods
On behalf of the Royal College of Ophthalmologists, an online SurveyMonkey questionnaire was sent to all 26 ophthalmic regional Simulation Leads in the UK in February 2021. Questions were designed to identify current simulation practice within their regions, and how these activities were resourced. Respondents were asked about time commitment to run these informal and formal activities, including if they had dedicated time allocated in their job plans to devote to simulation. They were also asked about the finances required for setting up simulation and the ongoing material costs, including where the funding support originated. Free text responses and comments regarding the current setup were encouraged at the conclusion of the survey.
Results
There were 22 responses within 1 month (84.6% response rate), though not every question was answered fully by all. 59.2% (13/22) of the Simulation Leads reported a sub-specialty interest in cataract surgery (7/22 motility, 6/22 paediatrics, 5/22 vitreo-retinal). Only 9.1% (2/22) reported not actively performing regular cataract surgeries in the preceding year, indicating that most regional Simulation Leads are surgically active ophthalmologists (1 respondent has a dedicated simulation role alone).
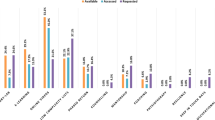
Regarding activity, 72.7% (16/22) ran regular simulation induction events for new trainees on at least a yearly basis (rather than on a sporadic basis). Only 3 Simulation Leads reported not using simulation activities during their induction programmes. 60% (12/20) ran mandatory laser simulation events each year. 38.1% (8/21) ran a vitreous loss fire drill (immersive simulation to surgical complication management) in the past year. Regional sub-specialty events included surgical complications (68.2%; 15/22), Oculoplastics (63.6%; 14/22), Glaucoma (54.5%; 12/22), Cornea (45.5%; 10/22) and Strabismus (31.8%; 7/22). 47.6% (10/21) run such sub-specialty events on a yearly basis. 42.9% (9/21) have run communication skills workshops (situational simulation) in the past.
Regarding time and employment support, 45.5% (10/22) were required to make alternative work arrangements to run simulation events and 77.3% (17/22) had no dedicated simulation time allocation in their job plans (2 had 0.25PA or less/week, 1 had 0.5PA/week). 13/22 reported that they regularly dedicated >1 h/week to simulation training (9 committed 1 h/week, 7 committed 2 h/week, 2 committed 3 h/week, 2 committed 4 h/week). 81.8% (18/22) had no knowledge of any of their ophthalmic colleagues in their deanery having any dedicated time for simulation in their job plans. 77.3% (17/22) had identified local trainees who were actively supporting simulation activities in their region. 90.9% (20/22) felt having a regional trainee simulation champion role would help develop simulation engagement in their setting.
Regarding access, 72.7% (16/22) had access to dedicated dry lab simulation set-ups (40.9% (9/22) had access to a wet lab environment). All respondents reported access to at least one EYESI simulator (12/22 had one (54.5%), 4/22 had 2 (18.2%), 4/22 had 3 (18.2%), 2/22 had 4 (9.1%), and there were reported plans to purchase additional simulators in time). The oldest simulators were reported to be >8 years old in 13 cases (59.1%). 40.9% (9/22) reported their EYESI simulators did not have a service plan or warranty. 18.2% (4/22) reported they did not have direct access to model eyes.
Regarding costs, 68.2% (15/22) EYESI simulators had originally been purchased via charity/endowments. 40.9% (9/22) had used deanery funds to purchase initial model eyes (with additional financial support in 36.4% (8/22) from charity and 31.8% (7/22) from endowment funds). Ongoing equipment supplies were financed by 65% (13/20) regions accessing unspent study leave budgets from the local Deanery. 15% (3/20) reported that in their region, trainees were buying their own simulation model eyes, and 15% (3/20) reported they did not have any model eyes for practice as there was no agreed funding for them.
In the free-text comments regarding the sustainability of this current climate regarding cost and time allocations for simulation, recurring themes included the need and requirement for a simulation budget (76.5%; 13/17), frustration about the lack of dedicated time to do the job properly (58.8%; 10/17), and that the current situation is unsustainable without appropriate resourcing (41.2%; 7/17).
Discussion
This is the first national survey of regional Simulation Leads in the UK. We have identified a significant commitment to simulation activity from the respondents. Regular activities included induction and orientation, laser safety and techniques, with a range of immersive and situational simulation such as communication skills and complication management [See Table 1].
However, all these activities require a time commitment to be planned, resourced and delivered. Aside from 1 respondent who had a simulation-only role, there was minimal dedicated time in any of the simulation leads’ job plans. It is a testimony to the professionalism and commitment of these individuals that they give up so much of their time to teaching the surgeons of tomorrow. Relying on goodwill alone may not be sustainable in the longer term, as was mentioned in the free-text comments.
The benefits of running regular simulation training for surgical scenario events such as a vitreous loss fire drill have been previously described, all with a view to improving confidence through maintaining competence [10, 16]. These safety-first principles apply to both the new trainee and the established consultant, as reduced complication rates can limit all theatre staff’s exposure to the management of uncommon, yet predictable surgical scenarios [10]. Simulation training can maintain familiarity with techniques prior to their use, and then lead to greater confidence in utilising them as required [11].
There appears to be good access across the UK to virtual reality simulation equipment such as the EYESI cataract simulators. This is probably reflective that the basic modules are mandatory prior to engaging in real-life ocular surgery, and therefore the regions have had to find ways to purchase this equipment. However, there was evidence that charitable, endowment or external funding sources provided the majority of funding for this expensive, yet essential kit. As these items require software updates and are out of warranty in many cases, a plan is required to address the future financial requirement to maintain and sustain an item that is now integrated into ophthalmic training.
While there was a range of sub-specialty courses being run using the expanding options of bespoke model simulation eyes, several regions had no direct finance to equip their dry lab facilities. Again, one-off charitable donations were meeting the gap in funding, as were unspent study leave budgets due to suspension of educational events in the COVID pandemic. These ad-hoc funding sources cannot be relied upon to maintain and sustain this form of simulation training.
It was concerning to note that 3 regional Simulation Leads (15%) reported no direct access to a supply of model eyes for simulation, and that their trainees were subsequently purchasing their own resources. This lack of support could serve to discourage trainees from working in these regions, as such hidden costs to training have been shown to be significantly under-reported and can lead to inadequate study leave budget calculations and inaccurate assumptions going forward [17].
Modern ophthalmic simulation has been demonstrated to being cost effective and patient saving in the avoidance of surgical complications, providing a safer surgical experience for the trainee, trainer and the patient (most importantly) [14, 15]. In light of the findings of this survey, and the educational culture disruption following the COVID pandemic, we believe that we can no longer afford to not invest in ophthalmic simulation [1, 15].
Conclusion
Nearly all ophthalmic simulation in the UK in 2021 is undertaken via goodwill and personal commitment to excellence in education by the regional Simulation Leads. There is minimal allowance of time or finance for these vital activities, which is sporadic at best, and unsustainable. We join calls for the necessary investment and dedicated time allocation to permit ophthalmic simulation to be supported and maintained.
Summary
What was known before
-
Ophthalmic simulation is cost-effective in complication prevention. There is no consistent resource allocation to provide the necessary time and finance to sustain such activities.
What this study adds
-
Nearly all ophthalmic simulation in the UK is undertaken via goodwill and personal commitment to excellence by the regional Simulation Leads. There is minimal allowance of time or finance for these vital activities, which is sporadic at best, and unsustainable. We call for the necessary investment and dedicated time allocation to permit ophthalmic simulation to be supported and maintained.
References
Chilibeck CM, McGhee CNJ. Virtual reality surgical simulators in ophthalmology: are we nearly there? Clin Exp Ophthalmol. 2020;48:727–9. https://doi.org/10.1111/ceo.13784. AugEpub 2020 Jun 2. PMID: 32488961.
Dean WH, Gichuhi S, Buchan JC, Makupa W, Mukome A, Otiti-Sengeri J, et al. Intense simulation-based surgical education for manual small-incision cataract surgery: the ophthalmic learning and improvement initiative in cataract surgery randomized clinical trial in Kenya, Tanzania, Uganda, and Zimbabwe. JAMA Ophthalmol. 2021;139:9–15. https://doi.org/10.1001/jamaophthalmol.2020.4718. Jan 1PMID: 33151321; PMCID: PMC7645744.
Lee R, Raison N, Lau WY, Aydin A, Dasgupta P, Ahmed K, et al. A systematic review of simulation-based training tools for technical and non-technical skills in ophthalmology. Eye. 2020;34:1737–59. https://doi.org/10.1038/s41433-020-0832-1. OctEpub 2020 Mar 13. PMID: 32203241; PMCID: PMC7609318.
Jacobsen MF, Konge L, Bach-Holm D, la Cour M, Holm L, Højgaard-Olsen K, et al. Correlation of virtual reality performance with real-life cataract surgery performance. J Cataract Refract Surg. 2019;45:1246–51. https://doi.org/10.1016/j.jcrs.2019.04.007. SepEpub 2019 Jul 29. PMID: 31371151.
Thomsen AS, Bach-Holm D, Kjærbo H, Højgaard-Olsen K, Subhi Y, Saleh GM, et al. Operating room performance improves after proficiency-based virtual reality cataract surgery training. Ophthalmology. 2017;124:524–31. https://doi.org/10.1016/j.ophtha.2016.11.015. AprEpub 2016 Dec 22. PMID: 28017423.
Hind J, Edington M, Lockington D. Maximising cost-effectiveness and minimizing waste in modern ocular surgical simulation. Eye. 2020:1–2. https://doi.org/10.1038/s41433-020-01155-9. Epub ahead of print. PMID: 32843746; PMCID: PMC7446602.
Mulholland C, Lockington D. Trainee experience with capsular tension rings in Scotland-the need for structured simulation exposure to surgical adjuncts. Eye. 2020;34:1497–8. https://doi.org/10.1038/s41433-020-0856-6. SepEpub 2020 Apr 7. PMID: 32265512; PMCID: PMC7608384.
Guthrie S, Goudie C, Lockington D. Survey of Scottish ophthalmic trainees’ experiences using 3-piece IOLs in cataract surgery. J Cataract Refract Surg. 2018;44:409 https://doi.org/10.1016/j.jcrs.2018.01.016. MarPMID: 29703295.
Brogan K, Dawar B, Lockington D, Ramaesh K. Intraoperative head drift and eye movement: two under addressed challenges during cataract surgery. Eye. 2018;32:1111–6. https://doi.org/10.1038/s41433-018-0047-x. JunEpub 2018 Feb 21. PMID: 29463862; PMCID: PMC5997653.
Lockington D, Belin M, McGhee CNJ. The need for all cataract surgeons to run a regular vitreous loss fire drill. Eye. 2017;31:1120–1. https://doi.org/10.1038/eye.2017.58. AugEpub 2017 Apr 7. PMID: 28387763; PMCID: PMC5558226.
Saleh GM, Wawrzynski JR, Saha K, Smith P, Flanagan D, Hingorani M, et al. Feasibility of human factors immersive simulation training in ophthalmology: the London pilot. JAMA Ophthalmol. 2016;134:905–11. https://doi.org/10.1001/jamaophthalmol.2016.1769. Aug 1PMID: 27310034.
la Cour M, Thomsen ASS, Alberti M, Konge L. Simulators in the training of surgeons: is it worth the investment in money and time? 2018 Jules Gonin lecture of the Retina Research Foundation. Graefes Arch Clin Exp Ophthalmol. 2019;257:877–81. https://doi.org/10.1007/s00417-019-04244-y. MayEpub 2019 Jan 15. PMID: 30648208.
Jamison A, Benjamin L, Lockington D. Quantifying the real-world cost saving from using surgical adjuncts to prevent complications during cataract surgery. Eye. 2018;32:1530–6. https://doi.org/10.1038/s41433-018-0133-0. SepEpub 2018 Jun 6. PMID: 29875386; PMCID: PMC6137160.
Ferris JD, Donachie PH, Johnston RL, Barnes B, Olaitan M, Sparrow JM. Royal College of Ophthalmologists’ National Ophthalmology Database study of cataract surgery: report 6. The impact of EyeSi virtual reality training on complications rates of cataract surgery performed by first and second-year trainees. Br J Ophthalmol. 2020;104:324–9. https://doi.org/10.1136/bjophthalmol-2018-313817. MarEpub 2019 May 29. PMID: 31142463.
Campbell S, Hind J, Lockington D. Engagement with ophthalmic simulation training has increased following COVID-19 disruption-the educational culture change required? Eye. 2021:1–2. https://doi.org/10.1038/s41433-021-01494-1. Epub ahead of print. PMID: 33707763; PMCID: PMC7947940.
Nairn J, Benjamin L, Lockington D. Comment on: ‘Ophthalmology Specialist Trainee Survey in the United Kingdom’. The need to increase familiarity with the management of predictable cataract surgery complications via simulation-ensuring competence to improve confidence. Eye. 2020;34:1713–4. https://doi.org/10.1038/s41433-019-0673-y. SepEpub 2019 Nov 21. PMID: 31754281; PMCID: PMC7608225.
Nairn J, Ferris J, Lockington D. The hidden financial hurdles of commitment to Ophthalmology in the current UK training system. Eye. 2020;34:984–5. https://doi.org/10.1038/s41433-019-0619-4. MayEpub 2019 Oct 4. PMID: 31586166; PMCID: PMC7182574.
Acknowledgements
We wish to thank all the regional Simulation Leads for their commitment to excellence in training and acknowledge those who responded and raised the issues contained in this article. The contributors were: Imran Ashfaq (North East), Richard Best (Northern Ireland), Kate Bush (Wessex), Tom Butler (East Anglia), James Deane (East Midlands South), Chrys Dimitriou (East Anglia), Tim de Klerk (Northwest), John Ferris (Severn), Simon Hewick (Scotland North), Jim Innes (Yorkshire), Saurabh Jain (London), David Lockington (West of Scotland), Arijit Mitra (West Midlands), Balasubramanian Ramasamy (Mersey/Northwest), George Saleh (London), Eulee Seow (Wales), Tamsin Sleep (Peninsula), John Somner (East of England), Richard Stead (East Midlands North), Sonali Tarafdar (Scotland East), Naing Tint (South East of Scotland), Martin Wasik (Thames Valley).
Author information
Authors and Affiliations
Contributions
DL and GS had the original idea, performed the survey and drafted the article. AFS and JF revised the paper and provided additional support. All authors reviewed and agreed to the final article.
Corresponding author
Ethics declarations
Competing interests
None to report. George M Saleh’s contribution was part-funded by the National Institute for Health Research (NIHR), Biomedical Research Centre based at Moorfields Eye Hospital, NHS Foundation Trust and UCL Institute of Ophthalmology. The views expressed here are those of the authors and not necessarily those of the Department of Health.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lockington, D., Saleh, G.M., Spencer, A.F. et al. Cost and time resourcing for ophthalmic simulation in the UK: a Royal College of Ophthalmologists’ National Survey of regional Simulation Leads in 2021. Eye 36, 1973–1976 (2022). https://doi.org/10.1038/s41433-021-01796-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01796-4
This article is cited by
-
Time requirements for mandatory cataract simulation modules
Eye (2024)
-
Simulation-based training for intraoperative posterior capsule rupture management: an analysis of nontechnical skills development and the relationship between technical and nontechnical skills
Eye (2024)
-
Creation of a proof-of-concept 3D printed corneal trauma simulation model
Eye (2023)
-
Attitudes of ophthalmic trainees in Scotland towards surgical simulation engagement
Eye (2023)
-
A pilot project evaluation of a novel heads-up viewing system compared to desktop microscopes commonly used for ophthalmic simulation
Eye (2023)