Abstract
Objectives
To investigate the threshold thickness of the foveal outer nuclear layer (ONL) associated with favourable visual outcome after half-dose photodynamic therapy (PDT) in patients with central serous chorioretinopathy (CSC).
Methods
The CSC patients were divided into two groups according to whether their best-corrected visual acuity (BCVA) at 1 year after half-dose PDT was 20/20 or worse than 20/20. Three multivariable logistic regression models were respectively created to determine the prognostic value of the pre-PDT foveal ONL thickness, the pre- and the post-PDT foveal ONL thickness ratio, which was defined as the foveal ONL thickness in the CSC eye to that in the normal contralateral eye, for predicting the outcome of half-dose PDT. The areas under the receiver operating characteristic curves (AUCs) were compared and the best cut-off values were determined, respectively.
Results
Totally, 134 patients were included. The pre-PDT foveal ONL thickness, the pre-PDT and the post-PDT foveal ONL thickness ratios were all independent predictors of the outcome after half-dose PDT in their respective model (all P < 0.05). The AUC of the post-PDT foveal ONL thickness ratio was significantly higher than the AUCs of the other two parameters (0.940 vs 0.840 and 0.882, DeLong test: both P < 0.05), with the cut-off value of 0.81.
Conclusions
The threshold of the foveal ONL thickness ratio is 0.81. Active CSC eyes with a foveal ONL thickness ratio of 0.81 or more could probably retain BCVA of 20/20 after half-dose PDT. They were considered reasonable to wait for spontaneous resolution of sub-retinal fluid.
Similar content being viewed by others
Introduction
Central serous chorioretinopathy (CSC) is a common macular disease and often presents as well-circumscribed serous retinal detachment in the macular region on clinical examination and with one or several points of leakage at the level of the retinal pigment epithelium (RPE) detectable with fluorescein angiography (FA) [1]. The natural course of acute CSC is usually considered a self-limiting process, with a promising visual prognosis. However, chronic CSC may result in a loss of vision, attributable to the cumulative death of photoreceptor cells as retinal detachment persists [2,3,4,5,6,7]. Photodynamic therapy (PDT) has been shown to be effective in promoting the resolution of the subretinal fluid [8,9,10,11,12,13,14], however, the visual outcome is worse in CSC eyes with thinner baseline foveal outer nuclear layer (ONL) [14, 15].
On the other hand, Matsumoto and Hata reported that some CSC eyes with relatively thin foveal ONL could still maintain favourable visual acuity [5, 16]. And, Hata further speculated that there may be a “threshold” of ONL thickness to retain some level of visual acuity [5].
To investigate the threshold of reduction in foveal ONL thickness associated with favourable visual outcome after PDT, the medical records of patients with CSC were reviewed in this study.
Materials and methods
This retrospective study was approved by the Ethics Committee of the Eye & Ear, Nose, Throat Hospital of Fudan University Shanghai China (2020052). The study adhered to the tenets of the Declaration of Helsinki. The medical records of CSC patients who received half-dose PDT in the clinic of our hospital between January 2012 and October 2019 were reviewed.
Patients
The clinical diagnosis of CSC was based on symptoms, reduced visual acuity with or without metamorphopsia or micropsia; the presence of serous retinal detachment on both fundus and optical coherence tomography (OCT) examinations; the presence of active angiographic leakage in FA (TRC-50IX; Topcon Corp., Tokyo, Japan); and/or abnormally dilated choroidal vasculature and other features in indocyanine green angiography (ICGA; Spectralis HRA + OCT; Heidelberg Engineering, Heidelberg, Germany) consistent with the diagnosis of CSC [17].
The patients included were those with clear and detailed medical records: one affected eye in the first episode of CSC and a normal contralateral eye (best-corrected visual acuity (BCVA) ≥ 20/20); no clinical signs or history of any other intraocular disease in either eye; no history of CSC or active CSC in the contralateral eye; no history of refractive surgery in either eye; no anisometropia (≤1 dioptre difference between bilateral eyes); accurately known symptom duration; subretinal fluid resolution within 2 months of half-dose PDT; no recurrence within 12 months of half-dose PDT.
The data were collected for both eyes, including BCVA, physical examination information, OCT examination and refraction data, which were converted to spherical equivalents (SEs), calculated as the spherical dioptric power plus one-half of the cylindrical dioptric power. The symptom duration and half-dose PDT spot diameter in each CSC eye were also collected.
Half-dose PDT protocol
The PDT protocol for CSC was performed using half the normal dose of verteporfin (Visudyne; Novartis AG, Bülach, Switzerland), that is, 3 mg/m2 verteporfin, with a rationale that using a lower dose has less severe collateral damaging effects to the retina and choroid. Verteporfin was infused over 8 min, followed by delivery of laser at 689 nm at 10 min from the commencement of infusion to target the area of choroidal dilation and hyperpermeability [8, 9] (Fig. 1A). The total light energy of 50 J/cm2 over 83 s was delivered to the angiographic leakage sites shown in FA or the area of choroidal hyperperfusion as observed in ICGA [8,9,10].
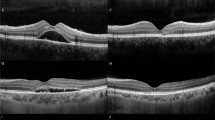
A ICGA showed dilated choroidal vasculature and hyperperfusion. The yellow circle represented the laser spot size of 2319 μm, used for half-dose PDT. B, C Foveal ONL thickness was defined as the distance between the internal limiting membrane and the external limiting membrane at the centre of the fovea. B Horizontal line scan of an eye with severe foveal ONL thinning (30 μm). C Horizontal line scan of an eye with minimal foveal ONL thinning (84 μm). All measurements were made manually using the supplied software, in 1:1 μm mode.
Optical coherence tomography protocol
All OCT images were obtained with a line scan protocol (line scans of 30°, composed of 100 averaged images; Heidelberg Spectralis OCT, Heidelberg Engineering, Heidelberg, Germany). For each patient’s scan, this protocol was applied both horizontally and vertically and centred on the fovea in both eyes. The OCT images that passed through the central fovea were selected for the measurement of the ONL thickness. OCT images were taken within 1 week before half-dose PDT, 2 months (±2 weeks) and 12 months (±2 weeks) after half-dose PDT were analysed [15].
Optical coherence tomography image analysis
The foveal ONL thickness was the average of the distance between the internal limiting membrane and the external limiting membrane at the centre of fovea measured from the horizontal and vertical images across the centre of fovea respectively [5, 14, 16, 18]. (Fig. 1B, C) The ratio of foveal ONL thickness was defined as the foveal ONL thickness in the CSC eye to that in the contralateral eye. The measurements were made manually using the supplied software (in 1:1 μm mode; HRA/Spectralis Viewing Module 6.0.9.0, Heidelberg Engineering).
For foveal ONL thickness measurements, both intra-observer repeatability and inter-observer reproducibility were evaluated on 25 normal eyes and 25 CSC eyes. YJ measured the same scan from each eye twice at an interval of 1 week to calculate the intra-observer repeatability. Inter-observer reproducibility was evaluated between YJ and JC, who measured the same scan independently. All the measurements of foveal ONL thickness were then made by YJ Intraclass correlation coefficients (ICCs) were used to assess the repeatability and reproducibility of the measurements [19].
The patients were divided into two groups according to their BCVA at 1 year after half-dose PDT as 20/20 (Group 1) or worse than 20/20 (Group 2).
Statistics analysis
Statistical analyses were performed using SPSS for Windows (version 21.0; SPSS; Chicago, IL, USA) and MedCalc Statistical Software (version 16.8.4; MedCalc; Ostend, Belgium). The calculated values are presented as either frequency (proportions), means ± standard deviations, or medians. The Kolmogorov–Smirnov test was used to confirm the normality of the data. Three multivariable logistic regression models were respectively created to determine the prognostic value of the foveal ONL thickness before PDT (Model 1), the foveal ONL thickness ratio before PDT (Model 2) and the foveal ONL thickness ratio after PDT (Model 3) for predicting the visual outcome at 1 year after half-dose PDT. The outcome of half-dose PDT was treated as a dichotomous variable (0 = Group 1 with BCVA of 20/20, 1 = Group 2 with BCVA lower than 20/20). Factors such as sex, age, symptom duration, BCVA before half-dose PDT, SEs of the CSC eye 1 year after half-dose PDT and half-dose PDT spot diameter were included in these multivariable models to adjust for potential confounding. The discriminative ability of each parameter was assessed with receiver operating characteristic (ROC) curves. For each parameter tested, the area under the ROC curve (AUC) was calculated and the best cut-off value that yielded the highest accuracy was determined, along with its sensitivity and specificity. The DeLong test was used to compare the AUCs [20]. A P value <0.05 was considered statistically significant.
Results
In total, 134 patients were enroled in the study. The demographic data for the patients were listed in Table 1. There were 96 (71.6%) patients in Group1, each of whom had a BCVA of 20/20 at 1 year after half-dose PDT. There were 38 (28.4%) patients in Group2, with a median BCVA of 20/26 (logMAR, 0.125; range, 0.1–2.0). The measurements of the foveal ONL thickness by Y.J. showed good intra-observer repeatability, with an ICC value of 0.980 for normal eyes and 0.990 for CSC eyes. The inter-observer reproducibility between Y.J. and J.C. was also satisfactory, with an ICC value of 0.986 for normal eyes and 0.992 for CSC eyes.
Table 2 showed that the foveal ONL thickness before PDT, the foveal ONL thickness ratio before PDT and the foveal ONL thickness ratio after PDT were all independent predictors of the visual outcome after half-dose PDT in their respective model, even after adjustment for baseline clinical characteristics, such as sex, age, symptom duration, BCVA before half-dose PDT, SEs of the CSC eye 1 year after half-dose PDT, and half-dose PDT spot diameter (Table 2; all P < 0.05). The eyes with greater values of these foveal ONL thickness parameters were less likely to have unfavourable visual outcomes after PDT (Fig. 2 and Table 2; each adjusted odd ratio <1: 0.917, 0.000, and 0.000, respectively).
A–C Vertical line scans of a 45-year-old male patient with best-corrected visual acuity (BCVA) of 20/32 and symptom duration of 70 days before half-dose PDT, and BCVA of 20/20 at 12 months after PDT. His foveal ONL thicknesses before PDT and at 12 months after PDT were 61 μm and 83 μm, respectively. The increase in foveal ONL thickness was 22 μm, attributable to retinal stretch recovery. A, B The foveal ONL thickness of his normal contralateral eye was 87 μm (C). The foveal ONL thickness ratios before PDT and after PDT were 0.70 and 0.95, respectively. D–F Vertical line scans of a 42-year-old male patient with BCVA of 20/40 and symptom duration of 43 days before half-dose PDT, and BCVA of 20/25 at 12 months after PDT. His foveal ONL thicknesses before PDT and at 12 months after PDT were 60 μm and 62 μm, respectively. The increase in foveal ONL thickness was 2 μm, attributable to retinal stretch recovery. D, E The foveal ONL thickness of his normal contralateral eye was 110 μm (F). The foveal ONL thickness ratios before PDT and after PDT were 0.55 and 0.56, respectively.
The AUC values of Models 1 and 2 were statistically comparable (Table 2; AUC: 0.840 vs 0.882, P = 0.193). And the AUC of Model 3 was significantly greater than the AUCs of the other two models (Table 2; AUC: 0.940 vs 0.840, 0.882; both P < 0.05). In Model 3, the cut-off value of 0.814 presented a sensitivity of 90.6% and a specificity of 86.8%. (Table 2, Fig. 3)
Discussion
This study showed that the foveal ONL thickness before PDT, the foveal ONL thickness ratio before and that after half-dose PDT were all independent predictors of the visual outcome of half-dose PDT. The foveal ONL thickness ratio after PDT could best predict the visual outcome of PDT, with a cut-off value of 0.81.
Consistent with the previous study, this study showed that foveal ONL thickness before PDT was independently associated with the visual outcome after PDT [14] (Table 2; Model 1). The foveal ONL contains cone cell bodies. The reduction in foveal ONL thickness indicated cone cells loss, which resulted in a visual acuity decrease [5, 16].
Although the difference between the AUCs of Model 1 and Model 2 did not reach statistical significance, the AUC of Model 2 was greater than the AUC of Model 1(Table 2 and Fig. 3), which suggested that the ratio of foveal ONL thickness before PDT might be better than the value of foveal ONL thickness before PDT in predicting the visual outcome. In our previous study, we demonstrated that the foveal ONL thickness varied widely in a normal Chinese population (Also shown in Fig. 2C, F), but that there was little difference between the bilateral eyes (OD: 103.19 ± 14.25 μm) [range 70–151]; OS: 103.90 ± 14.63 μm [range 69–155]; OD-OS: −0.71 ± 4.36 μm [range −13 to +12] [21]. In this study, since only one eye was affected with CSC in each patient, the normal contralateral eye could be used as the control. We hypothesised that the ratio of the foveal ONL thickness in the CSC eye to that in the normal contralateral eye was better than the value of foveal ONL thickness in the CSC eye to indicate the extent of reduction in foveal ONL thickness due to CSC. For example, the eye in Fig. 2A, and the eye in Fig. 2D, both had similar baseline foveal ONL thicknesses (61 μm and 60 μm, respectively), whereas their ratios of foveal ONL thickness before PDT differed (0.70 and 0.55, respectively). This partly explained their significantly different visual outcomes after PDT (Fig. 2). Compared with the absolute value, the ratio removed the contribution of inter-individual variation. Therefore, the ratio of the foveal ONL thickness before PDT might be better than the thickness value for predicting the outcome of PDT.
Moreover, this study showed that the AUC in Model 3 was significantly greater than those in either Model 2 or Model 1 (Table 2). This suggested that the foveal ONL thickness ratio after PDT can best predict the visual outcome. The ONL thinning was considered due to the photoreceptor cells loss [5, 16]. However, our previous study showed that, besides photoreceptor cells loss, retinal stretch also contributed to the foveal ONL thinning in the active CSC eyes [22]. And retinal stretch recovered when the subretinal fluid resolved, leading to foveal ONL thickness increase in some degree, ranging 9.15 ± 8.16 μm [22] (also shown in Fig. 2A, B, 22 μm; D, E, 2 μm). Therefore, the ratio before PDT may more or less lead to the overestimation of the loss of photoreceptors. Because there is no quantitative formula with which to calculate the contribution of retinal stretch to foveal ONL thinning, it remained impossible to determine the precise extent of reduction in photoreceptors in the active phase of CSC. Therefore, only the ratio of the foveal ONL thickness after PDT can precisely indicate the actual extent of photoreceptors loss, because it removed the influence of both retinal stretch and inter-individual variation.
Since the value of foveal ONL thickness before PDT in Model 1 and the ratio of foveal ONL thickness before PDT in Model 2 was influenced by inter-individual variation and/or retinal stretch, neither of these parameters could precisely indicate the actual extent of reduction in photoreceptors. Therefore, the cut-off points in these models (75.5 μm in Model 1 and 0.75 in Model 2) may not be reliable enough.
However, the foveal ONL thickness ratio after PDT in Model 3 was not influenced by either inter-individual variation or the retinal stretch, and thus, the threshold determined for this parameter was accurate and stable. The cut-off value was 0.81, which suggested that eyes with residual photoreceptors of more than 81% can retain visual acuity of 20/20 after PDT. Based on the retinal stretch hypothesis, if the foveal ONL thickness ratio before PDT was 0.81, the ratio would increase to some extent to more than 0.81 after PDT, due to retinal stretch recovery. That is, eyes, with a foveal ONL thickness ratio before PDT of 0.81, do actually hold more than 81% residual photoreceptors, and thus these eyes can recover to visual acuity of 20/20 after PDT. Therefore, we could conservatively conclude that it is reasonable to wait for spontaneous resolution of sub-retinal fluid in eyes with foveal ONL thickness ratio before PDT of >0.81.
Although acute CSC is typically a self-limiting process with few recognised visual sequelae, recurrent CSC and chronic CSC may develop RPE atrophy and neurosensory retinal changes that result in permanent loss of visual function [2,3,4]. Recently, Mrejen has reported that 12.8% of their 133 chronic CSC study patients progressed to bilateral legal blindness [23]. Half-dose PDT has become a major treatment for CSC [4, 8,9,10,11,12,13]. At present, the timing of half-dose PDT depends mainly on the duration of symptoms [8,9,10,11,12,13]. However, symptom duration is subjective and sometimes arbitrary. In contrast, the foveal ONL thickness is objective. Moreover, patients with similar symptom duration can differ in their outcomes after PDT, whereas, those with different symptom duration but a similar extent of reduction in foveal ONL thickness had similar outcomes after PDT [15]. Furthermore, both Ohkuma and we (this study) showed that the foveal ONL thickness was independently associated with the visual outcome of PDT [14]. (Table 2) Therefore, besides symptom duration, we believe the foveal ONL thickness can be helpful in determining the timing of PDT.
Our data suggested that the foveal ONL thickness ratio after PDT could best predict visual outcome after PDT, with a cut-off value of 0.81. Based on the retinal stretch hypothesis, in active CSC eyes whose foveal ONL thickness ratio was >0.81, although PDT may be an option, waiting for spontaneous resolution of the subretinal fluid was also reasonable. Whereas, for eyes with foveal ONL thickness ratio <0.81, immediate PDT was suggested to promote quick resolution of the subretinal fluid, thus, to retain the residual photoreceptors as much as possible. And these patients should be informed that their visual acuity after PDT might be worse than 20/20. In addition, for those patients with foveal ONL thickness in the normal contralateral eye close to the minimum value (70 μm) [21], immediate half-dose PDT was also recommended, even if the foveal ONL thickness ratio before PDT was >0.81, to retain as many of the limited number of photoreceptors as possible. Further studies with methods to remove the contribution of retinal stretch, thus obtaining a precise extent of reduction in foveal ONL thickness in the active phase, may be helpful to determine the latest timing for PDT more accurately. The threshold of foveal ONL thickness ratio at which a visual acuity of 20/20 was retained, 0.81, should also be tested in other progressive degeneration diseases. This study was limited by its retrospective design and relatively small population. Moreover, the axial length was not included. As the ranges of SEs in both eyes were relatively small and the difference in SEs between bilateral eyes was ≤1 dioptre in each patient, the axial length might not have affected the results significantly. Further prospective studies with large populations and axial length might tell us more.
The threshold of the foveal ONL thickness ratio is 0.81. Active CSC eyes with a foveal ONL thickness ratio of 0.81 or more could probably retain BCVA of 20/20 after half-dose PDT. They were considered reasonable to wait for spontaneous resolution of sub-retinal fluid.
Summary
What was known before
-
Half-dose photodynamic therapy (PDT) has become a major treatment for central serous chorioretinopathy (CSC).
-
The timing of half-dose PDT, mainly depending on symptom duration, remains somewhat arbitrary.
-
The value of the foveal outer nuclear layer (ONL) thickness of the CSC eye was an independent predictor of the visual outcome of half-dose PDT.
What this study adds
-
The ratio of foveal ONL thickness in the CSC eye to that in the normal contralateral eye is better at predicting PDT outcome than the value of foveal ONL thickness in the CSC eye.
-
The threshold of the foveal ONL thickness ratio is 0.81.
-
It indicated that the active CSC eyes with a foveal ONL thickness ratio of 0.81 or more could probably retain visual acuity of 20/20 after half-dose PDT. Therefore, these eyes are considered reasonable to wait for spontaneous resolution of sub-retinal fluid.
References
Klais CM, Ober MD, Ciardella AP, Yannuzzi LA. Central serous chorioretinopathy. In: Schachat AP editors. Retina. Vol 2, 4th edn. St. Louis: Mosby Publishing Ltd; 2006. p. 1135-61.
Klein ML, Van Buskirk EM, Friedman E, Gragoudas E, Chandra S. Experience with nontreatment of central serous choroidopathy. Arch Ophthalmol. 1974;91:247–50.
Yannuzzi LA. Central serous chorioretinopathy: a personalperspective. Am J Ophthalmol. 2010;149:361–363.
van Rijssen TJ, van Dijk EHC, Yzer S, Ohno-Matsui K, Keunen JEE, Schlingemann RO, et al. Central serous chorioretinopathy: towards an evidence-based treatment guideline. Prog Retin Eye Res. 2019;73:100770.
Hata M, Oishi A, Shimozono M, Mandai M, Nishida A, Kurimoto Y. Early changes in foveal thickness in eyes with central serous chorioretinopathy. Retina. 2013;33:296–301.
Cook B, Lewis GP, Fisher SK, Adler R. Apoptotic photoreceptor degeneration in experimental retinal detachment. Investig Ophthalmol Vis Sci. 1995;36:990–996.
Hisatomi T, Sakamoto T, Goto Y, Yamanaka I, Oshima Y, Hata Y, et al. Critical role of photoreceptorapoptosis in functional damage after retinal detachment. Curr Eye Res. 2002;24:161–172.
Lai TY, Chan WM, Li H, Lai RY, Liu DT, Lam DS. Safety enhanced photodynamic therapy with half dose verteporfin for chronic central serous chorioretinopathy: a short term pilot study. Br J Ophthalmol. 2006;90:869–874.
Chan WM, Lai TY, Lai RY, Liu DT, Lam DS. Half-dose verteporfin photodynamic therapy for acute central serous chorioretinopathy: one-year results of a randomized controlled trial. Ophthalmology. 2008;115:1756–1765.
Kim KS, Lee WK, Lee SB. Half-dose photodynamic therapy targeting the leakage point on the fluorescein angiography in acute central serous chorioretinopathy: a pilot study. Am J Ophthalmol. 2014;157:366–373.e1.
Fujita K, Imamura Y, Shinoda K, Matsumoto CS, Mizutani Y, Hashizume K, et al. One-year outcomes with half-dose verteporfin photodynamic therapy for chronic central serous chorioretinopathy. Ophthalmology. 2015;122:555–561.
Tseng CC, Chen SN. Long-term efficacy of half-dose photodynamic therapy on chronic central serous chorioretinopathy. Br J Ophthalmol. 2015;99:1070–7.
Lai FH, Ng DS, Bakthavatsalam M, Chan VC, Young AL, Luk FO, et al. A multicenter study on the long-term outcomes of half-dose photodynamic therapy in chronic central serous chorioretinopathy. Am J Ophthalmol. 2016;170:91–99.
Ohkuma Y, Hayashi T, Sakai T, Watanabe A, Tsuneoka H. One-year results of reduced fluence photodynamic therapy for central serous chorioretinopathy: the outer nuclear layer thickness is associated with visual prognosis. Graefes Arch Clin Exp Ophthalmol. 2013;251:1909–17.
Yu J, Ye X, Li L, Chang Q, Jiang C. Relationship between photoreceptor layer changes before half-dose photodynamic therapy and functional and anatomic outcomes in central serous chorioretinopathy. Eye. 2021;35:1002–10.
Matsumoto H, Sato T, Kishi S. Outer nuclear layer thickness at the fovea determines visual outcomes in resolved central serous chorioretinopathy. Am J Ophthalmol. 2009;148:105–.e1.
Guyer DR, Yannuzzi LA, Slakter JS, Sorenson JA, Ho A, Orlock D. Digital indocyanine green videoangiography of central serous chorioretinopathy. Arch Ophthalmol. 1994;112:1057–62.
Yu J, Jiang C, Xu G. Correlations between changes in photoreceptor layer and other clinical characteristics in central serous chorioretinopathy. Retina. 2019;39:1110–6.
Yu J, Jiang C, Wang X, Zhu L, Gu R, Xu H, et al. Macular perfusion in healthy Chinese: an optical coherence tomography angiogram study. Invest Ophthalmol Vis Sci. 2015;56:3212–3217.
DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44:837–45.
Yu J, Li L, Jiang C, Chang Q & Zhao Q. Inter- and intra-individual variations in foveal outer nuclear layer thickness and their associations with clinical characteristics in a healthy Chinese population. J Ophthalmol. 2020; 7967393.
Yu J, Lei Y, Chang Q, Xu G, Ye X, Li L, et al. The relationship between foveal outer nuclear layer thickness in the active and resolved phases of central serous chorioretinopathy treated with half-dose photodynamic therapy. BMC Ophthalmol. 2019;19:84.
Mrejen S, Balaratnasingam C, Kaden TR, Bottini A, Dansingani K, Bhavsar KV, et al. Long-term visual outcomes and causes of vision loss in chronic central serous chorioretinopathy. Ophthalmology. 2019;126:576–88.
Acknowledgements
This research was supported by the National Natural Science Foundation of China (Grant nos. 81870670 and 81900867), the Shanghai Committee of Science and Technology (Grant no.18411965100), and the Shanghai clinical three-year action plan-major clinical research project (SHDC2020CR2041B).
Author information
Authors and Affiliations
Contributions
QC and GX contributed equally as co-corresponding authors. CQ and XG designed the study. YX and LL performed the photodynamic therapy. YJ, YX, and LL collected the data. YJ, CQ, and JC analysed and interpreted the data. YJ was a major contributor in writing the manuscript. YX and LL participated in drafting the manuscript. CQ, XG, and JC revised the manuscript. All authors approved the final version and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding authors
Ethics declarations
Ethics approval
This retrospective study was approved by the Ethics Committee of the Eye & Ear, Nose, Throat Hospital of Fudan University Shanghai China (2020052).
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yu, J., Ye, X., Li, L. et al. Threshold thickness of foveal outer nuclear layer associated with outcomes of photodynamic therapy in central serous chorioretinopathy. Eye 36, 1884–1889 (2022). https://doi.org/10.1038/s41433-021-01762-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01762-0
This article is cited by
-
Evaluation of changes in macular structures after subthreshold micropulse laser therapy on chronic central serous chorioretinopathy
Lasers in Medical Science (2024)
-
Outer nuclear layer recovery as a predictor of visual prognosis in type 1 choroidal neovascularization of neovascular age-related macular degeneration
Scientific Reports (2023)