Abstract
Objectives
To investigate the relationship between photoreceptor layer (PRL) changes before half-dose photodynamic therapy (PDT) and functional and anatomic outcomes in central serous chorioretinopathy (CSC).
Methods
Baseline PRL changes were classified based on optical coherence tomography: (1) smooth PRL outer border without a foveal PRL defect; (2) smooth PRL outer border with a foveal PRL defect; (3) granulated PRL outer border and (4) scattered dots of PRL. The best-corrected visual acuity (BCVA), difference in the foveal outer nuclear layer (ONL) thickness between the CSC and normal contralateral eyes and ellipsoid zone (EZ) integrity 12 months after half-dose PDT were compared.
Results
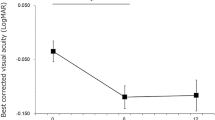
In total, 132 patients were included. Group 4 eyes had rather poor BCVA (20/2000–20/400) with little improvement (P = 0.088) at 1 year following half-dose PDT. In the other groups, the mean BCVA improved significantly to 20/25 or better (all P < 0.001). Group 1 eyes had the smallest foveal ONL thickness reduction (−5.12 ± 6.89 μm) and intact EZs (33/33), whereas Group 4 eyes had the largest foveal ONL thickness reduction (−70.00 ± 7.87 μm) and disrupted EZs (4/4). Group 2 and Group 3 eyes behaved similarly: they both had notable foveal ONL thickness reductions (−19.21 ± 18.53 and −20.75 ± 17.62 μm, respectively), but usually continuous EZs (18/19 and 69/76, respectively).
Conclusions
The PRL change category before half-dose PDT was closely related to functional and anatomic outcomes. This information could aid clinicians to better determine the timing of treatment with half-dose PDT in CSC.
Similar content being viewed by others
Introduction
Central serous chorioretinopathy (CSC) is a common macular disease and often presents with well-circumscribed serous retinal detachment in the macular region on clinical examination, with one or several leakage points at the level of the retinal pigment epithelium (RPE) detectable with fluorescein angiography (FA) [1]. Although acute CSC is typically a self-limiting process with few recognised visual sequelae, patients with recurrent CSC and chronic CSC may develop RPE atrophy and neurosensory retinal changes that result in permanent loss of visual function [2,3,4]. Recently, Mrejen has reported that 12.8% of their 133 chronic CSC study patients progressed to bilateral legal blindness [5]. Half-dose photodynamic therapy (PDT) has been shown to be effective not only in promoting the resolution of subretinal fluid but also in preventing recurrence [6,7,8,9,10,11]. However, the timing of half-dose PDT, which mainly depends on symptom duration, remains somewhat arbitrary [4, 12,13,14].
Symptom duration and visual acuity are known predictive factors for the visual outcome of half-dose PDT [9, 11, 15]; however, these are continuous variables, and the precise values of their turning points during a CSC episode have not yet been defined. Recently, it has been reported that photoreceptor layer (PRL) changes on optical coherence tomography (OCT) correlate closely with symptom duration and visual acuity [14].
To determine the relationship between PRL changes before half-dose PDT and the functional and anatomic outcomes of half-dose PDT, the medical records of patients with CSC were reviewed in this study: the morphological changes in the PRL before half-dose PDT were classified, and then the best-corrected visual acuity (BCVA), the foveal ONL thickness and the integrity of the ellipsoid zone (EZ) 12 months after half-dose PDT were analysed. The association between the PRL change category and BCVA 12 months after half-dose PDT was also assessed.
Materials and methods
This study was approved by the ethics committee of the Eye and Ear Nose Throat Hospital of Fudan University. Written informed consent was obtained from all the patients in accordance with the Declaration of Helsinki. The medical records of the CSC patients who received half-dose PDT between December 2011 and March 2018 were reviewed.
Patients
The clinical diagnosis of CSC was based on symptoms, reduced visual acuity with or without metamorphopsia or micropsia; the presence of serous retinal detachment on both fundus and OCT examinations; the presence of active angiographic leakage on FA (TRC-50IX; Topcon Corp., Tokyo, Japan) or abnormally dilated choroidal vasculature and other features on indocyanine green angiography (ICGA; Spectralis HRA + OCT; Heidelberg Engineering, Heidelberg, Germany) consistent with the diagnosis of CSC [16].
The subjects included were those with clear and detailed medical records: one affected eye in the first recorded episode of CSC and a normal contralateral eye (BCVA ≥20/20); no clinical signs or history of any other intraocular disease in either eye; no history of CSC or active CSC in the contralateral eye; accurately known symptom duration; subretinal fluid resolution within 2 months of half-dose PDT and no recurrence within 12 months of half-dose PDT.
Data for both eyes were collected, including the BCVA, which was measured with a standard Snellen chart and converted to the logarithm of the minimum angle of resolution (logMAR) for statistical analysis, clinical examination information and OCT examination. The symptom duration and half-dose PDT spot diameter in each CSC eye were also collected.
Half-dose PDT protocol
The PDT protocol for CSC was performed using half of the normal dose of verteporfin (Visudyne; Novartis AG, Bülach, Switzerland), that is, 3 mg/m2 verteporfin, with the rationale that using a lower dose has less severe collateral damaging effects on the retina and choroid. Verteporfin was infused over 8 min, followed by delivery of laser at 689 nm at 10 min from the commencement of infusion to target the area of choroidal dilation and hyperpermeability. A total light energy of 50 J/cm2 over 83 s was delivered either to the angiographic leakage sites shown in FA or the area of choroidal hyperperfusion as observed in ICGA [6, 8].
It has been considered that FA-guided half-dose PDT with the smallest spot size large enough to cover the point of active leakage on early-phase FA can potentially reduce the risk of further complications [8]. On the other hand, the area of abnormal choroidal vasculature can be visualised better with ICGA than with FA [7]. Thus, ICGA-guided PDT may have the benefit of reducing recurrence [8]. Therefore, in this study, patients with symptom duration of <3 months underwent FA to determine the spot size of PDT, whereas patients with symptom duration of more than 3 months underwent ICGA to determine the spot size of PDT [6, 8].
OCT protocol
All OCT images were obtained with a line scan protocol (line scans of 30°, composed of 100 averaged images; Heidelberg Spectralis OCT, Heidelberg Engineering, Heidelberg, Germany). This protocol was applied to both eyes of each participant both vertically and horizontally and centred on the fovea. The OCT images that passed through the central fovea were selected for the analysis of morphological changes in the PRL and the measurement of the ONL thickness. OCT images taken within 1 week before half-dose PDT and 2 months (±2 weeks) and 12 months (±2 weeks) after half-dose PDT were analysed.
OCT image analysis
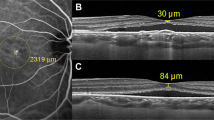
The PRL changes before half-dose PDT was classified into four types: (1) smooth PRL outer border with no PRL defect involving the fovea (Fig. 1a); (2) smooth PRL outer border with a PRL defect involving the fovea (Fig. 1c, e); (3) granulated PRL outer border (Fig. 1g, i) and (4) scattered dots of PRL (Fig. 1k) [14]. The integrity of the EZ 12 months after half-dose PDT was classified into two types: (1) continuous EZ on both the horizontal and vertical scans within 1 mm of the centre of the fovea or (2) disrupted EZ on either the horizontal or vertical scan within 1 mm of the centre of the fovea [17].
a Scan of a patient with BCVA of 20/20 and symptom duration of 41 days before half-dose PDT. The PRL outer border within the detached area was smooth without foveal PRL defect. b Scan of the eye 12 months after PDT. The BCVA was 20/20, the foveal ONL thickness difference was −4 μm and the EZ was continuous. c Scan of a patient with BCVA of 20/25 and symptom duration of 70 days before half-dose PDT. The PRL outer border within the detached area is smooth with a foveal PRL defect. d Scan of the eye 12 months after PDT. The BCVA was 20/20, the foveal ONL thickness difference was −38 μm and the EZ was continuous. e Scan of a patient with BCVA of 20/63 and symptom duration of 74 days before half-dose PDT. The PRL outer border within the detached area was smooth with a foveal PRL defect. f Scan of the eye 12 months after PDT. The BCVA was 20/40, the foveal ONL thickness difference was −43 μm, and the EZ was disrupted superior to the central fovea. g Scan of a patient with BCVA of 20/63 and symptom duration of 337 days before half-dose PDT. The PRL outer border within the detached area was granulated. h Scan of the eye 12 months after PDT. The BCVA was 20/20, the foveal ONL thickness difference was −32 μm and the EZ was continuous. i Scan of a patient with BCVA of 20/125 and symptom duration of 139 days before half-dose PDT. The PRL outer border within the detached area was granulated. j Scan of the eye 12 months after PDT. The BCVA was 20/400, the foveal ONL thickness difference was −60 μm and the EZ was disrupted on the nasal and temporal sides of the central fovea. k Scan of a patient with BCVA of 20/400 and symptom duration of 3692 days before half-dose PDT. The PRL within the detached area showed scattered dots. l Scan of the eye 12 months after PDT. The BCVA was 20/2000, the foveal ONL thickness difference was −74 μm and both the EZ and the external limiting membrane were disrupted throughout the macula.
The foveal ONL thickness was calculated as the average of the distance between the internal limiting membrane (ILM) and the external limiting membrane (ELM) at the centre of the fovea measured from the horizontal and vertical images across the centre of the fovea [14]. If the ELM was absent, the foveal ONL thickness was defined as the average distance between the ILM and the RPE at the centre of the fovea, measured on the horizontal and vertical images. The difference in the foveal ONL thickness was defined as the difference between the foveal ONL thickness in the CSC eye and that in the contralateral eye. The measurements were made manually using the supplied software (in 1:1 μm mode; HRA/Spectralis Viewing Module 6.0.9.0, Heidelberg Engineering).
When classifying the morphological changes of the PRL, the intra-grader repeatability and inter-grader reproducibility were determined for all the OCT images evaluated by three of the authors (JY, CJ and QC), who independently read all the OCT images twice, at an interval of 2-gap-week, and were masked to the information on the BCVA and symptom duration. They then discussed their decisions when there was any disagreement among them. The PRL change classification was based on the final results of the three authors (JY, CJ and QC). Both the intra-grader repeatability and inter-grader reproducibility were assessed as the percentage agreement [18, 19]. Kappa (κ) statistics and corresponding 95% confidence intervals (CIs) were also reported using the guidelines proposed by Koch eand Landis [20, 21].
For the foveal ONL thickness measurements, both intra-observer repeatability and inter-observer reproducibility were evaluated on 20 normal eyes and 20 CSC eyes. JY measured the same scan from each eye twice at an interval of 1 week to calculate the intra-observer repeatability. The inter-observer reproducibility was evaluated between JY and CJ, who measured the same scans independently. All the measurements of foveal ONL thicknesses were then made by JY. Intraclass correlation coefficients (ICCs) were used to assess the repeatability and reproducibility of the measurements [22].
Statistics analysis
The data were analysed with SPSS version 21.0 for Windows (SPSS, Chicago, IL, USA). The calculated values are presented as either frequencies (proportions), means ± standard deviations, or medians. The Kolmogorov–Smirnov test was used to confirm the normality of the data. Either the Wilcoxon signed-rank test or paired t test was used to evaluate the differences in the BCVA before half-dose PDT and 12 months after half-dose PDT. Among the eyes in different baseline PRL change groups, the symptom duration before half-dose PDT, the BCVA before and 12 months after half-dose PDT and the foveal ONL thickness difference at 12 months after half-dose PDT were compared using either the Kruskal–Wallis test or one-way ANOVA, followed by post hoc multiple comparisons. The association between the PRL change category before half-dose PDT (independent variable) and BCVA 12 months after half-dose PDT (dependent variable of interest) was assessed with generalised linear regression analysis. Factors such as BCVA before half-dose PDT, symptom duration, sex, age and half-dose PDT spot diameter were included in a multivariate model to adjust for potential confounding. A P value < 0.05 was considered statistically significant.
Results
In total, 663 eyes from 583 patients with CSC underwent half-dose PDT either by XY or LL at our hospital between December 2011 and March 2018. Of these eyes, 599 (90.3%) had complete resolution of the subretinal fluid at 2 months after half-dose PDT. Eventually, 132 (22.6%) patients who met the inclusion criteria were included in the study. No complications following half-dose PDT, such as RPE atrophy, choroidal neovascularization or systemic adverse events, were observed until the end of the 1-year follow-up. The demographic data for the patients are listed in Table 1. The classification of the morphological changes of the PRL showed good repeatability and reproducibility. The intra-grader repeatability scores for JY, CJ and QC were similar, with 94.7% agreement (κ = 0.91, 95% CI 0.85–0.97), 95.5% agreement (κ = 0.92, 95% CI 0.86–0.98) and 96.2% agreement (κ = 0.94, 95% CI 0.87–0.99), respectively. The inter-grader reproducibility was also satisfactory, with an agreement rate of 95.5% (κ = 0.92, 95% CI 0.85–0.98) between JY and CJ, 94.7% (κ = 0.91, 95% CI 0.84–0.97) between CJ and QC and 94.7% (κ = 0.91, 95% CI 0.84–0.97) between QC and JY. The measurements of the foveal ONL thickness by JY showed good intra-observer repeatability, with an ICC value of 0.978 for normal eyes and 0.990 for CSC eyes. The inter-observer reproducibility between JY and CJ was also satisfactory, with an ICC value of 0.968 for normal eyes and 0.987 for CSC eyes.
Eyes in different PRL change groups before half-dose PDT behaved rather differently in terms of their BCVA, foveal ONL thickness difference and EZ integrity 12 months after half-dose PDT (Fig. 1a–l, and Table 2). The eyes with scattered dots of PRL had rather poor BCVA (20/2000–20/400), with little improvement (P = 0.088), whereas the mean BCVA improved significantly in the other groups to 20/25 or better (all P < 0.001). The eyes with smooth PRL outer border without foveal PRL defect had the smallest foveal ONL thickness reduction (−5.12 ± 6.89 μm) and intact EZ (33/33), whereas the eyes with scattered dots of PRL had the largest foveal ONL thickness reduction (−70.00 ± 7.87 μm) and disrupted EZ (4/4). The eyes with smooth PRL and foveal PRL defect and the eyes with granulated PRL behaved similarly; both showed a notable reduction in foveal ONL thickness (−19.21 ± 18.53 and −20.75 ± 17.62 μm, respectively), but most had continuous EZ (18/19 and 69/76, respectively).
The PRL change category was independently associated with BCVA 12 months after half-dose PDT, even after adjusting for baseline clinical characteristics such as BCVA, symptom duration, sex, age and half-dose PDT spot diameter (generalised linear regression analysis: all P < 0.001).
Discussion
This study shows that the functional and anatomic outcomes after half-dose PDT were closely related to the PRL change category before half-dose PDT. All eyes with smooth PRL without foveal PRL defect showed significant recovery in their BCVA, a minimal reduction in their foveal ONL thickness, and intact EZ, whereas all eyes with scattered dots of PRL showed limited improvement in their BCVA, a significant reduction in their foveal ONL thickness, and disrupted EZ; the remaining eyes showed partial recovery in these parameters (Table 2).
In the eyes with smooth PRL without foveal PRL defect before half-dose PDT (Table 2, Group 1), the foveal ONL thickness difference after half-dose PDT was ~−5 μm. Because the ONL at the centre of the fovea contains the nuclei of cone photoreceptors, this slight decrease may indicate that these CSC eyes had a minimal loss of cone cells [13, 17]. However, the mean BCVA was restored to 20/20, and the EZ was continuous in all of these eyes, suggesting that half-dose PDT restored both a generally normal anatomy and normal function to these eyes. Moreover, the eyes in Group 1 showed a mean symptom duration of 41 days (Table 2), suggesting that waiting for spontaneous resolution of the subretinal fluid in these eyes, within a period of 41 days, was reasonable.
Eyes with smooth PRL and foveal PRL defect (Table 2, Group 2) and eyes with granulated PRL (Table 2, Group 3) achieved quite similar results in both their BCVA and foveal ONL thickness after half-dose PDT (Table 2; both P > 0.05), although the symptom duration was much shorter in Group 2 (Table 2; mean, 58 vs. 195 days, P < 0.001). On the one hand, Group 2 and Group 3 showed a steady improvement in BCVA after half-dose PDT (Table 2; both P < 0.001), and some eyes even achieved a BCVA of 20/20, and the EZ was continuous in most eyes (Table 2; 18/19 and 69/76, respectively) (Fig. 1d, h).These results indicated that the outcomes of half-dose PDT evaluated by BCVA and EZ status were satisfactory for both Group 2 and Group 3. On the other hand, the foveal ONL thickness difference after half-dose PDT in Group 2 and Group 3 were both significantly smaller than that in Group 1 (Table 2; −19.21 and −20.75 vs. −5.12 μm, respectively; both P < 0.05). This finding suggested that there was notable cone cell loss both in Group 2 and Group 3, and therefore, the mean BCVA after half-dose PDT in these two groups had decreased slightly to ~20/25. The observations described above that the eyes with obvious ONL thinning can maintain BCVA of 20/25 may support the hypothesis that there may be a ‘threshold’ of ONL thickness to retain some level of visual acuity [13]. Half-dose PDT has been shown to effectively promote the resolution of the subretinal fluid, thus it could quickly stop the ONL thinning in the current episode [6,7,8,9,10,11, 13]. Moreover, half-dose PDT has been reported to significantly reduce the recurrence rate [9,10,11], thus it can further protect these eyes from recurrence. Therefore, until the possible precise threshold of ONL thickness is defined, half-dose PDT should be performed promptly to these eyes to retain as much of the residual ONL thickness as possible.
All four patients whose PRL showed scattered dots (Table 2, Group 4) had quite similar post-PDT results: rather poor BCVA of 20/2000–20/400, significant foveal ONL thinning of ~−70 μm, and disrupted EZ. This high degree of ONL thinning suggests a marked loss of photoreceptor cells in these eyes. Moreover, although the ELM was continuous in the active phase of these eyes, it was disrupted when the subretinal fluid was resolved (Fig. 1k, l). The exact mechanism underlying this phenomenon remains unknown. The ELM, which is formed by a tangentially oriented series of adhesions, zonulae adherens, connecting the apical processes of the Müller cells with inner segments of photoreceptors, could help to maintain the alignment and orientation of the photoreceptors [23]. It is therefore regarded as a predictive factor for the subsequent restoration of the PRL and visual improvement in various diseases, including macular oedema, CSC, retinal detachment, and macular hole [23,24,25,26]. A disrupted ELM might suggest combined damage to both the PRL and the photoreceptor cell bodies [24, 27]. Therefore, it suggested that EZ recovery in these eyes can no longer be expected. Although the subretinal fluid was resolved completely, neither the morphology nor the BCVA of these CSC eyes improved. Because the eyes of this type had extremely long symptom duration (Table 2: mean, 1437 days), half-dose PDT may have been performed too late.
We also demonstrated that the PRL change category before half-dose PDT was independently associated with BCVA after half-dose PDT (generalised linear regression analysis: all P < 0.001). It has been reported that the symptom duration and baseline BCVA are characteristics that are related to visual outcome [9, 11, 15], and these two parameters are closely related to the PRL change category in eyes with active CSC [14]. However, these three parameters may not always behave in a synchronous manner: eyes with smooth PRL outer border without foveal PRL defect and eyes with smooth PRL outer border and foveal PRL defect had similar symptom durations (Table 2; 41 vs. 58, P = 0.757) but different BCVA (Table 2; logMAR 0.13 vs. 0.33, P = 0.001); eyes with smooth PRL outer border and foveal PRL defect and eyes with granulated PRL outer border had different symptom durations (Table 2; 58 vs. 195, P < 0.001) but similar BCVA (Table 2; logMAR 0.33 vs. 0.36, P = 1.000). This asynchronous phenomenon may support the statistical finding that the PRL change category was independent of BCVA and symptom duration. Symptom duration and BCVA are parameters indirectly associated with the status of the photoreceptor cells, whereas the various morphological changes in the PRL are directly related to the ability for PRL renewal of the photoreceptor cells and are associated with different degrees of reduction of photoreceptor cells [14]. Therefore, in addition to symptom duration and BCVA before treatment, we believe that PRL change category can serve as an effective predictor of visual outcomes after half-dose PDT.
CSC is usually considered a self-limiting process, with a promising visual prognosis. However, chronic CSC entails a loss of vision, attributable to cumulative photoreceptor cell death as retinal detachment persists [13, 28,29,30]. Half-dose PDT has become a major treatment for CSC [4, 6,7,8,9,10,11]. At present, the timing of half-dose PDT depends mainly on the duration of symptoms [6,7,8,9,10,11]. Symptom duration, determined from the recollection of the patient, is subjective and sometimes ambiguous [4, 12,13,14]. Furthermore, CSC eyes with similar symptom durations can differ in their vision and anatomy [14]. Compared with symptom duration, the morphological changes of PRL on OCT is objective and directly associated with the photoreceptor status [14]. Moreover, although symptom duration and BCVA are known predictive factors for the visual outcome of half-dose PDT [9, 11, 15], they are continuous variables, and the precise values of their turning points during a CSC episode have not yet been defined. However, the morphological changes of the PRL is a categorical variable. Moreover, PRL changes on OCT is visible and clear to doctors. For these reasons, we compared BCVA ranges, degrees of reduction in the foveal ONL thickness and the integrity of the EZ at 12 months after half-dose PDT based on their PRL change category before PDT. Our data show that the classification of PRL changes is a practical and effective way to differentiate CSC eyes. CSC eyes, except those with scattered dots of PRL, showed improvement in BCVA after half-dose PDT. Eyes with smooth PRL and foveal PRL defect and eyes with granulated PRL behave similarly after half-dose PDT, and both may require immediate half-dose PDT. It should be further investigated whether the functional and anatomic outcomes for eyes with smooth PRL without foveal PRL defect differs after immediate half-dose PDT and after spontaneous resolution of the subretinal fluid. The number of cases with scattered dots of PRL was also limited. In our hospital, only patients with symptom duration <3 months were advised to be followed up for possible spontaneous resolution of the subretinal fluid, the others were prescribed immediate half-dose PDT. Thus, cases with such long symptom duration before half-dose PDT can rarely be obtained. A future study with more cases of symptom duration longer than 3 months may confirm the benefits of half-dose PDT for these eyes. This study was limited by its retrospective design, and further prospective studies with long-term follow-ups and large populations might tell us more.
The PRL change category before half-dose PDT is closely related to the functional and anatomic outcome of half-dose PDT. It is an independent predictive factor for the BCVA after half-dose PDT. Therefore, the PRL category prior to treatment with half-dose PDT could be helpful when considering the timing of half-dose PDT in CSC.
Summary
What was known before
-
Half-dose PDT has become a major treatment for CSC.
-
The timing of half-dose PDT, mainly depending on symptom duration, remains somewhat arbitrary.
-
Symptom duration is subjective and sometimes ambiguous.
What this study adds
-
The PRL change category before half-dose PDT was closely related to functional and anatomic outcomes.
-
PRL change category is also an independent predictive factor for the visual acuity after half-dose PDT.
-
PRL change category prior to treatment with half-dose PDT could be helpful when considering the timing of half-dose PDT.
References
Klais CM, Ober MD, Ciardella AP, Yannuzzi LA. Central serous chorioretinopathy. In: Schachat AP, editor. Retina, vol 2. 4th ed. St. Louis, Missouri, USA: Mosby Publishing Ltd; 2006. p. 1135–61.
Klein ML, Van Buskirk EM, Friedman E, Gragoudas E, Chandra S. Experience with nontreatment of central serous choroidopathy. Arch Ophthalmol. 1974;91:247–50.
Yannuzzi LA. Central serous chorioretinopathy: a personal perspective. Am J Ophthalmol. 2010;149:361–3.
Nicholson B, Noble J, Forooghian F, Meyerle C. Central serous chorioretinopathy: update on pathophysiology and treatment. Surv Ophthalmol. 2013;58:103–26.
Mrejen S, Balaratnasingam C, Kaden TR, Bottini A, Dansingani K, Bhavsar KV, et al. Long-term visual outcomes and causes of vision loss in chronic central serous chorioretinopathy. Ophthalmology. 2019;126:576–88.
Lai TY, Chan WM, Li H, Lai RY, Liu DT, Lam DS. Safety enhanced photodynamic therapy with half dose verteporfin for chronic central serous chorioretinopathy: a short term pilot study. Br J Ophthalmol. 2006;90:869–74.
Chan WM, Lai TY, Lai RY, Liu DT, Lam DS. Half-dose verteporfin photodynamic therapy for acute central serous chorioretinopathy: one-year results of a randomized controlled trial. Ophthalmology. 2008;115:1756–65.
Kim KS, Lee WK, Lee SB. Half-dose photodynamic therapy targeting the leakage point on the fluorescein angiography in acute central serous chorioretinopathy: a pilot study. Am J Ophthalmol. 2014;157:366–73.e1.
Fujita K, Imamura Y, Shinoda K, Matsumoto CS, Mizutani Y, Hashizume K, et al. One-year outcomes with half-dose verteporfin photodynamic therapy for chronic central serous chorioretinopathy. Ophthalmology. 2015;122:555–61.
Tseng CC, Chen SN. Long-term efficacy of half-dose photodynamic therapy on chronic central serous chorioretinopathy. Br J Ophthalmol. 2015;99:1070–7.
Lai FH, Ng DS, Bakthavatsalam M, Chan VC, Young AL, Luk FO, et al. A multicenter study on the long-term outcomes of half-dose photodynamic therapy in chronic central serous chorioretinopathy. Am J Ophthalmol. 2016;170:91–9.
Song IS, Shin YU, Lee BR. Time-periodic characteristics in the morphology of idiopathic central serous chorioretinopathy evaluated by volume scan using spectral-domain optical coherence tomography. Am J Ophthalmol. 2012;154:366–75.e4.
Hata M, Oishi A, Shimozono M, Mandai M, Nishida A, Kurimoto Y. Early changes in foveal thickness in eyes with central serous chorioretinopathy. Retina. 2013;33:296–301.
Yu J, Jiang C, Xu G. Correlations between changes in photoreceptor layer and other clinical characteristics in central serous chorioretinopathy. Retina. 2019;39:1110–6.
Moon JW, Yu HG, Kim TW, Kim HC, Chung H. Prognostic factors related to photodynamic therapy for central serous chorioretinopathy. Graefes Arch Clin Exp Ophthalmol. 2009;247:1315–23.
Guyer DR, Yannuzzi LA, Slakter JS, Sorenson JA, Ho A, Orlock D. Digital indocyanine green videoangiography of central serous chorioretinopathy. Arch Ophthalmol. 1994;112:1057–62.
Matsumoto H, Sato T, Kishi S. Outer nuclear layer thickness at the fovea determines visual outcomes in resolved central serous chorioretinopathy. Am J Ophthalmol. 2009;148:105–10.e1.
Li HK, Hubbard LD, Danis RP, Florez-Arango JF, Esquivel A, Krupinski EA. Comparison of multiple stereoscopic and monoscopic digital image formats to film for diabetic macular edema evaluation. Invest Ophthalmol Vis Sci. 2010;51:6753–61.
DeCroos FC, Toth CA, Stinnett SS, Heydary CS, Burns R, Jaffe GJ, et al. Optical coherence tomography grading reproducibility during the Comparison of Age-related Macular Degeneration Treatments Trials. Ophthalmology. 2012;119:2549–57.
Koch GG, Landis JR, Freeman JL, Freeman DH Jr, Lehnen RC. A general methodology for the analysis of experiments with repeated measurement of categorical data. Biometrics. 1977;33:133–58.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74.
Yu J, Jiang C, Wang X, Zhu L, Gu R, Xu H, et al. Macular perfusion in healthy Chinese:an optical coherence tomography angiogram study. Invest Ophthalmol Vis Sci. 2015;56:3212–7.
Chhablani JK, Kim JS, Cheng L, Kozak I, Freeman W. External limiting membrane as a predictor of visual improvement in diabetic macular edema after pars plana vitrectomy. Graefes Arch Clin Exp Ophthalmol. 2012;250:1415–20.
Yalcinbayir O, Gelisken O, Akova-Budak B, Ozkaya G, Gorkem Cevik S, Yucel AA. Correlation of spectral domain optical coherence tomography findings and visual acuity in central serous chorioretinopathy. Retina. 2014;34:705–12.
Wakabayashi T, Oshima Y, Fujimoto H, Murakami Y, Sakaguchi H, Kusaka S, et al. Foveal microstructure and visual acuity after retinal detachment repair: imaging analysis by Fourier-domain optical coherence tomography. Ophthalmology. 2009;116:519–28.
Chang YC, Lin WN, Chen KJ, Wu HJ, Lee CL, Chen CH, et al. Correlation between the dynamic postoperative visual outcome and the restoration of foveal microstructures after macular hole surgery. Am J Ophthalmol. 2015;160:100–6.e1.
Zhou C, Lin Q, Chen F. Prevalence and predictors of metamorphopsia after successful rhegmatogenous retinal detachment surgery: a cross-sectional, comparative study. Br J Ophthalmol. 2017;101:725–9.
Cook B, Lewis GP, Fisher SK, Adler R. Apoptotic photoreceptor degeneration in experimental retinal detachment. Invest Ophthalmol Vis Sci. 1995;36:990–6.
Hisatomi T, Sakamoto T, Goto Y, Yamanaka I, Oshima Y, Hata Y, et al. Critical role of photoreceptor apoptosis in functional damage after retinal detachment. Curr Eye Res. 2002;24:161–72.
Ozdemir I, Eren A, Ersöz G. Outer nuclear layer thickness at the central fovea relation with symptom duration in central serous chorioretinopathy. Int Ophthalmol. 2019;39:1323–8.
Funding
This research was supported by the Science and Technology Commission of Shanghai Municipality (grant no. 18411965100), the National Key Research and Development Plan (grant no. 2017YFC0108200) and the National Natural Science Foundation of China (grant no. 81900867).
Author information
Authors and Affiliations
Contributions
QC and CJ designed the study. XY and LL performed the photodynamic therapy. JY, XY and LL collected the data. JY, QC and CJ analysed and interpreted the data. JY was a major contributor in writing the manuscript. XY and LL participated in drafting the manuscript. QC and CJ revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
Ethics Committee of the Eye and Ear, Nose and Throat Hospital, Fudan University, Shanghai, China.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yu, J., Ye, X., Li, L. et al. Relationship between photoreceptor layer changes before half-dose photodynamic therapy and functional and anatomic outcomes in central serous chorioretinopathy. Eye 35, 1002–1010 (2021). https://doi.org/10.1038/s41433-020-1018-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-1018-6
This article is cited by
-
Evaluation of changes in macular structures after subthreshold micropulse laser therapy on chronic central serous chorioretinopathy
Lasers in Medical Science (2024)
-
Threshold thickness of foveal outer nuclear layer associated with outcomes of photodynamic therapy in central serous chorioretinopathy
Eye (2022)
-
Risk factors of persistent subretinal fluid after half-dose photodynamic therapy for treatment-naïve central serous chorioretinopathy
Graefe's Archive for Clinical and Experimental Ophthalmology (2022)