Abstract
Background/objectives
Retinopathy of prematurity (ROP) is a potentially blinding disease of immature retinal vasculature. ROP regresses in majority of the cases and very few go on to develop ROP needing treatment. Fundus fluorescein angiography (FFA) is the gold standard technique to study retinal vasculature. The present study was undertaken with the objective to identify the FFA findings associated with the progression of ROP.
Subject/methods
Prospective single centre study in a tertiary care hospital of 99 eyes of 50 preterm babies. Fundus fluorescein angiography (FFA) was performed in all babies using RetCam 3 at the first detection of ROP. The babies were followed up for the progression of ROP. The FFA predictors for the progression of ROP were evaluated using the Mann–Whitney U test and Fisher’s test.
Results
Thirty-eight eyes were Type 1 ROP at initial presentation and were lasered. Amongst the rest, 24 eyes showed features of stage 3 ROP with intense leakage on FFA and were designated as FFA-treatable ROP and were also lasered. Amongst the rest of the 37 eyes, the disease progression was seen in 13 eyes and the disease regression was seen in 24 eyes. The baseline FFA findings associated with the progression of ROP were delayed retinal arterial perfusion (p = 0.037) and popcorn lesions (p = 0.042). The post hoc analysis was done using a validated FFA scoring system.
Conclusions
FFA may be added in the classification of ROP and delayed retinal arterial perfusion and popcorn lesions on FFA may predict the progression of ROP.
Similar content being viewed by others
Introduction
Retinopathy of prematurity (ROP) is a complex vasoproliferative disease of the retina in premature infants, resulting in the abnormal proliferation of blood vessels of the retina. The introduction of newer digital wide-angle imaging systems has revolutionised fundus imaging in the paediatric population and has become a novel diagnostic modality for the evaluation of ROP [1]. The clinical examination by indirect ophthalmoscopy has been used since long as a standard method for diagnosing ROP. Early Treatment ROP study, a large multicentric trial, classifies ROP into Type 1 ROP (high-risk pre-threshold ROP needing treatment) and Type 2 ROP (low-risk pre-threshold ROP needing close observation) depending on the extent of the disease on clinical examination [2]. Type 1 ROP being a progressive disease requires treatment, while the babies with Type 2 ROP are closely followed up for the pattern of vascularisation and possible progression to Type 1 ROP [2, 3]. Approximately 15% of Type 2 ROP babies progress to develop Type 1 ROP requiring intervention and the rest of the cases regress spontaneously [4].
The current literature on fundus fluorescein angiography (FFA) in ROP has been predominantly descriptive and has diagnosed clinically unapparent areas of capillary non-perfusion (CNP) and neovascularisation [5]. The data pertaining to vascular predictors of progression of ROP is scant. We hypothesised that the details of the course of development of vessels seen on FFA in ROP eyes needing intervention vs. no intervention would help in deriving the vascular predictors of disease progression.
Methods
This is a single centre prospective intervention study of the preterm babies with diagnosed ROP at a tertiary care centre from March 2018 to December 2019 (Fig. 1). All the babies were screened for ROP by an Ophthalmologist (SN) with more than 20 years of experience in screening ROP. We excluded 11 infants who were not clinically stable (n = 4) or were on respiratory support (n = 5) or had corneal opacity (n = 1) or had abnormal renal function tests (n = 1). Fifty babies with the clinical diagnosis of ROP using indirect ophthalmoscope were eligible for the study. The study was approved by the institutional review board. FFA was performed in 99 eyes of 50 stable preterm babies by two ophthalmologists (AH and MS) in the presence of a paediatrician. The whole procedure was done under topical anaesthesia and no sedation was given to the babies. The parents were explained about the procedure and informed consent was obtained in the language best understood by them.
The image acquisition of enrolled babies was obtained using RetCam 3 (Widefield Digital Imaging System by Natus Medical, inc. 130ﹾlens). An intravenous bolus of 20% solution of sodium fluorescein dye, 0.04 ml/kg (8 mg/kg) followed by a saline flush was administered via an intravenous cannula under the care of a neonatologist. The coloured pictures were taken in the supine position using eye speculum to open the eyes and Wire Vectis for globe rotation under topical anaesthesia (proparacaine 2% contact gel). The corresponding FFA images of the posterior pole and the periphery were captured bilaterally in all the babies. The FFA images were interpreted for the stage, zone and leakage by two ophthalmologists in consensus (AH and MS), with 3 years and 5 years of experience in ophthalmology respectively. These ophthalmologists were blinded to the clinical staging at the time of evaluation of the FFA images. On the basis of the clinical examination using indirect ophthalmoscope, the babies were divided into Type 1 ROP and Type 2 ROP as described by Early Treatment Retinopathy of Prematurity study [2]. In case of any discrepancy in the clinical and FFA findings, the FFA images were reviewed by all three ophthalmologists together (SN, AH, MS) and the treatment requiring ROP was diagnosed in consensus. Those eyes with clinical diagnosis of Type 2 ROP on indirect ophthalmoscope which showed significant dye leakage and CNP areas on fluorescein angiography were classified as FFA-treatable ROP. All babies with Type 1 ROP on indirect ophthalmoscope or treatable ROP on FFA were treated using 532 nm laser. All the babies were kept under weekly follow-up to observe the course of ROP. Follow-up fundus imaging and angiography was done in babies at any sign of ROP progression on indirect ophthalmoscopy in terms of the stage of the disease and increase in dilatation and tortuosity of the vessels. The babies were lasered when there was definitive evidence of progressive disease with intense leakage from neovascularisation on FFA. Babies with Type 2 ROP showing regression were kept under follow-up till complete vascularisation of the retina. For this study, the regression of ROP was taken as resolution of vascular dilatation and downstaging of the disease and also retinal vessel growth and maturation.
Post hoc FFA scoring (0–10) was done for all the babies based on FFA scoring proposed by Barilla et al. [6]. FFA findings were scored based on the severity of leakage (absent to severe as 0–3), ischemic areas (absent to extension >2-disc diameter as 0–3), plus disease (absent to periphery, pre-plus and plus disease as 0–3), vascular abnormalities (present or absent as 0–1). The maximum FFA score in these eyes could be 10 and the minimum could be 0. The data analysis was performed using Stata 16.1 (Stata Corp, College Station, Texas, USA). Numerical data was analysed using the Mann–Whitney U test. Categorical data was analysed using Fisher’s exact test. ‘P value’ < 0.05 was considered significant. No adjustment was made for multiple testing.
Results
Out of 99 eyes of 50 preterm babies, 38 eyes of 19 babies were diagnosed clinically as Type 1 ROP at initial presentation and 61 eyes of 31 babies were diagnosed clinically as Type 2 ROP at initial presentation. None of the patients was lost to follow-up. One preterm baby had asymmetric disease showing ROP in one eye only. Therefore, only one eye of the baby was included in the study. The babies with Type 2 ROP and the babies with Type 1 ROP had a mean gestational age of 31 ± 2.7 weeks vs. 30 ± 1.9 weeks, and the mean birth weight of 1379 ± 327.6 g vs. 1295 ± 264.3 g respectively. The mean duration of ventilation in babies was significantly higher (p = 0.03) in babies with Type 1 ROP vs. babies with Type 2 ROP (6.36 ± 8.34 days and 2.12 ± 5.43 days respectively). There was no significant association of other baseline variables like respiratory distress syndrome, transient tachypnoea of newborn, pneumothorax, patent ductus arteriosus, bacterial sepsis, septic shock, jaundice, meningitis, blood transfusion or double volume exchange transfusion to the development of Type 1 ROP (Supplementary Table 1).
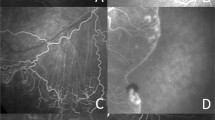
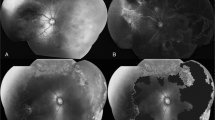
The vascular pattern in eyes with Type 1 and Type 2 ROP on FFA included tangles (21 and 11 eyes respectively), arterio-venous shunts (37 and 40 eyes respectively), cotton wool spots (8 and 3 eyes respectively), popcorn lesions (37 and 23 eyes respectively), rosary beads (20 and 7 eyes respectively), capillary tufts (10 and 9 eyes respectively), CNP areas (38 and 34 eyes respectively) and retinal haemorrhages (10 and 2 eyes respectively) (Fig. 2, Supplementary Table 2). Notably, 38 eyes had plus disease and were Type 1 ROP at presentation and were treated with 532 nm laser or anti-VEGF. Post hoc analysis showed the mean FFA score of these babies to be 6.9 ± 1.9 (range 5–9). Of the remaining 61 eyes, 24 eyes (39.3%) with a clinical diagnosis of Type 2 ROP on indirect ophthalmoscope showed significant dye leakage and CNP areas on FFA. These eyes were regarded as FFA-treatable ROP and were given laser treatment. Post hoc analysis showed the mean FFA score to be 6.2 ± 1.3 in these eyes. Total of 62 eyes were given laser treatment after FFA, including 38 eyes with a clinical diagnosis of Type 1 ROP and 24 eyes with a clinical diagnosis of Type 2 ROP as per indirect ophthalmoscope but with FFA findings of intense leakage from neovascularisation. The post hoc analysis showed that FFA score of eyes which were treated at initial presentation was significantly higher than the FFA score of eyes which finally showed regression of ROP (p = 0.013) (Table 1).
A Arterio-venous phase showing preplus disease and popcorns (red plus sign), capillary non-perfusion areas (orange arrows), arterio-venous shunt vessels (yellow arrow heads), capillary tufts (pink ovoids) and rosary beads (green circle). B FFA late phase of the same baby 2 weeks later showing leakage from the ridge area and progression of plus disease.
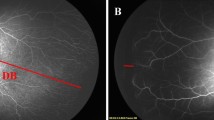
In addition to these, certain rare FFA findings in ROP included delayed retinal perfusion (three eyes), avascular island surrounded by arterio-venous shunt vessels (two eyes), saccular dilation of the arterioles giving beaded appearance (one eye) and arterio-venous shunt vessel formation in the vascularized retina with macular oedema (one eye) (Fig. 3). Zone 1 ROP was significantly associated with laser treatment (p = 0.004). There was significantly higher number of eyes with AV shunts, popcorn lesions, capillary non-perfusion areas in the eyes who required ROP treatment at initial visit than the eyes which showed regression of ROP (Table 1).
A FFA showing delayed arterio-venous filling at 1 min 40 s. The arrow demonstrates the unfilled retinal veins. B FFA arterio-venous phase showing avascular island superiorly lined by arterio-venous shunt vessels (Block black arrow). C FFA arterio-venous phase showing saccular dilatations of arterioles (seen in the white circle). D FFA arterio-venous phase showing arterio- venous shunt vessels in vascularized retina (black arrow head) and macular dye leakage suggestive of macular oedema (black arrow).
Of the 37 Type 2 ROP eyes at baseline, the progression of ROP was seen in 13 eyes (35.1%) on follow-up at a mean post-conception age of 36 ± 1.2 weeks. Of these eyes, one eye progressed to retinal detachment after laser treatment. The remaining 24 eyes with Type 2 ROP showed clinical regression of disease and were followed up till complete vascularisation of retina. For the purpose of statistical analysis for FFA predictors of progression of ROP, the babies with clinical Type 1 or FFA-treatable ROP (n = 38 + 24) at presentation were excluded and the association of baseline FFA findings with disease progression in 13 out of 37 eyes was evaluated. Progression of ROP showed significant association with the delayed retinal circulation (arm to retina circulation time) of more than 5 s (p value = 0.04) and popcorn lesions (p value = 0.04) in initial FFA (Table 2, Supplementary Fig.1).
In this study, none of the babies had an adverse effect of the fluorescein dye.
Discussion
ROP has emerged as a major health challenge in this millennium necessitating close follow-up and emergency laser of affected eyes, as and when required, to prevent blindness. Early identification of the vascular pattern in the retina of preterm neonates suffering from ROP may have a role in the early detection of the babies that are likely to require laser treatment for ROP. In the present study a large number of eyes needed treatment at the first examination. This can be explained by the fact that ours is a tertiary care centre getting referrals for ROP treatment from other hospitals of the region. The present study also shows that the larger and older babies are getting ROP as well as APROP in our set up. This is consistent with the previous studies from developing countries [7]. Various risk factors are identified in these larger babies, which lead to development of ROP [8, 9]. In the present study, the mean duration of ventilation was the significant risk factor for developing treatable ROP.
Lepore et al. have published an atlas of fluorescein angiography which documented popcorn lesions (51%), tangles (72.5%), AV shunts (37.3%), CNP areas (100%), rosary beads (17.6%), cotton wool spots (49%), capillary tufts (39.7%) and vascular abnormalities with hypo and hyperfluorescent lesions in 51 eyes of preterm babies which required treatment [5]. The FFA findings appear to be more severe in our patients than in the above study, which could be due to ethnic differences in the two populations. The birth weight and the gestational age of the babies developing ROP was also different in the two studies. In addition to these vascular abnormalities, we found saccular dilation of arterioles and abnormal avascular island surrounded by arterio-venous shunt vessels in the vascularized retina of preterm infants. Thus, FFA aided in finding newer vascular changes in premature babies with ROP which could add to the understanding of the pathogenesis and evolution of this complex disease.
Of the 61 eyes, 24 (39.3%) that were clinically diagnosed as Type 2 ROP had FFA features warranting treatment. Earlier studies have also shown that FFA not only adds to the sensitivity in the diagnosis of stage of ROP but also has the ease of interpretation even by personnel not trained in ROP management [10]. The inter-observer agreement of 79% for the Retcam coloured images improved to 85% for the Retcam FFA pictures in another study [11]. FFA enables easy visualisation of the retinal vasculature, which may not be clearly visible by indirect ophthalmoscope and helps in the accurate staging of the disease. Azad et al. conducted FFA after 2–3 weeks in preterm infants who were treated with laser and noted clinically unidentified skip laser areas in the periphery requiring additional session of laser treatment [12]. We also detected many cases on FFA which needed laser treatment despite the clinical diagnosis of Type 2 ROP. In the present study on post-hoc analysis, using Barilla’s scoring, the maximum FFA score in these eyes was 10 and the minimum was 4. Barilla et al. showed that all eyes with score ≥7 were lasered within 6 days and those with a score of 5–6 were lasered by 19 days [6].
It has been found that ~15% of babies with Type 2 ROP progress to develop Type 1 ROP requiring treatment within 7 days and the rest regress and do not require any treatment [3]. We identified progression of Type 2 ROP to Type 1 ROP in 13 out of 37 eyes (33.3%) wherein laser treatment was required. One of these eyes of Type 1 ROP progressed to stage 4b ROP after laser treatment. Previously in a study, FFA was conducted in 13 preterm infants [13]. The authors found that arterio-venous shunts, surrounded by areas of CNP, rosary-bead-like hyperfluorescence, tortuosity and leakage from distal arterioles were seen in two babies who later on developed treatable ROP. They concluded that FFA can help examiners to identify vascular changes that are not detectable by indirect ophthalmoscopy, which could predict the progression to threshold disease, and provide an alert about the need for therapeutic interventions. Delayed arm to retina circulation time and popcorn lesions were the significant predictors of the progression of Type 2 ROP to treatable Type 1 ROP in our cohort of patients. Popcorn lesions are well known to be related to neovascularisation, so their association with progression of ROP to Type 1 ROP is not surprising [14].
The time of dye appearance in newborns is variable. We hypothesise that delayed arm to retina circulation time could be associated with ischaemia, further leading to increase in VEGF levels and progression to treatable ROP. In the present study, only three babies had delayed perfusion and all these babies progressed to treatable ROP. These findings need further validation in larger studies.
Limitations
The main limitation of our study is that it is a single centre study. Moreover, the FFA images were evaluated in consensus and inter-grader as well intra-grader variability for the images was not assessed. There could be a bias in treating Type 2 clinical ROP with laser, based on FFA findings which needs to be addressed by a large randomised controlled multi-institutional blinded prospective trial. The present study included only infants with a stable neonatal course, the results may not be generalisable to other cases which includes infants with a more unstable clinical course.
Conclusion
Advances in imaging have transformed the understanding of vascular changes in paediatric disease including ROP. Techniques such as FFA could play a pivotal role in understanding the vascular pathology and guiding in prompt management of the disease. FFA scores may help us to identify treatable ROP. By using FFA, we have highlighted the increase in accuracy for diagnosing treatable ROP. The vascular abnormalities like prolonged arm to retina circulation time and popcorn lesions could be predictors of progression of ROP to treatable ROP.
Summary
What was known before
-
FFA adds to the sensitivity of diagnosing the stage of ROP.
What this study adds
-
For the first time, FFA has been used to predict the progression of ROP. FFA is a safe modality to be done in preterm babies and popcorn lesions and delayed arm to retina circulation time could predict the progression of ROP.
References
Temkar S, Azad SV, Chawla R, Damodaran S, Garg G, Regani H, et al. Ultra-widefield fundus fluorescein angiography in pediatric retinal vascular diseases. Indian J Ophthal. 2019;67:788–94.
Early Treatment for Retinopathy of Prematurity Cooperative Group. Revised indications for the treatment of retinopathy of prematurity: results of the early treatment for retinopathy of prematurity randomized trial. Arch Ophthalmol. 2003;121:1684–94.
International Committee for Classification of Retinopathy of Prematurity. The international classification of retinopathy of prematurity revisited. Arch Ophthalmol. 2005;123:991–9.
Christiansen SP, Dobson V, Quinn GE, Good WV, Tung B, Hardy RJ, et al. Progression of type 2 to type 1 retinopathy of prematurity in the Early Treatment for retinopathy of prematurity study. Arch Ophthalmol. 2010;128:461–5.
Lepore D, Molle F, Pagliara MM, Baldascino A, Angora C, Sammartino M, et al. Atlas of fluorescein angiographic findings in eyes undergoing laser for retinopathy of prematurity. Ophthalmology. 2011;118:168–75.
Barilla D, Guagliano R, Bertone C, Maffia A, Bruttini C, Periti F, et al. Screening and follow-up of acute ROP: reproducibility of fluorescein angiography. Adv Ther. 2020;37:860–8.
Kumawat D, Sachan A, Shah P, Chawla R, Chandra P. Aggressive posterior retinopathy of prematurity: a review on current understanding. Eye. 2021;35:1140–58.
Gilbert C. Retinopathy of prematurity-′the second lull′? Br J Ophthalmol. 2001;85:1017–9.
Dutta S, Narang S, Narang A, Dogra MR, Gupta A. Risk factors of threshold retinopathy of prematurity. Indian Pediatr. 2004;41:665–71.
Klufas MA, Patel SN, Ryan MC, Gupta MP, Jonas KE, Ostmo S, et al. Influence of fluorescein angiography on the diagnosis and management of retinopathy of prematurity. Ophthalmology. 2015;122:1601–8.
Guagliano R, Barillà D, Bertone C, Maffia A, Periti F, Spallone L, et al. Fluorescein angiography-based diagnosis for retinopathy of prematurity: expert-non expert comparison. Eur J Ophthalmol. 2013;23:881–6.
Azad R, Chandra P, Khan MA, Darswal A. Role of intravenous fluorescein angiography in early detection and regression of retinopathy of prematurity. J Pediatr Ophthalmol Strabismus. 2008;45:36–9.
Purcaro V, Baldascino A, Papacci P, Giannantonio C, Molisso A, Molle F, et al. Fluorescein angiography and retinal vascular development in premature infants. J Matern Fetal Neonatal Med. 2012;25:53–6.
Wallace DK, Kylstra JA, Greenman DB, Freedman SF. Significance of isolated neovascular tufts (“popcorn”) in retinopathy of prematurity. JAAPOS. 1998;2:52–6.
Acknowledgements
Dr Meba, MD Paediatrics for her help for paediatric monitoring.
Author information
Authors and Affiliations
Contributions
AH was responsible for collecting clinical data and analysing FFA images and writing the report; SN was responsible for designing the protocol, screening the babies with ROP, analysing FFA and editing the report; MS was responsible for doing FFA and analysing the FFA images; SJ was involved in paediatric monitoring of the babies during FFA, DC did the statistical analysis and interpreted the results and also did paediatric monitoring during FFA.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Hans, A., Narang, S., Sindhu, M. et al. Fundus fluorescein angiography in retinopathy of prematurity. Eye 36, 1604–1609 (2022). https://doi.org/10.1038/s41433-021-01694-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01694-9